View sample urban health systems research paper. Browse research paper examples for more inspiration. If you need a health research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Introduction
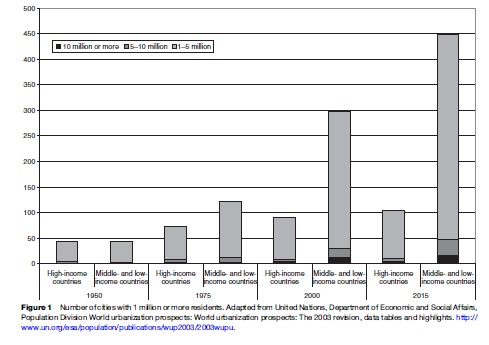
Demographic trends suggest that there is an urgent need to consider the health of urban populations. Cities are becoming the predominant mode of living for the world’s population. According to the United Nations (UN), approximately 29% of the world’s population lived in urban areas in 1950. By 2000, 47% lived in urban areas and the UN projects that approximately 61% of the world’s population will live in cities by 2030. Overall, the world’s urban population is expected to grow from 2.86 billion in 2000 to 4.94 billion in 2030. As the world’s urban population grows, so does the number of urban centers. The number of cities with populations of 500 000 or greater grew from 447 in 1975 to 804 in 2000. In 1975 there were four megacities with populations of ten million or more worldwide; by 2000 there were 18, and 22 are projected by 2015. As illustrated by Figure 1, most cities are in middle to low-income countries; in 2000 middle to low-income countries contained 72% of the world’s cities. During the second session of the World Urban Forum in 2004, world leaders and mayors warned that rapid urbanization is going to be one of the most important issues in this millennium.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
A Brief History Of Urban Health
Cities and their impact on health have been a concern for millennia. City architects as early as the fourth century BCE designed cities to maximize exposure to the sun in winter, minimize solar exposure in the summer, and take advantage of mountain and sea breezes (Semenza, 2005). More familiar, recurrent plague epidemics in European cities between the fourteenth and sixteenth centuries, and pestilence within slums early in the Industrial Age became a major concern for urban dwellers such that authorities were required to develop and maintain knowledge for dealing with the epidemics.
For centuries, researchers and scholars have considered the study of how cities may shape health an important area of inquiry. Some of the early epidemiological studies and interventions were centered on urban populations. John Graunt, considered by many to be the first epidemiologist, published Natural and Political Observations Mentioned in a Following Index, and Made upon the Bills of Mortality in 1662. In it, he presented the first life tables, as well documenting increases in urban populations due to immigration. Almost two centuries later, John Snow, in what might be considered a prototypical urban health intervention, removed the Broad Street pump handle after observing differential attack rates for cholera in London.
Until relatively recently, in the academic literature, urban living and its related exposures were considered mainly in terms of their detrimental effects. This urban health ‘penalty’ perspective, described by Andrulis and others, focused attention on poor health outcomes in an inner-city environment and disparities in the burden of morbidity and mortality, as well as disparities in healthcare access, among specific subgroups. Recent work, however, has shown that urban living may be health promoting and may confer an urban health ‘advantage.’ Urban areas can provide access to cultural events, educational opportunities, cutting-edge medical facilities, and a plethora of health and social services. Moving forward, academic interest in urban health will likely balance the features of the urban environment that both promote and harm population health.
Defining Urban Areas
There is little consensus about the definition of urban and what constitutes a city across national and international entities and disciplines. The U.S. Bureau of the Census defines an urbanized area as ‘‘a place and the adjacent densely settled surrounding territory that together comprise a minimum population of 50,000 people,’’ where the ‘‘densely settled surrounding territory’’ is defined as ‘‘one or more contiguous block having a population density of at least 1,000 people per square mile.’’ The Census bureau thus provides a dichotomy whereby territory, population, and housing units within specific size and density parameters are designated urban and those that are outside those parameters are nonurban. However, there are inherent limitations to these definitions: urban areas exist in contrast to rural or simply in contrast to nonurban areas. In the twenty-first century, few cities exist in extreme isolation such that what is not defined as city is rural (e.g., Las Vegas). Most cities (e.g., New York City, London, Bangkok, etc.) are actually far-reaching densely populated areas, containing peri-urban and suburban areas, which continue relatively uninterrupted for miles beyond the municipal city boundaries and the city center. Alternative definitions have been developed and rates of disease, risk, and protective behaviors vary between definitions.
The definition of urban also varies widely between countries. Among 228 countries on which the UN had data for in 2000, almost half (100) include size and density as criteria, 96 include administrative definitions of urban (e.g., living in the capital city), 33 include functional characteristics (e.g., economic activity, available services, etc.), 24 have no definition of urban, and 12 define all (e.g., Anguilla, Bermuda, the Cayman Islands, Gibraltar, the Holy See, Hong Kong, Monaco, Nauru, Singapore) or none (e.g., Pitcairn Island, Tokelau, and Wallis and Futuna Islands) of their population as urban. Official statistics (e.g., UN statistics detailed previously) rely on country-specific designations and as such vary widely. In specific instances, definitions of urban in adjacent countries vary tremendously (e.g., Cambodia vs. Vietnam). Furthermore, definitions of urban have changed over time in different ways in different countries. Therefore, global statistics are subject to country-level differences in the definition of urban that may be based on population density or specific urban features (e.g., proportion of agricultural workers, municipal services).
Conceptualizing Urban Exposure As A Determinant Of Health
We can conceptualize urban exposure in three main ways: urbanicity, urbanization, and the urban environment. ‘Urbanicity’ focuses on characterizing the presence of conditions at a particular point in time (i.e., prevalence) that are particular to urban areas or present in urban areas to a much greater or lesser extent than in nonurban areas. The focus on urbanicity is important to public health assessments on prioritizing current needs and approaches.
Urbanization is more dynamic in that it refers to the change in size, density, and heterogeneity of cities and provides a perspective for public health planning. Factors such as population mobility, segregation, and industrialization frequently accompany urbanization. More simply stated, urbanization is the process that involves the emergence and growth of cities. Thus the process of urbanization is not dependent on definition of urban per se, but rather on the dynamics of agglomeration of individuals. Although the pace of urbanization is independent of the base size of the population, the population size/density of surrounding areas may shape the pace of urbanization. For example, urbanization may include the establishment (or destruction) of new buildings or neighborhoods, development (or removal) of transportation routes, and the in-migration and out-migration of people, changing the racial/ethnic composition of cities. The process of urbanization gives rise to unique features of urban areas that merit separate study. How the dynamics of urbanization affect health can be considered with examples. An influx of impoverished peoples to a city (e.g., immigration driven by food or work shortages in nonurban or other urban areas) in search of jobs and services may tax available infrastructure including transportation, housing, food, water, sewage, jobs, and health care. Overtaxed sanitary systems may directly lead to rapid spread of disease as has been the case many times in North America during the past century and as continues to be the case in the developing world today. Also, the population strain on available jobs may result on devaluation of hourly wage rates, higher unemployment, and changing socioeconomic status for persons previously living in a given city. This lowering of socioeconomic status can result in more limited access to health care and to poorer health. Therefore, characteristics of urbanization, including the intensity, rate, and duration of these changes, and the response to these changes, all may have health effects on urban residents. Common mechanisms may exist through which urbanization affects health independent of the size of the city in question.
The urban context or environment can be defined as the specific characteristics or features of cities that influence health. Consider the urban environment as three distinct concepts: the social environment, the physical environment, and the urban resource infrastructure. The social urban environment comprises contextual factors that include social norms and attitudes, disadvantage (e.g., neighborhood socioeconomic status), and social capital (e.g., social trust, social institutions, etc.). The urban physical environment refers to the built environment, pollution, access to green space, transportation systems, and the geological and climate conditions of the area the city occupies. Features of the urban resource infrastructure that influence health may include factors such as the availability of health and social services, and municipal institutions (e.g., law enforcement). Features of the urban environment – the social and physical environment, as well as the infrastructural resources – all in turn are influenced by municipal, national, and global forces and trends.
Types Of Studies To Investigate Issues Of Health In Urban Populations
Urban Versus Rural
Urban versus rural studies typically contrast urban areas with rural areas in the same country or consider morbidity and mortality in urban versus nonurban areas. Essentially, these studies seek to determine whether morbidity and mortality due to a specific health outcome is different in specific urban areas as compared to specific nonurban areas.
Urban versus rural (or nonurban) comparisons are useful in drawing attention to particular health outcomes that may be more or less prevalent in urban areas and merit further investigation to examine the specific features of the urban (or rural) environment that are associated with that outcome. Recognizing that urban–rural comparisons are too blunt, more recent work has refined distinctions such as urban core, urban adjacent, urban nonadjacent, and rural. However, such studies are limited in their ability to identify what those factors may be and what the pathways are through which they affect the health of urban dwellers. Features of cities change over time and some factors may not be conserved between cities (e.g., racial/ethnic distribution). It is unsurprising then that different urban–rural comparisons have provided conflicting evidence about the relative burden of disease in urban and nonurban areas. At best, these studies reveal gross estimates of the magnitude and scope of health measures in broad areas by geographical areas typically defined by size and population density.
Interurban
Interurban studies typically compare health outcomes between two or more urban areas between or within countries. Such studies can simply identify differences between cities or they can begin to examine specific features of cities that influence health. Examples of the former are numerous. For example, Vermeiren and colleagues (2003) have compared mental health outcomes among adolescents in New Haven (United States), Arkhangelsk (Russia), and Antwerp (Belgium), providing insights about cross-cultural, cross-urban similarities and differences in antisocial behavior, depression, substance use, and suicide. A study of Puerto Rican injection drug users in New York City (United States) and Bayamo´n (Puerto Rico) revealed several differences between the two ethnically similar populations; injection drug users in Puerto Rico injected more frequently (Colon et al., 2001) and had higher rates of needle sharing as compared to their New York counterparts (Deren et al., 2001). The authors pointed to similarities in drug purity (Colon et al., 2001) and differences in the onset of the crack epidemic (Deren et al., 2001) as city-level factors that influenced injector risk behaviors. When using the city as the unit of analytic interest, one implicitly assumes that city-level exposures are equally important for all residents. Studying differences in drug use risk behaviors among two cities does not permit analysis of differences in behaviors within cities because of location of residence, intraurban variability in barriers to safer behaviors, or variations in access to key services (e.g., drug treatment, needle exchange) provided to different urban residents. However, interurban studies such as the examples mentioned here can help guide municipal and state policy makers when making decisions on service provision throughout a city.
Intraurban
Intraurban studies typically compare health outcomes within cities and are becoming widely used to investigate specific features of the urban environment. These studies often focus on neighborhoods, specific geographic areas within a city that are generally administrative groupings (e.g., census tracts in Canada, subareas or suburbs in South Africa). However, it is important to note that these areas may not represent residents’ perceptions of their neighborhoods. The Project for Human Development in Chicago Neighborhoods (PHDCN), which identified collective efficacy as a determinant of violence in urban neighborhoods (Sampson et al., 1997), is an example of such a study and has demonstrated their potential to guide specific interventions to improve urban health. As a result of findings from the PHDCN, public health interventions have been developed that attempt to increase collective efficacy and social capital in particular urban neighborhoods.
Intraurban studies may contribute important insights into the relations between specific urban features and health outcomes. However, it may be difficult to generalize from one city to another. For instance, the relation between collective efficacy and violence may be modified by different levels of policing or differential access to illicit substances within a given city. Furthermore, it is important to consider that neighborhood residence is a function of geographical location and other types of social ties that are facilitated or necessitated by the urban environment.
Defining And Quantifying Urban Exposures
Social Environment
The urban social environment includes features such as social norms and attitudes, income distribution, and social capital. Although we summarize some key aspects of the social environment, the list provided here is by no means exhaustive. (For a more comprehensive consideration of the urban social environment, see the section titled ‘Further reading.’)
Social norms are patterns of behaviors that are considered accepted and expected by a given society. From the perspective of urban health, societal and cultural norms are important considerations when thinking about the behavior of urban dwellers and may exist on several levels. For example, Frye et al. (2006) considered the role of social norms in shaping behaviors among men who have sex with men (MSM) in urban communities. They posited that MSM may be influenced by the social norms of the gay community, with its unique physical and social structures and cultural characteristics as well as smaller subpopulations within the gay community. These communities may not be limited to one geographic location, however. Thus, MSM may also be influenced by the norms operating within their geographical neighborhood, which may have norms that operate in conjunction with, or opposition to, the prevailing norms of the broader gay community.
Income inequality is the relative distribution of income within a city or neighborhood, and is typically operationalized with the Gini coefficient. Income inequality has been associated with several health outcomes, including self-rated health, cardiovascular mortality, and consequences of illicit drug use. Income inequality is thought to operate through material and psychosocial pathways to shape population health independently of absolute income. For example, Subramanian et al. (2003) reported a significant association between self-rated health and community level income inequality among adults in Chile, even after adjusting for absolute household and community income.
According to Berkman and Kawachi in Social Epidemiology (2000), social cohesion is the connectedness among groups and includes elements such as strong social bonds and a lack of conflict within the community. Social capital is thought to provide resources for collective action. There is evidence that the absence of social capital is associated with negative health outcomes such as increases in mortality, poor self-rated perception of health, higher crime rates, and violence.
Physical Environment
The urban physical environment refers to the built environment (e.g., green space, housing stock, transportation networks, etc.), pollution, noise, traffic congestion, and the geological and climate conditions of the area the city occupies. The built environment refers to ‘‘housing form, roads and footpaths, transport networks, shops, markets, parks and other public amenities, and the disposition of public space’’ (Weich et al., 2001). Recent studies have suggested that poor-quality built environments are associated with depression, drug overdose, and physical activity. Examination of the association of built environment and health overall is a relatively recent area of inquiry (for a more thorough treatment of health and the built environment, see the September 2003 issues of the Journal of Urban Health 80(3): 359–519 and the American Journal of Public Health 93(9): 1376–1598).
Green space (e.g., parks, esplanades, community gardens, etc.) has the potential to significantly contribute to the health of urban dwellers. Living in areas with walk able green spaces has been associated with increased longevity among elderly urban residents in Japan, independent of their age, sex, marital status, baseline functional status, and socioeconomic status (Takano et al., 2002).
Urban transportation systems include mass transit systems (i.e., subways, light rail, and buses) as well as streets and roads. According to the Light Rail Transit Association, there are 135 subways currently operating in 67 countries worldwide. Urban transportation systems on one hand are key in the economic livelihoods of city residents as well as cities as a whole. Yet on the other, there are significant health considerations for mass transit and roadways including security and violence, noise, and exposure to pollutants. These exposures are relevant not only for transit workers, but also for transit riders.
Pollution is one of the well-studied aspects of the urban physical environment. Urban dwellers are exposed to both outdoor and indoor pollutants that include heavy metals, asbestos, and a variety of volatile hydrocarbons. For example, one study in Bangkok (Thailand) reported high levels of benzene and polycyclic aromatic hydrocarbons among street vendors and school children sampled from traffic congested areas as compared to monks and nuns sampled from nearby temples (Ruchirawat et al., 2005).
Urban Resource Infrastructure
The urban resource infrastructure can have both positive and negative effects on health. The urban infrastructure may include more explicit health-related resources such as health and social services as well as municipal structures (e.g., law enforcement), which are shaped by national and international policies (e.g., legislation and cross-border agreements).
The relation between availability of health and social services and urban living is complicated and varies between and within cities and countries. In wealthy countries, cities are often characterized by a catalog of health and social services. Even the poorest urban neighborhood often has dozens of social agencies, both governmental and nongovernmental, each with a distinct mission and providing different services. Many of the health successes in urban areas in the last two decades, including reductions in HIV transmission, teen pregnancy rates, tuberculosis control, and new cases of childhood lead poisoning, have depended in part on the efforts of these groups. For example, social and health services are frequently more available in cities than they are in nonurban areas, which may contribute to better health and well-being among urban residents. Despite wider availability of social and health services in cities, many cities are experiencing remarkable disparities in wealth between relatively proximate neighborhoods, which are often associated with disparities in the availability and quality of care. Low-income urban residents face significant obstacles in finding health care both in wealthy and less-wealthy countries.
Municipal, National, And Global Forces And Trends
Municipal, national, and global forces and trends can have a far-reaching impact on both urban living and urbanization. Legislation and governmental policies can have substantial influence on the health of urban dwellers. Historically, municipal regulations regarding sanitation in the nineteenth and twentieth centuries facilitated vast improvements in population health and led to the formation of national groups dedicated to improving population health like the American Public Health Association. A contemporary example of the power of legislation to influence health has been ongoing in the state of New York (United States) since the early 1970s. In 1973 the New York state legislature, with the encouragement of then Governor Nelson Rockefeller, enacted some of the most stringent state drug laws in the United States. Characterized by mandatory minimum sentences, the Rockefeller Drug Laws have led to the incarceration of over 100 000 drug users since their implementation. Those incarcerated under the Rockefeller Drug Laws overwhelmingly are New York City residents (78%) and black or Hispanic (94%). Assuming that each year incarcerated was a year of life lost, Drucker estimated the potential years of life lost as a result of the Rockefeller Drug Laws to be equivalent to 8667 deaths (Drucker, 2002).
Regional and global trends can affect not only urban living, but also the rate and process of urbanization or de-urbanization. Changes in immigration policies or policy enforcement can impact urban dwellers in a variety of ways including, but not limited to, changes in access to key health and social services for some subpopulations, changes in community policing practices and changes in social cohesion and levels of discrimination. Terrorist attacks in urban centers (e.g., Baghdad, Jerusalem, London, Madrid, New York) are associated not only with morbidity and mortality among those directly affected by the event, but also significant psychological distress for other residents of the cities. Armed conflicts have resulted in mass displacement of individuals, some of whom have fled cities for other cities, regions or countries, or camps for displaced individuals (e.g., Darfur).
Methods For Studying Urban Health
The study of urban health requires the employment of analytic resources from diverse disciplines that can combine to produce an understanding of how features of the urban environment influence population health. We summarize the contribution of selected qualitative and quantitative methods to the study of urban health.
Qualitative Methods
Participant Observation
Participant observation involves systematic observation of a phenomenon of interest while engaging as a participant in that setting. Participant observation offers opportunities for the researcher to develop an in-depth understanding of a particular social context through their experience as an actor within that context. Some of the classic studies of urban life were developed using participant observation, including William Foote Whytes’s Street Corner Society (1943) and Carol Stack’s All Our Kin (1977). A more recent example of participant observation in an urban community was Bourgois’s (2003) study of crack cocaine sellers in East Harlem, New York City. This study highlighted the unstable, contingent, and constantly negotiated nature of city living within the context of a predominantly minority and economically disadvantaged neighborhood with open-air illicit drug markets.
In-Depth Interviews
In-depth interviews are designed to gather information about the experience, interpretations, understandings, and reactions to a particular phenomenon in a respondent’s own words. Whereas quantitative interviews offer respondents a set of predetermined response categories from which to choose, qualitative interviews are usually open-ended and invite respondents to discuss the topic of interest in their own words. The structure of in-depth interviews is variable, ranging from a set of predetermined questions presented in a predetermined order to a set of topics to be covered in no particular order within the span of the interview. Often, the open-ended nature of the questions allows researchers to explore and elucidate areas that would not be captured in qualitative interviews. Similarly, analysis of in-depth interviews can be conducted in a manner that ranges from the application of predetermined categories to more inductive approaches in which the goal is to identify constructs and their relationships based on their presentation in the interviews.
Within urban contexts, in-depth interviews can be used productively to elicit residents’ understandings of their environments and perceptions of the ways that those environments influence residents’ health. Correspondingly, they can be used productively with urban residents, health providers, and key decision makers to develop mechanisms to improve social contexts and address health issues within urban environments. Sampling decisions should be shaped by the specific question of interest and may range from random sampling to specific selection of key informants (e.g., decision makers, longtime neighborhood residents).
Focus Groups
Focus groups are interviews that are generally made up of small samples of individuals – generally between 6 and 12 per group – to discuss a topic or process of interest in detail. Focus groups are often used when the topic is one that is not highly sensitive and when a goal is to enable participants to interact with one another around the topic. Focus group interviews often rely upon interactions among group members on a topic provided by the researcher (who may take the role of facilitator). Participants discuss ideas, issues, insights, and experiences among themselves, commenting, criticizing, or elaborating on the views expressed by previous speakers.
As with in-depth interviews, focus groups can be relatively structured or unstructured. A facilitator knowledgeable about the topic of interest, skilled in group facilitation, and able to develop rapport with the focus group participants is essential to successful data collection. Analysis of focus group interviews may proceed using a deductive approach with categories determined a priori or with an inductive approach that seeks to develop themes and categories out of the focus group material itself.
Quantitative Methods
Ecological Analyses
Ecological analyses consider associations using grouped or aggregated data for both exposure and outcomes. For example, ecological analyses can be used to consider the association between HIV prevalence and legal repressiveness across cities (defined as hard drug arrests per capita, police employees per capita, and corrections expenditures per capita; Friedman et al., 2006). Such simple correlations can suggest city features that covary with measures of city-level health for further consideration. More sophisticated techniques (e.g., multilevel multivariate regression analyses) can consider how particular features are associated with particular outcomes while accounting for the contribution of other potentially important variables. Ecological analyses have historically been the primary method used in interurban comparisons. In urban health research, ecological studies have been used for generating hypotheses. For example, ecological studies demonstrating that relative income within cities was associated with asthma hospitalization rates in New York City generated theories about the role of race/ethnicity and the neighborhood environment on the occurrence of asthma in cities.
Although ecological analyses are potentially useful in identifying features of the urban environment that may be associated with health, there are several inherent limitations to inferences that may be drawn from ecological analyses about how these features may impact health on the individual level. Causal inferences at the individual level cannot be drawn from ecological studies. For example, the ecological observation that residential areas in Tshwane (South Africa) with high socioeconomic circumstances have higher suicide mortality rates does not necessarily imply that wealthier individuals are more likely to commit suicide (Burrows and Laflamme, 2005). Such an inference is frequently referred to as the ecological fallacy, and highlights the limited interpretations that should be drawn from ecological studies. Still, ecological analysis will continue to be an urban health research tool for hypothesis generation and will continue to suggest features of cities that may be associated with health outcomes. It is important to note that ecological studies are not limited to interurban comparisons but can equally generate hypotheses about features of intraurban units, such as neighborhoods or residential areas, which can shape population health.
Multilevel Methods
Multilevel analyses integrate individual-level variables with group and macro-level variables so that multiple levels of influence can be assessed simultaneously. Multilevel models have been available since the 1960s although they did not come into widespread use for more than two decades due to limitations of early models. Multilevel analyses allow researchers to consider how specific features of cities or of units within cities (e.g., neighborhoods) contribute to individual health independent of the contribution of other individual and contextual variables.
In its simplest application to urban health, a multilevel analysis uses data from individuals in multiple cities (or neighborhoods within a city) to consider whether city living independently explains interindividual variability in health status after controlling for other relevant individual characteristics. More useful to the study of urban health, however, is the consideration of how different characteristics of urban living at multiple levels may be associated with a particular health outcome. For example, multilevel analysis can test whether racial/ethnic segregation between neighborhoods is associated with individual access to preventative health care (e.g., influenza vaccination) while controlling for social ties at the neighborhood level and for individual race/ethnicity and other key variables. With multilevel analyses, researchers can evaluate the possibility that the effect of urban living on health is different within and between cities by introducing random slopes that allow for varying strengths of the associations between urban characteristics and health.
Conclusion
Urban health is the study of urban characteristics – including features of the social and physical environment and features of the urban resource infrastructure – that can influence health and disease in the urban context. Global demographic trends suggest urban living has become normative and thus there is an urgent need to consider how urban living may influence the health of populations. The study of urban health requires a multidisciplinary perspective that can consider different types of studies, including interand intraurban studies and urban–rural comparisons, and employs a multiplicity of methods including qualitative and quantitative methods. Epidemiologists, public health practitioners, urban planners, as well as social, behavioral, clinical, and environmental health scientists can contribute to the study of urban health in conjunction with the active participation of community residents, civic, business, faith-based, and political leaders. The International Society for Urban Health (see the section titled ‘Relevant websites’) is an organization devoted to furthering perspectives and approaches to improving health in cities and can serve as a resource for those interested in further reading about the study of urban health.
Bibliography:
- Berkman LF and Kawachi I (eds.) (2000) Social Epidemiology. New York: Oxford University Press.
- Bourgois PI (2003) In Search of Respect: Selling Crack in El Barrio, 2nd edn. New York: Cambridge University Press.
- Bureau of the Census (2002) Qualifying urban areas for Census 2000. Department of Commerce. Federal Register, vol 67, No. 84. May 1, 2002: 21962.
- Burrows S and Laflamme L (2005) Living circumstances of suicide mortality in a South African city: An ecological study of differences across race groups and sexes. Suicide and Life-Threatening Behavavior 35: 592–603.
- Colo HM, Robles RR, Deren S, et al. (2001) Between-city variation in frequency of injection among Puerto Rican injection drug users: East Harlem, New York, and Bayamon, Puerto Rico. Journal of Acquired Immune Deficiency Syndrome 27: 405–413.
- Deren S, Robles R, Andia J, Colon HM, Kang SY, and Perlis T (2001) Trends in HIV seroprevalence and needle sharing among Puerto Rican drug injectors in Puerto Rico and New York: 1992–1999. Journal of Acquired Immune Deficiency Syndrome 26: 164–169.
- Drucker E (2002) Population impact of mass incarceration under New York’s Rockefeller drug laws: an analysis of years of life lost. Journal of Urban Health 79: 434–435.
- Friedman SR, Cooper HLF, Tempalski B, et al. (2006) Relationships of deterrence and law enforcement to drug-related harms among drug injectors in US metropolitan areas. AIDS 20: 93–99.
- Frye V, Latka MH, Koblin B, et al. (2006) The urban environment and sexual risk behavior among men who have sex with men. Journal of Urban Health 83: 308–324.
- Ruchirawat M, Navasumrit P, Settachan D, Tuntaviroon J, Buthbumrung N, and Sharma S (2005) Measurement of genotoxic air pollutant exposures in street vendors and school children in and near Bangkok. Toxicology and Applied Pharmacology 206: 207–214.
- Sampson RJ, Raudenbush SW, and Earls F (1997) Neighborhoods and violent crime: A multilevel study of collective efficacy. Science 277: 918–924.
- Semenza JC (2005) Building healthy cities: A focus on interventions. In: Galea S and Vlahov D (eds.) Handbook of Urban Health: Populations, Methods and Practice, pp. 459–478. New York: Springer.
- Stack C (1977) All Our Kin: Strategies for Survival in a Black Community. New York: Harper and Row.
- Subramanian SV, Delgado I, Jadue L, Vega J, and Kawachi I (2003) Income inequality and health: Multilevel analysis of Chilean communities. Journal of Epidemiology and Community Health 57: 844–848.
- Takano T, Nakamura K, and Watanabe M (2002) Urban residential environments and senior citizens’ longevity in megacity areas: The importance of walkable green spaces. Journal of Epidemiology and Community Health 56: 913–918.
- Vermeiren R, Schwab-Stone M, Deboutte D, Leckman PE, and Ruchkin V (2003) Violence exposure and substance use in adolescents: Findings from three countries. Pediatrics 111: 535–540.
- Weich S, Burton E, Blanchard M, Prince M, Sproston K, and Erens B (2001) Measuring the built environment: Validity of a site survey instrument for use in urban settings. Health and Place 7: 283–292.
- Whyte WF (1943) Street Corner Society: The Social Structure of an Italian Slum. Chicago, IL: University of Chicago Press.
- Andrulis DP (1997) The urban health penalty: New dimensions and directions in inner-city health care. Inner City Health Care. Philadelphia, PA: American College of Physicians. https://www.acponline.org/acp_policy/policies/urban_health_penalty_new_dimensions_directions_in_inner_city_health_care_1996.pdf
- Bureau of the Census (2002) Qualifying urban areas for Census 2000. Department of Commerce. Federal Register, vol 67, No. 84. May 1, 2002: 21962.
- Diez Roux AV (2001) Investigating neighborhood and area effects on health. American Journal of Public Health 91: 1783–1789.
- Freudenberg N, Silver D, Carmona JM, Kass D, Lancaster B, and Speers M (2000) Health promotion in the city: A structured review of the literature on interventions to prevent heart disease, substance abuse, violence and HIV infection in US metropolitan areas, 1980–1995. Journal of Urban Health 77: 443–457.
- Freudenberg N, Vlahov D, and Galea S (2005) Beyond urban penalty and urban sprawl: Back to living conditions as the focus of urban health. Journal of Community Health 30(1): 1–11.
- Galea S and Vlahov D (eds.) (2005) Handbook of Urban Health: Populations, Methods and Practice. New York: Springer.
- Harpham T and Tanner M (1995) Urban Health in Developing Countries, London: Earthscan.
- Kawachi I and Berkman LF (eds.) (2003) Neighborhoods and Health. New York: Oxford University Press.
- Leviton LC, Snell E, and McGinnis M (2000) Urban issues in health promotion strategies. American Journal of Public Health 90: 863–866.
- Luke DA (2004) Multilevel Modeling. Thousand Oaks, CA: Sage.
- Patton MQ (2001) Qualitative Research and Evaluation Methods. Newbury Park, CA: Sage.
- Raudenbush SW and Bryk AS (2002) Hierarchical Linear Models, 2nd edn. Thousand Oaks, CA: Sage.
- Vlahov D and Galea S (2002) Urbanization, urbanicity, and health. Journal of Urban Health 79(supplement 1): S1–S12.
- Vlahov D, Galea S, and Freudenberg N (2005) The urban health ‘‘advantage.’’ Journal of Urban Health 82: 1–4.
- https://unhabitat.org/ – United Nations Human Settlements Program.
- https://apps.who.int/iris/handle/10665/70718 – Commission on Social Determinants of Health, Knowledge Network on Urban Settings.




