View sample waterborne diseases research paper. Browse research paper examples for more inspiration. If you need a health research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Introduction: Magnitude Of The Problem, Overview, And Definitions
Water is essential to human life, to agriculture and animal husbandry, and to modern industrial society. The absence of water precludes human existence. People must have adequate amounts of water as well as access to water of sufficient quality that it does not harm them when drunk. Re-use of water is common, and through this mechanism human pathogens (of animal, human, or environmental origin) can be introduced into water that may be used multiple times between the time it falls from the sky and it enters the sea. Some waterborne pathogens do not survive for long periods of time in water, or when diluted into large bodies of water fail to achieve a minimal concentration of organisms likely to cause infection (‘the infectious dose’). Others are well adapted to survival in fresh or brackish waters. Well over 400 organisms have been documented to cause waterborne disease, so that in this research paper we focus on key principles of transmission and prevention, while mentioning important specific diseases as needed.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
Waterborne diseases, as a group, contain some of the most important illnesses known to humans, such as typhoid fever (enteric fever), rotavirus diarrhea, and the pandemic disease cholera. Each of these currently, or historically, has been a leading human cause of death. Diarrheal diseases remain a leading cause of death in children globally. While most deaths from diarrhea occur in poor countries, the risk for waterborne disease outbreaks remains a constant threat even in the richer nations should the barriers to disease, sanitation, and water treatment be compromised. There are many examples of modern water treatment failures in the ‘developed’ countries resulting in epidemics of waterborne disease such as gastroenteritis or hepatitis. While waterborne diseases have their greatest impact on children, they are fully capable of causing significant death and morbidity in adult populations. For example, when cholera was re-introduced into South America in the early 1990s, many adults died, shocking the sensibilities of societies where child, but not adult, deaths were common.
Recent authoritative World Health Organization (WHO, 2006) estimates are that unsafe water and a lack of basic sanitation led to at least 1.6 million deaths in children under the age of 5 years in 2004. An estimated 1.8 million deaths, including adults, from diarrheal diseases occur every year. Recent estimates (Pruss-U stun and Corvala´n, 2006) are that at least 88% of diarrheal episodes globally are attributable to poor water, sanitation, and hygiene. Thus, for the purposes of understanding the public health importance of waterborne diseases, a focus on prevention via the provision of these services is obvious.
Approximately 1.1 billion people do not have access to an ‘improved’ source of drinking water, and more than 2 billion people in 2004 ‘‘did not have access to basic sanitation facilities’’ (Pruss-Ustu n and Corvalan, 2006).
The challenge of eliminating waterborne disease, especially for poor and rural populations, is thus immense. An improved water supply can be as simple as a borehole well, a public water pipe shared by a community, a protected well or spring, or collected rain water. None of these ‘improved’ water supplies would meet modern criteria for potable water in the richer nations, yet they represent substantial improvements over open surface water sources as they lower the risk of waterborne disease.
In the approximately 40 countries where 90% of all childhood deaths occur, the major causes of death are diarrhea, pneumonia, malaria, and neonatal disorders. Clean water is important not only for drinking water, but also because it allows related hygienic practices, such as hand washing, to be effective. Recent studies from Pakistan and elsewhere have shown that hand washing with soap decreases not only diarrheal episodes by over 50%, but also pneumonia episodes by a similar proportion (Luby et al., 2005). Measures that eliminate the classically recognized waterborne diseases such as diarrhea are thus likely to have important effects on other communicable diseases such as viral respiratory infections and trachoma. Indeed, 100 years ago, there was a widespread recognition in the public health community that for every case of typhoid prevented by water treatment or sanitation, somewhere between three and ten other deaths could be prevented (the Mills-Reincke phenomenon; see discussion on historical data).
Bacterial pathogens such as Salmonella, Shigella, Escherichia coli, and Campylobacter cause much of the burden of waterborne disease. Other high-impact human diseases (viral, bacterial, and parasitic), such as hepatitis A, amebiasis, caliciviruses, leptospirosis, polio, and the other enteroviruses, schistosomiasis, giardiasis, and cryptosporidiosis, are also waterborne. These diseases share the common characteristics of water acting as a vector or vehicle for transporting pathogens from other humans, other animals, or the environment to new humans who, once infected by the contaminated water, usually act as a source of infection for others. Water can also act as the site for multiplication of a waterborne disease, such as for schistosomiasis, where the parasite obligatorily multiplies in water-associated snails before it can infect humans. In this research paper we separate waterborne diseases from ones where a vector of disease requires water but the pathogen does not, such as mosquitoes that transmit malaria. It should be noted, however, that these two are related, since the creation of an impoundment or reservoir for improving drinking water quality can provide new habitats for vectors of disease.
Some authors divide water-related infections into ‘waterborne’ (the pathogen is ingested, such as typhoid or cholera), ‘water-washed’ or ‘water-scarce’ (person-to-person transmission because of a lack of water for hygiene), ‘water-based’ (transmission via an aquatic intermediate host, such as schistosomiasis), and ‘water-related insect vector’ (with transmission by insects that breed in, or bite near, water). These distinctions are useful intellectual constructs, but in practice the divisions are sometimes less clear, as explained later in the paper. Indeed, reservoir construction is associated with increasing incidences of both malaria and schistosomiasis, of which only the latter is classically waterborne.
Waterborne diseases are intimately linked not only to the ingestion of, or exposure to, water, but also to how human and animal feces are separated from water and food supplies (sanitation), and to the availability of clean water for hand washing and bodily cleansing (hygiene). Fecal pathogens frequently, through inadequate or absent sewerage, enter surface waters (rivers, lakes, and recreational pools) or groundwaters (accessed through wells and boreholes) to infect new hosts. Examples of these include pathogens such as cholera bacteria, viruses, and Giardia cysts. Human urine and feces can also contain schistosome eggs or other parasites, such as the cysts of Entamoeba histolytica, the agent of human amebiasis. Human excrement can contaminate hands, food, and environmental surfaces, as well as soil. Thus, a disease that enters a population through water can then spread through other routes, via person-to-person transmission, or through contamination of crops by wastewater. Similarly, a disease that first spreads by person-to-person contact may then enter water supplies through the fecal stream, and then become waterborne. When considering waterborne diseases, an ecological perspective is often useful in understanding the complex web of relationships that exist between humans and these diseases. One obvious reason why the control of waterborne diseases is so important is that it can also decrease the likelihood of subsequent person-to-person or foodborne transmission.
Some waterborne diseases, such as the parasitic infections schistosomiasis and dracunculiasis, require that humans have direct skin-in-water (dermal) contact with water bodies where the infectious forms of the parasites dwell (‘water-based’ transmission). Globally, much of this contact is due to the need of individuals to collect water for household use, to engage in agricultural activities, and for recreational bathing or swimming. Thus, there is also merit in understanding that waterborne diseases are affected by not only the quality of water, but also by human behaviors and the local infrastructure. For example, the provision of piped water or wells (forms of infrastructure) in communities may alleviate the need for children and others to collect water by hand from infectious rivers or surface waters, but it is unlikely to affect the natural desire of small children in a hot climate to play in contaminated water (forms of behavior).
Water Needs: As Supply Increases, Health Hazards Decrease
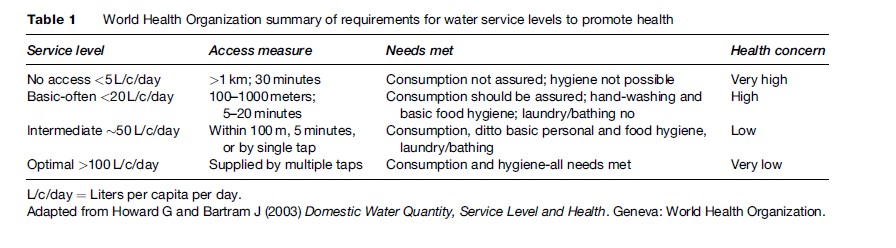
Depending on factors such as age, level of physical activity, and the need to produce breast milk, minimal daily water needs range from between 1 and 3 liters (L) for hydration; perhaps as little as 2 to 3 L for food preparation; 6 to 7 L for personal hygiene; and 4 to 6 L for laundry. The World Health Organization (WHO) has published estimates that minimal water needs are approximately 7.5 to 10 L per person per day. As access to quantities of water increases, the public health risks decrease (see Table 1). When water is scarce, then people are forced to drink unsafe water, and there is no water for hygiene, or to carry feces away. By way of comparison, many city dwellers in rich countries use 200 to 300 L of water per day for consumption, sanitation, and cooking, as well as ancillary uses such as watering lawns or washing vehicles. These ancillary uses of water are not as critical as drinking water, but it should be mentioned since historically much of the civic impetus to the provision of piped water was the need to have water to fight fires.
Sources Of Waterborne Diseases: Water Types, Sanitation, And Risk Of Waterborne Diseases
Water for drinking, cooking, and hygiene purposes is generally divided into surface waters and groundwaters. Surface waters include lakes, rivers, reservoirs, ponds, and streams. They are easily contaminated with pathogens, and thus treatment of surface waters is important when one considers the prevention of this group of diseases. Surface waters that are small, such as ponds, may evaporate during dry seasons, and it is common for people who use seasonally affected surface waters to utilize multiple sources over the course of a year.
Groundwaters are usually thought of as being ‘shallow’ or ‘deep,’ with the former easily contaminated and the latter difficult to contaminate. Shallow wells and natural springs tap into the upper aquifer table found in soil, which fluctuates in depth by season. A spring is simply a place where the water table and the surface intersect. Shallow wells are typically hand dug, and springs are usually found on hillsides. Protecting shallow wells from waterborne pathogen contamination can be accomplished by simple walls around the top of the well, and sculpting the surrounding ground so that contaminated rainwater runs away, rather than toward, the well. Well covers keep small animals or children from falling in. Ideally, the water should be pumped up by hand or electrical devices rather than through the use of buckets, since the buckets can serve as a route of contamination. Springs can be protected with an enclosing house or box, and water should be taken downstream of the spring source.
Deep wells, popularly known as boreholes, access deep aquifers that are usually below impermeable rock. This renders the water much safer, but deep borehole water may be less amenable to recharge from the surface. Boreholes are costly to drill, and the well must be cased where it traverses the upper soil levels to prevent upper, contaminated shallow water from contaminating the safer, deeper water. Furthermore, the depth of these wells requires the use of electric pumps when water is withdrawn.
Rainwater is often collected from roofs and stored for use in dry seasons. This water may be contaminated by bird and animal feces, leaves, and soil. Both sand filtration and flushing tanks are used to decrease contamination. Flushing tanks divert the initial flush of water during a rainstorm, as it is assumed that most of the contaminating substances are rinsed off in the initial rainfall. Outbreaks of E. coli, Salmonella, and Cryptosporidium, among other pathogens, have been linked to the use of untreated rainwater.
Sanitation can be defined as the methods for dealing with human wastes such as feces and urine, and the principles can also be applied to animal wastes that contain pathogens that can cause human waterborne disease. Sanitation not only prevents waterborne diseases, but also reduces the transmission of helminth infections such as hookworm, Trichuris, and Ascaris, which require fecal contamination of soil. The simplest form of sanitation is the latrine, a pit covered with a robust cover. Latrines do not use any water for waste transport, but act primarily as a storage space (although they can easily be cleaned out to extend their usable lifetime). Waterborne pathogen contamination of the surrounding soil, and shallow groundwater, can occur, especially if the soil is sandy and porous. The bottoms of latrines should not come closer than approximately 0.6 meters to the top of the wet-season water table to prevent contamination of nearby springs and shallow wells. Where water tables are high, latrines can be lined with impermeable stone or concrete.
The ventilated, improved pit (‘VIP’) latrine has solid walls with no windows, and has a tight roof with a screened ventilation pipe in it. The entryway is sited downwind of the prevailing winds improving ventilation, and flies are drawn to the screen where, unable to escape, they die. Thus, the VIP latrine has fewer aesthetic detractions than the unimproved pit latrines, but in many societies it is considered unacceptable to defecate indoors, pointing out the importance of behavioral factors in waterborne diseases and in particular population acceptance. Community involvement in planning sanitation systems is critical to their success or failure.
Water can be used to flush wastes into larger underground cesspools, which will increase the risk of groundwater contamination. Septic systems allow solids to settle in a central tank and have effluent, perforated pipes to distribute liquids into the surrounding ground. Alternately, wastes can be flushed with water via gravity into piped sewerage systems and then centrally disposed of. This method is by far the preferred one in areas of high population density Treatment of piped sewerage waste is via settling (primary treatment), biological degradation (secondary treatment), and disinfection (tertiary treatment). Human wastes treated through these methods have dramatically lower levels of waterborne pathogens and can even be used as crop fertilizers. Biological treatment, through the use of lagoons or wetlands with nutrient-absorbing plants, requires little maintenance and has great promise in the appropriate climates.
Historical Elements: What We Have Known And Forgotten About The Benefits From Decreasing Waterborne Diseases
At The Dawn Of Waterborne Disease Prevention
The value of clean drinking water, and of sanitation, was evident to the human population even before the germ theory was widely accepted. Waterborne diseases are most common when drinking waters are contaminated by animal and particularly human feces; this was recognized to one extent or another before our scientific capacity to identify specific pathogens was developed (see water’s roles in transmission, discussed earlier). Before water treatment technologies such as filtration and chlorination were widely adopted, many municipalities in richer countries focused on securing protected water supplies for future generations, free of obvious contaminants, during the period of 1850 to 1900. In the absence of protected water supplies, communities sought water as free as possible from human or animal feces. This principle of watershed protection remains a critical one even today. The economics, logistics, and health risks relating to waterborne diseases are profoundly different for communities with pristine source water supplies versus those with heavily polluted, pathogen-loaded waters. In practice, cities along rivers, without access to clean water, should at a minimum try to obtain their drinking water from less contaminated sites along the river, or build aqueducts or pipes to carry water from more pristine sites.
When John Snow famously removed the Broad Street pump in 1854 in the City of London during a cholera outbreak, he did so because he realized that that specific pump supplied water to a group of people with a high risk of death from cholera, which he believed to be caused by a germ transmitted by unclean water (others believed it was caused by poor hygiene or atmospheric conditions). He did not use modern statistical methods to prove the connection, but rather made a reasonable conclusion based on the state of knowledge at the time. Indeed, the then novel theory that waterborne disease was caused by pathogens – bacteria, viruses, parasites – was unproven and widely disavowed. John Snow was able to calculate that the number of deaths from cholera in the population served by the Southwark & Vauxhall Company was 315 per 10 000, versus 37 per 10 000 for people served by the Lambeth Company, whose source of water was upstream of London. In retrospect, we can recognize that human sewage, containing cholera bacteria, entered the Thames River in London above the water intake for the Southwark & Vauxhall water supply, which in turn supplied the Broad Street pump.
From The 1850s Through The Sanitary Period: Stockholm And Chicago
It is instructive to examine the documented experiences of rich nations that were once poor. For example, the infant mortality rate in Stockholm, Sweden, in 1878 exceeded 20% (200 per 1000 infants per year) but declined to 50 per 1000 in 1925, with most of the decrease due to a near abolition of deaths from diarrheal disease (Burstro¨m et al., 2005). After the 1853 cholera epidemic in Stockholm, a sanitation office was established to remove and manage human and animal feces. Wastewater flowed in open ditches, and was only occasionally covered by stones or wooden planks, as is common in many poorer countries today. Regulations for the control of wastes through the construction of sewers, and separation from water sources, were promulgated in Sweden during the 1870s and 1890s.
During this same period, the population obtained its drinking water from open surface waters and wells of varying quality. This circumstance is also identical to the current situation of many communities in poorer countries. After 1860, piped water was incrementally introduced to provide water for firefighting, to improve hygiene, to ‘reduce the risk of epidemics,’ and to allow industry better access to water. Initially, water posts were provided throughout the city where water was provided free of charge, and with time, water pipes were extended to dwellings, streets, squares, and courtyards. By 1896 about half of apartment dwellers had piped water in their buildings, and a third had water taps in courtyards. Only 14% had no access to piped water. Outdoor and indoor privies numbered perhaps 60 000 in 1880, and by 1900, approximately 75% of families had private privies with only 3% having to share facilities with more than one family. Subsequently, the proportion of indoor facilities tied to sewers increased and outdoor privies decreased.
The decrements in diarrheal mortality during this period were enormous. During the period 1918 to 1925, the diarrhea mortality rate in children under the age of 2 years had fallen to a rate of only 2 per 1000, down from 59 per 1000 in 1878 to 1882. Of no small importance is the fact that the differential death rates from diarrhea between rich and poor children essentially disappeared. In 1878 to 1882, the mortality rate per 1000 children under 2 years of age in the wealthiest group was approximately 38, while for the poorest it was about 85, with a relative risk of death from diarrhea for the poorest, compared with the wealthiest, of approximately 2.2. By 1918 to 1925, the overall diarrhea mortality rate had fallen to about 2 per 10 000, and the relative risk for the poor, compared with the wealthy, was only 1.3.
To summarize this experience, the provision of sanitation occurred before clean drinking water provision or water treatment with filtration or chlorination with major decreases in the incidence of waterborne diseases, and it led to the virtual elimination of deaths from diarrhea in children. It allowed the demographic transition to occur, and it provided an element of what we would now term environmental justice, since these measures improved the health of all citizens, and not just the wealthy.
Similar impressive reductions in mortality have been documented for the period from 1850 to 1925 for Chicago, Illinois, in the United States (Ferrie and Troesken, 2008). Mortality rates dropped by 60% during this period, with an estimated 30 to 50% of this decrement directly attributable to water purification and sanitation. Using typhoid as a marker of waterborne disease, three events were important: (1) around 1870, placing the intake for Chicago’s drinking water 2 miles away from the polluted Lake Michigan shoreline, and reversing the flow of a heavily polluted river that dumped sewage into Lake Michigan; (2) around 1893, improving water intake sites, and the permanent closure of all shoreline sewage outlets that might pollute the drinking water inlet sites in Lake Michigan; and (3) in 1917, citywide chlorination of centrally piped water. Again, it appears that sanitary improvements that preceded the onset of water treatment had the greatest effect on decreasing mortality from waterborne diseases.
The Mills-Reincke Phenomenon
Coincident with impressive decreases in waterborne disease mortality in the rich countries were equally impressive decreases in the death rates from all diseases, which correlate to the timing of these waterborne disease prevention efforts. This effect has been ascribed to ‘diffuse’ positive impacts on human health, and in the case of Chicago, an elegant statistical analysis suggests that for each death from typhoid that was prevented, an additional 4 to 5 deaths from other causes were prevented as well. Hiram F. Mills and J. J. Reincke, in the late 1880s and 1890s, independently working in Lawrence, Massachusetts, and in Hamburg, Germany (respectively), documented dramatic changes in nontyphoidal death rates that followed the initiation of water filtration in each city in 1893. This included deaths from pneumonia, influenza, heart disease, and tuberculosis, none of which are classically considered waterborne. Hazen in 1907 and Sedgwick and colleagues in 1910, along with others in the following decade, repeatedly documented the existence of the Mills-Reincke phenomenon after analyzing data from multiple large and small U.S. cities, and U.S. Army bases.
In deciphering the events of a century ago, we cannot be perfectly sure that we fully understand the reasons for this extraordinary effect, but the reality of the effect is not in doubt. It is likely that this general benefit was mediated, in large part, through decreases in childhood diarrheal diseases of all kinds, as well as through decreased mortality in people who were no longer weakened and made frail by having had typhoid. Beyond these effects, since diarrheal diseases are known to have a negative impact on nutritional status, it is possible that the elimination of waterborne diseases leads to fewer deaths from diseases worsened by malnutrition, such as pneumonia. This now nearly forgotten, well-documented history supports the thesis that improving water quality, sanitation, and hygiene for the purpose of preventing waterborne disease may have very substantial, while difficult to directly link, benefits in countries currently undergoing the sanitary and mortality transitions that rich countries have already undergone.
Modern Evidence Of The Benefits Of Preventing Waterborne Diseases
At least three lines of evidence from the current era speak to the importance of preventing waterborne disease. They include our experience with outbreaks of disease when prevention fails; studies showing benefits after interventions in the recent past; and emerging information about the negative effects of having had waterborne diseases.
The elimination of waterborne diseases required, as it requires today, political commitment, the enforcement of regulations and the implementation of public health policies, attention to both water sources and wastewater, properly trained labor, and adequate capital. When these are absent, because of inattention, war, or calamity, outbreaks of waterborne disease occur. Examples of these are numerous. In the 1990s, in Tajikistan, a shortage of funds for chlorination of water led to an outbreak of typhoid in the capital Dushambe, which was halted as soon as chlorination was restored. In Ontario, Canada, the town of Walkerton suffered an outbreak of dysentery and diarrhea caused by animal feces making their way into well water that was erratically treated with chlorine. In a town of approximately 5000 people, more than 2000 became ill, with some deaths. The city of Milwaukee was the site of the largest waterborne disease outbreak in the history of the United States in 1993. Over 400 000 people developed diarrhea when Cryptosporidium parasites (originating in wastewaters) found their way into the drinking water supply due to a filtration plant failure. In each of these cases (and there are countless more), the medical, economic, and social costs were enormous.
Although some have argued that economic development is enough to explain the decreases in mortality that rich nations have enjoyed, the weight of evidence is that specific, targeted public health efforts focused on drinking water, sanitation, and hygiene promotion are required to produce these dramatic improvements in human health. The elimination of waterborne diseases is likely to decrease the disparities between rich and poor, as was seen a century ago in Sweden, and to lead to major decreases in all-cause mortality, through well-understood, direct effects as well as poorly understood ones. Two positive, modern examples, from the United States and from Malaysia, can be cited to illustrate these points.
In the United States, many of the aboriginal peoples present before colonization by Europeans live on ‘Indian’ reservations, and they represent the poorest ethnic group in the country. In 1952, most peoples living on these reservations carried water for household use and drank from contaminated sites. Beginning in 1960, about 3700 sanitation projects were implemented on these Native American reservations (Watson, 2006). These efforts sharply reduced the cost of clean water, the incidence of waterborne gastrointestinal diseases, and infectious respiratory illness in infants. These benefits became evident 2 to 7 years after the infrastructure projects were begun. In 1960, the infant mortality rate on U.S. Indian reservations was 53 per 1000, whereas for ethnically white U.S. residents, it was 26 per 1000. By 1998, the rates were 9 and 6 per 1000, respectively, and the author of one study has ascribed approximately 40% of this improvement to water and sanitation. This speaks to the importance of targeted interventions, and to issues of social equity. In Sarawak, Malaysia, water supply and sanitation intervention during the period 1963 to 2002 led to a 200-fold and a 60-fold decrease in the incidence of dysentery and enteric fever (typhoid), respectively (Liew and Lepesteur, 2006). In this Malaysian effort, communities had to invest in basic sanitation (pit or improved latrines) before the government would invest in piped (not necessarily disinfected) water to the community. These remarkable decrements in the incidence of waterborne disease were progressive, and directly related to the percentage of the population with both sanitation and piped water. Hepatitis A also markedly decreased as water supply coverage increased. This, again, speaks to the importance of targeted interventions to prevent waterborne diseases. Of note, epidemics of cholera still occur in Sarawak, demonstrating that waterborne disease epidemics can still occur when drinking water is contaminated and not disinfected.
A third line of evidence speaking to the importance of preventing waterborne diseases is emerging that revolves around malnutrition. As intimated in the discussion of the Mills-Reincke phenomenon, one benefit in the prevention of waterborne diseases may be a decrease in malnutrition, which is an important cofactor in many infectious diseases. In a recent retrospective study of 25 483 children prospectively enrolled in a 1988 vitamin A study in Sudan (Merchant et al., 2003), it was found that the risk of stunting was lowest in households with both household water and sanitation facilities, and highest in households that lacked them. Risks were intermediate for children in households with sanitation, or with household water, but not both. Furthermore, during the course of the study, children in households with both water and sanitation who were stunted when the study commenced had a 17% higher chance of reversing their stunting than did children in households with neither barrier to waterborne diseases. Data consistent with a protective effect of clean water and sanitation against malnutrition have also been acquired from Lesotho, Nigeria, and the Philippines. Malnutrition has been linked not only to increased morbidity and mortality from infectious diseases, but also to cognitive impairment and lower socioeconomic achievement. There is excellent evidence that children who suffer from specific waterborne diseases such as shigellosis, cryptosporidiosis, and giardiasis are more likely to be stunted, and to have poorer educational performance, suggesting lifelong negative nutritional and socioeconomic impacts above and beyond the medical effects.
What, then, can be stated about the health benefits of sanitation and water? It can be confidently said that their provision can have profound, though sometimes not fully understood, positive effects on decreasing disease, on improving nutritional status, and on individual development.
Problems With Understanding The Full Range Of Waterborne Pathogens
Etiologic agents of waterborne disease include viruses, bacteria, fungi, helminths, trematodes, and protozoa, as well as cyanobacteria. Prions are not believed to be agents of waterborne disease. Our understanding of the agents of waterborne diseases is informed by over 100 years of bacteriology and microbiology, but paradoxically remains limited. For a waterborne disease to be recognized, it must, in general, be detectable in human samples such as feces, or be so well recognized that a serological test exists, such as those for hepatitis A. Many bacteria, such as the agents of cholera and other acute watery diarrheas, and of dysentery, are easily isolated using bacterial culture media. Other agents of diarrhea are fastidious, rarely tested for, or (likely) unknown. For example, many obligate parasitic and viral pathogens do not grow on culture media, but rather only in people or other hosts. Their detection requires sophisticated, often costly and therefore unavailable, technologies. Thus, the problem with waterborne diseases is that disease pathogens are only tested for if they are already known to exist and can be tested by using inexpensive methods. Novel pathogens will only be recognized if public health authorities or scientific researchers devote resources to devising methods for the detection of new agents, and if the testing method is inexpensive enough for widespread use. For example, the burden of many viral waterborne pathogens was previously greatly underappreciated, because of the lack of methods for detecting them other than electron microscopy.
However, reasons for the continued recognition of new waterborne pathogens go well beyond simply increased technological capacities to detect pathogens.
These factors include the development of human subpopulations who are at times exquisitely sensitive to specific pathogens, such as people with HIV/AIDS or those on immunosuppressive therapies, such as following transplantation or during chemotherapy for cancer. Another potential reason is the development of concentrated animal husbandry with industrial levels of manure production where emerging zoonotic pathogens (originating in animals but capable of infecting humans) are present in urine and feces, and can contaminate water supplies. In addition, inherent properties of the emerging pathogens may render them relatively or absolutely resistant to water treatment technologies. These include the presence of a waxy cell wall (Mycobacteria) or cyst wall (Cryptosporidium, Giardia) resistant to chlorination, or the presence of pathogen enzymes that can repair sections of doublestranded DNA damaged by ultraviolet light disinfection (using as a template the nondamaged strand) such as are found in adenoviruses. In addition, as water treatment technologies change, an untoward effect may be the abandonment of a technology that was effective against a pathogen.
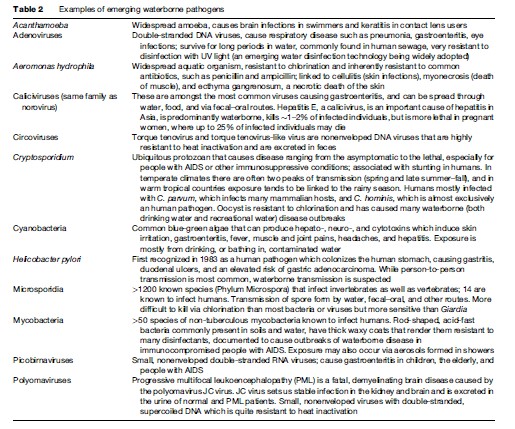
Two important waterborne pathogens prove these points. As the AIDS pandemic began and spread, a disease informally named ‘slim’ or wasting disease was recognized, characterized by persistent diarrhea and wasting. The most important causes of this syndrome are Cryptosporidium species and Microsporidia, neither or which were recognized as causing human disease before the HIV/AIDS era. In the Milwaukee (USA) epidemic of cryptosporidiosis in 1993, more than 400 000 people became ill, but only 12 people were diagnosed with Cryptosporidium infection during the epidemic, because this organism was rarely if ever tested for. The Microsporidia were once thought to be protozoa, but are now believed to be fungi, as they contain chitin in their cell walls and have strong genetic similarities to other fungi. Although more than 1200 species of Microsporidia infect invertebrate and vertebrate hosts, only 14 are known to infect human hosts. Waterborne transmission has been consistently identified in epidemiological studies, as well as fecal–oral, oral–oral, inhalation of aerosols, and foodborne transmission routes. Characteristics of Microsporidia that favor waterborne transmission include the ability to infect a wide variety of mammals, excretion in urine and feces, extended survival of the spores in water, a low infectious dose, and a small enough size (1–3 mm 1.5– 4 mm) that removal by water filtration is difficult. These characteristics are identical to those for Cryptosporidium species, which are approximately 5 mm in diameter. A list of potential important waterborne disease agents is provided in Table 2.
Indeed, the U.S. National Academy of Sciences recently described the obstacles to accurately estimating the burden of waterborne diseases in the United States, and these limitations are likely global. One critical issue is that when a case of waterborne disease occurs, the individual affected has likely had multiple possible exposures to food, water, and other individuals (person-to-person spread). The illness cannot be ascribed to water unless the individual is part of an epidemiological monitoring program (surveillance) or epidemiological study. Undoubtedly many cases of illness ascribed to food or water are misclassified – or not classified – as to the origin of the illness. Our ability to estimate the global burden of waterborne diseases is limited by the realities: (1) that endemic waterborne diseases are unrecognized unless an epidemic occurs; (2) that the public health infrastructure must be capable of recognizing an epidemic; and (3) that inexpensive, widely available tools must be available to identify the pathogen(s) involved. Without these, the incidence of waterborne diseases will be underestimated. Much evidence suggests that endemic waterborne disease is common; it is a reality that national and international surveillance for waterborne disease is woefully underfunded; and that our capacity to identify pathogens is not only overwhelmingly limited to rich nations, but that within those countries it is still limited by the capacities of reference laboratories.
Treatment Of Waterborne Diseases: Overview
The treatment of waterborne diarrheal diseases was essentially revolutionized by the development, and implementation, of oral rehydration therapy (ORT). Most deaths due to diarrheal disease are due to dehydration, and so greatly decreasing the frequency of dehydration has led to a decrease in deaths from perhaps 5 to 10 million deaths a year to current levels of 1.5 to 2 million deaths per year. While ORT has dramatically decreased mortality from acute, watery diarrhea, it has not had any significant effect on the incidence of waterborne disease, which is estimated to be (for diarrheal disease alone) more than 4 billion cases per year. Indeed, as deaths from acute, watery diarrhea (such as cholera and rotavirus diarrhea) have declined, there has been an increased appreciation for the human burden of dysentery (bloody diarrhea, often caused by Shigella) and of persistent diarrhea (diarrhea for 14 or more days), especially in malnourished and immunocompromised populations. These problems are much more difficult to address. Compounding the importance of these diseases has been the development of antibiotic resistance by many bacterial pathogens that cause dysentery; the appreciation of new, emerging pathogens; and the lack of antiretroviral treatment for people with HIV/AIDS in most of the world. For many important waterborne diseases, such as hepatitis A, no specific treatment exists, and there are only supportive and preventive measures. These circumstances have once again renewed interest in the prevention of waterborne diseases through the provision of potable water, hygiene promotion, and sanitation globally.
Prevention
As outlined earlier, the prevention of waterborne diseases can have profound human benefits, including decreased mortality and morbidity rates, increased life span, and improved nutrition. The trilogy of water treatment, the separation of human and animal sewage from drinking water supplies, and the provision of clean foodstuffs (e.g., foodstuffs uncontaminated by sewage and washed by potable water) are substantially responsible for the 3-decade increase in the human life span enjoyed in many countries during the twentieth century. While vaccinations, improved housing, and other sanitary and social measures have contributed perhaps a third to this increase in the human life span, many authorities believe that nothing is as important as the prevention of waterborne disease. The demographic transition to longer life spans, and mortality due to diseases of old age and affluence (cancer, heart disease, etc.), could not have occurred without the prevention of waterborne disease.
Other benefits to the elimination of waterborne diseases depend on the technologies and methods used. For example, the provision of piped water removes the economic and social costs of carrying water by hand. The labor involved in obtaining water in many locations is a substantial burden in terms of labor, time, and nutritional cost, particularly for women and children. The provision of sewerage removes the costs and risks of contact with waste removal.
Economic Considerations And Progress Toward The Elimination Of Waterborne Diseases
Economic losses due to waterborne diseases include not only the direct costs of illness and treatment, but also the indirect costs of lost work, attendance in school, and other productive activities, and of long-term nutritional and socioeconomic achievement. Cost-effectiveness estimates regarding the benefits of water quality interventions, primarily for the prevention of diarrheal disease, have shown that almost all of the studied interventions are highly cost-effective, especially in poorer countries with high mortality rates. These interventions include: (1) improving access to ‘improved’ water sources and basic sanitation, such as latrines; (2) improving access to piped water and sewerage; and (3) household treatment of water through chlorination, filtration, solar disinfection, or flocculation with disinfection. Indeed, the authors of a recent analysis found that just the direct health-care cost savings to governmental bodies outweighed the costs of controlling waterborne diarrheal disease (see Haller et al., 2007). In countries where the risk of waterborne disease is highest, the cost of averting a disability-adjusted life year (DALY) is as little as US$20. This compares quite favorably with the cost of averting a DALY through the use of ORT.
Centralized Sanitation And Drinking Water Provision
In many countries the provision of potable water and sanitation as a communal effort has proven far less expensive, and effective, than individual household treatment. One of the traditional advantages of the ‘built’ environment (such as in cities or towns) has been the elimination of waterborne diseases through commonly used sanitation and water infrastructure that is inexpensive on a percapita basis. A major advantage is that excreta can be inexpensively centrally eliminated, disinfected, and disposed of away from sources of drinking water through sewerage. By drinking water and sanitation infrastructure we mean to include the identification of suitable source water, and its protection from microbial and chemical contamination; water disinfection and treatment; the distribution of potable water to communities free of cross-contamination with sewage or other pollutants; the centralized collection of excreta and its ultimate separation from water supplies unless disinfected; and maintenance of each of these pieces. In addition, this infrastructure obligatorily includes staff trained in sanitary engineering and operations. It must be noted that the conditions for centralized water treatment and sanitation do not exist in rural areas or in the burgeoning slums of many cities in poor countries.
Point Of Use Treatment Of Water To Prevent Waterborne Diseases
The recent explosive growth of urban centers globally has far outstripped water and sanitation infrastructure, leaving hundreds of millions of people at risk from waterborne diseases. Given this reality, and noting that in rural areas communal resources may be scanty, innovative methods for the prevention of waterborne diseases – such as individual household treatment by means of chlorination, solar (ultraviolet light, UV) disinfection, and flocculation with or without chemical disinfection – may be more appropriate. While heating water to 60ºC for a prolonged period, or boiling water, kills waterborne disease pathogens, the cost or availability of fuel may make the use of these other methods more cost effective. These circumstances explain the current, widespread interest in studying, and implementing, household-level disinfection practices that are affordable even in the poorest of communities. Recent studies have confirmed that killing pathogens through oxidation with a halogen, such as chlorine or chloramines, at the household level or at some central water source remains the most cost-effective strategy, with water filtration (at either a central site or the home) adding substantial additional benefits although with additional costs. Other methods include the storage of water atop roofs in inexpensive, second-hand clear plastic containers, where solar UV light can kill pathogens; simple settling, where particulates may carry adherent pathogens with them to the bottom of a container; and combined disinfection-flocculation.
With an ecological approach, it is possible to see that the treatment of drinking water before ingestion and the prevention of water contamination through sanitation serve the same goal of eliminating waterborne disease pathogens from transmission to humans. Sanitation has the additional benefit of reducing the contamination of agricultural foodstuffs. Good hygiene, promoted by the provision of clean water, acts as a second barrier to transmission within a household as well. There is an evolving literature suggesting that sanitation efforts may be most cost effective in densely populated urban areas, and water treatment (including at the household level) may edge out sanitation in more rural or slum areas. In cities, it appears that the most cost-effective approaches to reducing the burden of waterborne disease, and the largest reductions in diarrhea morbidity, appear to be related to sanitation alone; a combination of water quality and sanitation; or hygienic behavioral practices alone. (Historically, as outlined later, the near elimination of typhoid in rich nations dates to the implementation of sanitation to prevent fecal contamination of water, rather than to the initiation of water treatment via filtration or chlorination.) In addition, the promotion of basic hygienic practices such as hand washing may be facilitated by having water connections in homes, as it has been shown that households with individual connections have less diarrheal disease than do households that use standpipe water. It has been suggested that this is because water use is higher in houses with individual connections, and the incrementally greater use of water may go to improved hygiene.
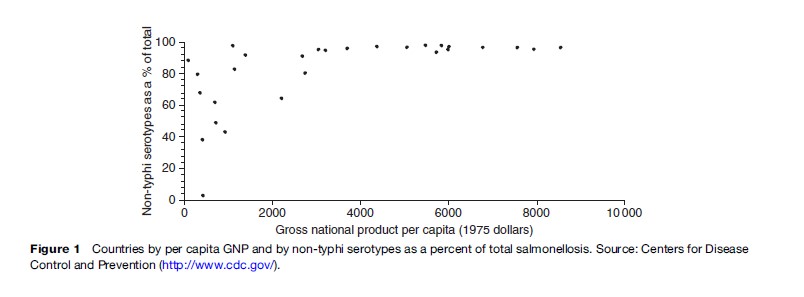
There are excellent data to show that poor countries do not need to have high per-capita incomes in order to eliminate or greatly decrease waterborne diseases. Typhoid is a disease caused by a Salmonella bacterium that is essentially only found in, and transmitted from, humans. It is excreted in feces and urine and can only infect other humans when there is contact with the feces or urine from infected people, for example, through person-to-person contact or through water or food contaminated by human excrement. Other Salmonella bacteria are found in many other animals such as chickens and cattle. Thus, the incidence of typhoid in a population is a measure of human contact with human excrement. As sanitation, hygiene, and water treatment improve, then the proportion of typhoid disease decreases and the proportion caused by other Salmonella serotypes increases. In Figure 1, it can be seen that some countries have essentially eliminated typhoid despite having a per capita Gross National Product of less than US$1000 in 1975 dollars, which is perhaps US$2000 now.
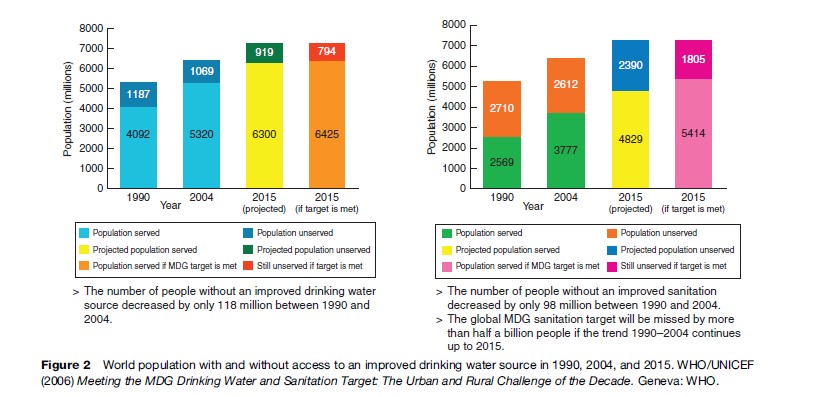
The fact that eliminating or controlling waterborne diseases is cost effective does not mean, alas, that these efforts are being undertaken at a pace that will ensure the elimination of waterborne disease. A recent progress report from WHO (2006) has made it clear that ‘‘with half of developing country populations still lacking basic sanitation, the world is unlikely to reach its target’’ of halving the number of people without sustainable access to safe drinking water and basic sanitation (United Nations Millennium Development Goals [MDG]). It is estimated that during the period 2005–2015, there will need to be an additional 450 000 people per day who acquire basic sanitation, and an additional 300 000 people per day who acquire improved drinking water (see Figure 2). Without additional political and economic resources, the challenge of waterborne diseases will remain for decades or centuries to come.
Source Water Protection And The ‘Multi-Barrier’ Approach
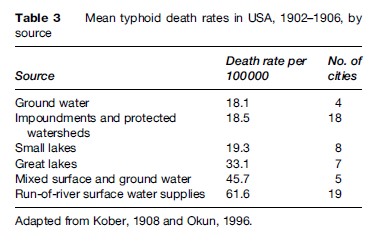
Optimally, source water is uncontaminated by pathogens, and thus when it is ingested or used for cooking or washing, it poses no risk of communicable disease. Of course, this is rarely the circumstance, yet source water protection is a critical element in the prevention of waterborne disease. Over 100 years ago it was recognized that protected watersheds, and groundwater (where the soil acts as a filter), were far more safe than open surface bodies of water or rivers. In 1908, Kober in the United States reported mean typhoid rates (Table 3) that showed a more than threefold higher typhoid death rate in cities whose source water was an open river, as compared with cities with either groundwater or protected watersheds. Cities that draw on river water are, of course, also drinking the diluted sewage dumped into the river by the communities upstream of them. In some countries, forward-thinking groups, governments, and civic institutions have purchased land with pristine water for their community’s future use, which both protects public health and reduces the cost of water treatment. Protection can also include measures such as banning the entry of human or animal wastes into the source, limiting recreational use of the source water, and banning nearby development (residential, industrial, and agricultural).
The second concept of importance is the use of redundant barriers to the contamination of water and redundant methods for treatment, known as the multi-barrier approach (see Figure 3). In a very real sense, source water protection is an important ‘barrier’ to waterborne disease, but it is not adequate in and of itself. Source water can be of variable quality; and should contamination of the source occur, then some form of subsequent treatment is needed to kill or remove pathogens. Conventional water treatment that incorporates the multi-barrier approach includes the use of flocculation agents, to remove some of the suspended particles to which pathogens can adhere, with settling tanks that allow the flocculant to settle; filtration through sand or similar media to physically remove pathogens, especially those present as cysts or oocysts or eggs; disinfection with halogenated compounds, such as chlorine or chloramines, that will kill most viruses and bacteria, and some protozoa, and which will persist in the piped delivery system so that any residual pathogens do not regrow; and the prevention of cross-contamination. By cross-contamination we mean the contamination of treated water with untreated water or sewage. Pipes laid in the ground may corrode or crack, allowing contamination, and many epidemics have been documented where (for misguided reasons of cost savings) sewer pipes and drinking water pipes have been laid next to one another in the same trench. Recent sophisticated studies have shown that short-term, low- or even negative-pressure waves can occur in distribution pipes. If the surrounding soil and water in the soil contain pathogens, this will allow contamination to occur if the pipes are cracked or lack one-way valves into households.
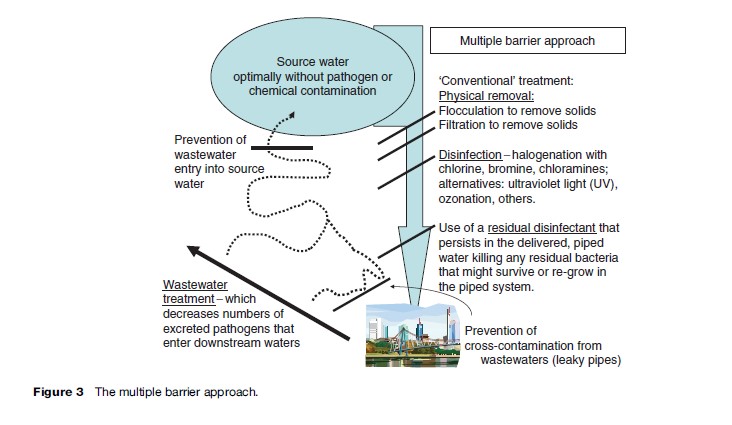
In the absence of costly infrastructure such as centralized water treatment and household delivery of water through piping and taps, it is still possible to adopt a multi-barrier approach at the household level. Water used for drinking, cooking, or personal washing can be disinfected through boiling or adding chlorine or commercially sold bleach solutions. Behavioral modification to enhance hand washing after defecation or taking care of family members with diarrhea can prevent secondary household transmission of waterborne diseases. Water can be stored in traditionally shaped vessels with narrow mouths, so that children and impatient adults do not soil the water through hand contact during use. Defecation in the open can be altered through education and efforts at behavioral modification in the use of latrines, septic systems, and sewerage.
Historically, some cities and communities have chosen to treat poor-quality source water rather than protect their source water. Some communities have no choice about what water is available to them, and must therefore utilize robust water treatment to render their water drinkable. Often there is tension between adherents of source water protection and those of water treatment. For example, sanitary engineers may wish to add treatment modalities such as filtration to a water supply, while environmentalists may be concerned that this addition will allow real estate developers to push for activities that will degrade the source water. Urban communities may push for increased recreational use of reservoirs (boating, swimming) that inevitably lead to increased fecal and chemical contamination. The rationale here is that more robust treatment, if put into place, will ‘take care’ of the increased contamination due to development or increased recreational use in the watershed.
The Future: Emerging Issues And Methods For Measuring And Understanding The Burden Of Waterborne Diseases
One key issue is that the etiologic agents of waterborne disease are still incompletely understood, even if the major source of disease (fecal contamination) is well known. The majority of waterborne disease outbreaks that cause diarrhea are still uncharacterized in terms of their etiologic agents, perhaps because many are viral in origin and few accurate, inexpensive tests are available for their detection. It is likely that the major advances in genomics will lead to the use of rapid diagnostic methods, such as ‘chips’ with many thousands of ligands for pathogen DNA or RNA, to better identify the causes of waterborne illness. Much of the impetus for this may be the desire to detect pathogens that could be used for bioterrorism.
Related to the issue of emerging pathogens is the waterborne transmission of diseases, other than gastroenteritis, which may not be recognized as related to water, either because of multiple routes of transmission, such as food, or because they are still emergent. An example is Microsporidia, which can cause syndromes other than gastroenteritis in susceptible hosts. Again, genomic microchips that recognize signature genetic elements, or similar technologies, could be used diagnostically from concentrated water samples (as well as from human specimens) to identify such emerging pathogens.
A second key issue in waterborne diseases is to understand the level and severity of endemic transmission of these diseases, as opposed to the often more dramatic (and therefore more easily noticed) epidemics of disease. There is a substantial body of literature that suggests that low-level, endemic transmission of waterborne pathogens may be more important than epidemics, particularly when partially or incompletely effective sanitation and treatment is present, dampening the magnitude of epidemics but still allowing for transmission. This requires not only good surveillance for these diseases, but also the mathematical and biostatistical capacity to see associations that may not be obvious. For example, when a person acquires a waterborne disease and does not know where they acquired the organism, or does not recall contact with an infected person, then the illness cannot be ascribed to water by public health authorities with assurance. Further complicating this situation is that many waterborne pathogens have multiple potential routes of transmission. Modern methodologies, such as time series analysis, have proven useful in this regard. Indeed, through statistical means it is even possible to quantify the ‘waves’ of illness that proceed through a community after an illness has been introduced into a community (Naumova et al., 2003).
Tied to the issue of epidemic and endemic disease is a third issue, which is the capacity of water treatment to deal with fluctuating levels of contaminants in source waters. In particular, meteorological factors and climate can profoundly affect the levels of pathogens in water. It has been shown that rainstorms can increase concentrations of parasites such as Cryptosporidium by several orders of magnitude, as they are flushed from land or from watershed sediments. It has also been shown that the recognized epidemics of waterborne disease in the United States are associated with prior heavy rainfall. Manure from concentrated animal feedlot operations is often sprayed on land to dry (presumably killing pathogens by desiccation and soil absorption), and can serve as a powerful source of water contamination after heavy rainfall. In addition, for reasons of economy, in many communities rainfall collection systems often empty into sewer systems, the capacities of which in times of heavy rainfall can be overwhelmed, leading to sewage entering drinking water sources without adequate treatment. If a water system is designed to remove or kill 99.9% of a rare pathogen, then it is unlikely that much endemic disease will occur; however, in the event of a heavy rainfall or sewage overflows, it must be expected that the system will not be adequate to protect public health and that high levels of ‘endemic’ or even epidemic disease may result.
Summary
The control of waterborne diseases is an urgent global problem that disproportionately affects poor nations and rural populations, yet it remains a threat even in rich countries. Simple sanitation practices, such as the use of latrines, and water disinfection, can lead to major improvements in human health. For those parts of the globe where centralized sanitation and water treatment plants are lacking, and are likely not to be built because of poverty or low population density, novel methods for the disinfection of water and wastes are a high priority. Point-of-use disinfection methods are being devised and refined, and may offer substantial advantages in these circumstances. It must be noted that one advantage of centralized systems – that they benefit everyone, rich and poor alike – may be absent if only the wealthy can afford to treat water in their own home.
Bibliography:
- Burstrom B, Macassa G, Oberg L, Bernhardt E, and Smedman L (2005) Equitable child health interventions: The impact of improved water and sanitation on inequalities in child mortality in Stockholm, 1878 to 1925. American Journal of Public Health 95: 208–216.
- Ferrie JP and Troesken W (2008) Water and Chicago’s mortality transition, 1850–1925. Explorations in Economic History 45: 1–16.
- Haller L, Hutton G, and Bartram J (2007) Estimating the costs and health benefits of water and sanitation improvements at global level. Journal of Water and Health 5: 467–480.
- Liew KB and Lepesteur M (2006) Performance of the rural health improvement scheme in reducing the incidence of waterborne diseases in rural Sarawak, Malaysia. Transactions of the Royal Society of Tropical Medicine and Hygiene 100: 949–955.
- Luby SP, Agboatwalla M, Feiken DR, et al. (2005) Effect of hand-washing on child health: A randomized controlled trial. The Lancet 366: 225–233.
- Merchant AT, Jones C, Kiure A, et al. (2003) Water and sanitation associated with improved child growth. European Journal of Clinical Nutrition 57: 1562–1568.
- Naumova EN, Egorov AI, Morris RD, and Griffiths JK (2003) The elderly and waterborne Cryptosporidium infection: Gastroenteritis hospitalizations before and during the 1993 Milwaukee outbreak. Emerging Infectious Diseases 9: 418–425.
- Pruss-Ustun A and Corvala´ n C (2006) Preventing Disease through Healthy Environments: Towards an Estimate of the Environmental Burden of Disease. Geneva, Switzerland: World Health Organization.
- World Health Organization (WHO) (2006) Meeting the Millennium Development Goals Drinking Water and Sanitation Target: The Urban and Rural Challenge of the Decade. Geneva, Switzerland: WHO.
- Ali SH (2004) A socio-ecological autopsy of the E coli O157:H7 outbreak in Walkerton, Ontario. Canada Social Science and Medicine 58: 2601–2612.
- Griffiths JK and Winant E (2007) Environmental health in the global context. In: Markle W, Fisher M and Smego R (eds.) Understanding Global Health. New York: McGraw-Hill Professional.
- Howard G and Bartram J (2003) Domestic Water Quantity, Service Level and Health. Geneva, Switzerland: World Health Organization.
- Hutton G and Haller L (2004) Evaluation of the Costs and Benefits of Water and Sanitation Improvements at the Global Level. Geneva, Switzerland: World Health Organization.
- Water Science and Technology Board, National Research Council (1999) Identifying Future Drinking Water Contaminants. Washington, DC: National Academy Press.
- Lorntz B, Soares AM, Moore SR, et al. (2006) Early childhood diarrhea predicts impaired school performance. Pediatric Infectious Diseases Journal 25: 513–520.
- Naumova EN, Jagai JS, Matyas B, DeMaria A Jr., MacNeill IB, and Griffiths JK (2006) Seasonality in six enterically transmitted diseases and ambient temperature. Epidemiology and Infection 135: 281–292.
- Watson T (2006) Public health investments and the infant mortality gap: Evidence from federal sanitation interventions on U.S. Indian reservations. Journal of Public Economics 90: 1537–1560.
- https://www.cdc.gov/healthywater/drinking/public/water_diseases.html – Centers for Disease Control and Prevention (CDC): Water-related Diseases and Contaminants in Public Water Systems.




