Sample Phantom Limbs Research Paper. Browse other research paper examples and check the list of research paper topics for more inspiration. If you need a religion research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our research paper writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Many patients awake from the anesthetic after an amputation feeling certain that the operation has not been performed. They feel the lost limb so vividly that only when they reach out to touch it, or peer under the bed sheets to see it, do they realize it has been cut off. This startling realization does nothing to subdue the reality of the limb they experience, and may even intensify the sensations that define it. The first detailed description of this phenomenon was provided by the American Civil War surgeon, Silas Weir Mitchell (1871), who dubbed it the ‘phantom limb.’ The term so accurately captures the nature and subjective experience of the phenomenon that it has been adopted ever since. This research paper reviews the nature of phantom limb pain and nonpainful phantom limb sensations which arise after limb amputation.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
1. Phantom Limb Pain
For many amputees, a distressing problem is phantom limb pain. While the distinction between a painful and nonpainful phantom is not always clear-cut, it is useful to separate them for purposes of description, classification, and treatment. Painful phantom experiences vary in a number of dimensions. These include intensity, quality, location, frequency, and duration. Many amputees report a painful intensification of the tingling, ‘pins and needles’ or paresthetic quality (i.e., dysesthesias) that defines the nonpainful phantom limb. Some sufferers describe bouts of paroxysmal shooting pain that travel up and down the limb. Others report the phantom to be in a cramped or otherwise unnatural posture that gives rise to excruciating pain. Many amputees describe the pain in the phantom limb as indistinguishable from the pain they experienced in the limb before amputation. In still others, the phantom may be immobile or paralyzed so that attempts to move it generate pain. Finally, the phantom is often the seat of an intense burning pain, as if the hand or foot were held too close to an open flame. Frequently amputees suffer from several types of pain. Phantom limb pain, it appears, is equally prevalent among men and women, and is not related to side, level, age, or cause of amputation (Jensen and Nikolajsen 1999).
Surveys based on several thousand amputees reveal that between 78 percent and 85 percent of patients continue to experience significant amounts of phantom limb pain more than 25 years after amputation (Sherman et al. 1997). Prospective studies of the incidence of phantom limb pain are consistent with these estimates (Jensen et al. 1985, Nikolajsen et al. 1997). Between 50 percent and 71 percent of amputees report phantom limb pain two years after amputation. There is a reduction in the frequency and duration of attacks over time. Equally striking is the low success rate of treatments for phantom limb pain: in the long term only 7 percent of patients are helped by the more than 50 types of therapy used to treat phantom limb pain (Sherman et al. 1997).
The different qualities of phantom limb pain, its high prevalence and incidence, and its low treatment success rate point to the complexity of the problem. Phantom limb pain is not a unitary syndrome, but a symptom class, with each class subserved by different etiologic mechanisms. There is not just one cause of phantom limb pain. The development and severity of this disorder are determined by the interaction of multiple factors that vary across individuals. These include ectopic activity from peripheral nerves that were transected during amputation and have formed a neuroma, contributions from the sympathetic nervous system, sensitization of central nervous system structures due to the effects of amputation, inflammation and ectopic activity, alterations in the functional organization of sensory nucleii, past experience with pain, and the immediate physiological, motivational, and psychological states of the individual.
1.1 Pain Memories In Phantom Limbs
A striking property of phantom limb pain is the presence of a pain that existed in a limb prior to its amputation (Katz and Melzack 1990). This class of phantom limb pain is characterized by the persistence or recurrence of a previous pain, has the same qualities of sensation, and is experienced in the same region of the limb as the pre-amputation pain. Cases studies of amputees have revealed pain ‘memories’ of painful diabetic foot ulcers, bedsores, gangrene, corns, blisters, ingrown toenails, cuts and deep tissue injuries, and damage to joints and bony structures. In addition, the phantom limb may assume the same painful posture as that of the real limb prior to amputation, especially if the arm or leg has been immobilized for a prolonged period.
The proportion of amputees who report similar pain before and after amputation may be as high as 79 percent (Katz and Melzack 1990), although according to prospective studies, the incidence is approximately 10 percent at one year after amputation (Jensen et al. 1985, Nikolajsen et al. 1997). Pain also persists in patients with deafferentation that does not involve amputation. In these conditions, the involved body part is still present but it is devoid of sensibility due to an interruption in the supply of sensory (afferent) information (i.e., deafferentation). Brachial plexus avulsions, in which the sensory nerve roots supplying the arm and hand are torn from the spinal cord, often produce pain that is felt in the deafferented and anesthetic region. Similarly, patients with spinal cord injuries may complain of pain referred to body parts below the level of the transection, including, for example, a patient who continued to feel the pain of an ingrown toenail after a complete spinal cord break.
Painful and nonpainful sensations also persist or recur after surgical removal or deafferentation of body structures other than the limbs, such as breasts, teeth, and internal and special sense organs. Ulcer pain has been reported to persist after subtotal gastrectomy with removal of the ulcer. Patients have reported labor pain and menstrual cramps after total hysterectomy, rectal pain and hemorrhoids after removal of the rectum and anus, the burning pain of cystitis after complete removal of the bladder, and the pain of a severely ulcerated cornea after enucleation of an eye.
As noted above, not all phantom limb memories are of painful experiences. Nonpainful preamputation sensations do recur, but they are not as common and tend to include the sensation of objects that were once worn on the limb. These superadded sensations vary in complexity from such simple somatosensory qualities as the sensation of bandages that once wrapped a wound, a plaster cast, finger rings, and wristwatches to the multimodal, perceptually integrated phenomenon of a phantom foot clad in a sock and a shoe of specific type and color (Katz and Melzack 1990).
Taken together, these case reports and studies of amputees reveal that pain memories are not merely images or cognitive recollections; they are direct experiences of pain that resemble an earlier pain in location and quality. They are perceptually complex experiences that may even involve information from multiple sensory modalities including visual, olfactory, tactile, and motor components that had accompanied the original experience. The precise details of the experiences of pain involve localization, discrimination, affect, and evaluation—that is, all the dimensions of perceptual experience—and these properties are a function of integrated brain activity. It is likely that the outputs of sensitized spinal cells activate the neural structures in the brain that subserve memories of earlier events.
2. The Nonpainful Phantom Limb
The most salient property of the nonpainful phantom is the tingling, paresthetic quality, but sensations of temperature, posture, length, volume, and movement are also very common (Jensen and Nikolajsen 1999). The incidence of the nonpainful phantom is estimated to be between 80 percent and 100 percent. In fact, the presence of a nonpainful phantom is so common that it is considered a ‘normal’ sequela of amputation. It is standard practice to prepare the patient preoperatively for its subsequent occurrence.
The frequency with which a painless phantom occurs does not appear to be related to the extremity, side, level of amputation, age, gender, or reason for amputation (Jensen and Nikolajsen 1999). There is considerably more variability in the estimates of the duration of the nonpainful phantom. In some amputees, the phantom may disappear within days or weeks of the amputation. In others, it remains unchanged for up to 60 years.
2.1 Fading, Telescoping, And Shrinking Of The Phantom Limb
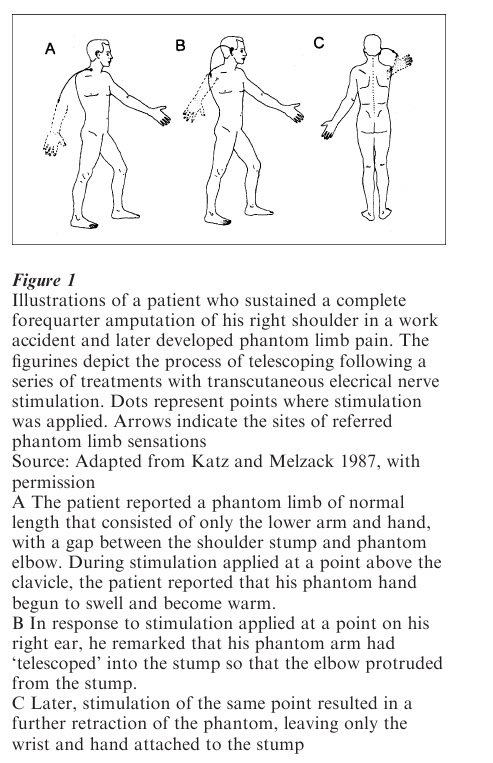
In many cases, the normal phantom undergoes a number of predictable changes within several years of amputation (Katz 2000). These include fading, telescoping, and shrinking. Immediately after amputation the phantom limb usually feels of normal length and size. Over time, the proximal portions begin to fade and soon disappear (Fig. 1). At this point, the phantom limb consists of only the extremity and major joints. These are felt at a normal distance from the body. The intervening parts have disappeared so that the phantom hand or foot feels as if it were hanging, unattached, in empty space. In the case of an amputation performed at the shoulder, the phantom limb may consist of only the lower arm and hand, with a gap between the shoulder stump and the phantom elbow. In approximately one-third of amputees, a process of ‘telescoping’ begins. Among upper extremity amputees, the phantom is perceived gradually to approach the stump so that the hand is located in phenomenal space on a level with the elbow of the other arm. As the process continues, the gap between the stump and phantom continues to close; the amputee may find that the hand is protruding from, or attached to, the end of the stump. Later, the phantom hand may retract into the stump so that only the tips of the fingers jut out. In some cases, eventually even these may disappear completely and permanently into the stump.
There are times when a completely telescoped phantom will temporarily lengthen so that the hand or foot is once again felt at a normal distance from the stump. Less commonly, the converse also occurs; a phantom which is already telescoped may temporarily retract completely into the stump, or one which is of normal, or shortened length may become even shorter. The circumstances and stimuli which bring about these changes are extremely varied and range from peripheral stimulation of the stump and other regions of the body to more central influences.
The process of telescoping is sometimes accompanied by a marked shrinking of the phantom to the dimensions of a child’s limb. This gradual diminution in perceived size or volume occurs in both upperand lower-limb amputees. The extent of shrinking that occurs is variable. Adult amputees have reported the phantom to be the size of a doll’s or baby’s hand, a silver dollar, or even as small as a postage stamp (Katz 2000).
2.2 Cortical Maps And Phantom Limbs
Factors governing the fading, telescoping, and shrinking of the phantom are not well understood. The gradual fading of the phantom is thought to represent a perceptual correlate of the re-establishment of inhibitory control over hyperactive or spontaneously active cells which subserve the phantom. The gradual telescoping and shrinking have been hypothesized to depend upon input from intact peripheral fibers located in the stump. These experiences appear to be perceptual markers of the short and long-term reorganizational changes that occur after amputation in central nervous system structures including the somatosensory cortex (Katz 2000, Merzenich et al. 1984). The perceived distance between the phantom and the stump may be a function of the distance separating their respective representations in the cortical map.
2.3 Psychophysical Correlates Of Phantom Limb Sensations
Although a normal phantom occurs whenever nerve impulses from the periphery are blocked or otherwise removed, it is also true that direct stimulation of the amputation stump frequently exaggerates the tingling or paresthetic quality of sensation typical of the painless phantom limb. Careful questioning of amputees reveals that the nonpainful phantom limb is not perceived as a static phenomenon. The paresthetic quality of sensation, which defines the phantom limb percept, is in a constant state of flux, with changes occurring in intensity, body part, or both.
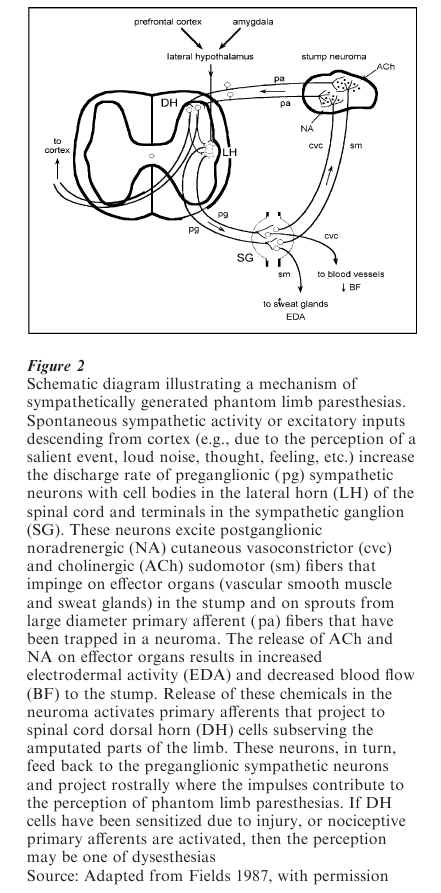
One mechanism that accounts for the paresthetic component of the phantom limb is a cycle of sympathetic-efferent somatic-afferent activity (Katz 2000). Changes in the intensity of phantom limb paresthesias reflect the joint activity of cholinergic (sudomotor) and noradrenergic (vasomotor) postganglionic sympathetic fibers on primary afferents located in the stump and stump neuromas. Release of acetylcholine and norepinephrine from postganglionic sympathetic fibers produces transient vasoconstriction and heightened skin conductance responses. In addition, neurotransmitter release onto apposing peripheral fibers trapped in stump neuromas increases primary afferent discharge. This information is transmitted rostrally, where it gives rise to referred phantom sensations upon reaching central structures subserving the amputated parts of the limb. The moment-tomoment fluctuations in the intensity of phantom limb paresthesias reported by many amputees may, in part, reflect a cycle of sympathetic-efferent somatic-afferent activity. Increases in the intensity of phantom limb paresthesias would follow bursts of sympathetic activity, and decreases would correspond to periods of relative sympathetic inactivity. If central sensitization has also developed, through prior injury, trauma during amputation, or peripheral inflammation, or if the sympathetic-sensory coupling involves nociceptors, the sensation may be one of dysesthesia.
2.4 Psychological And Emotional Processes Influence The Phantom Limb
The idea that emotional and psychological processes can cause pain traditionally has been tied to the notion of psychopathology. However, it is becoming increasingly clear that under certain circumstances pain may be triggered by these processes in psychologically healthy individuals as well. The aggravation or alleviation of pain referred to phantom body parts may be mediated in part by psychological processes that alter anxiety levels. Phantom breast pain after mastectomy is provoked by emotional distress in 6 percent of women three weeks after surgery, and in 29 percent one year later. Of lower-extremity amputees, 50 percent report that attacks of phantom limb pain are triggered by emotional distress as long as seven years after amputation. A combination of progressive relaxation training and Electromygraphic (EMG) biofeedback of stump and forehead muscles produces significant reductions of phantom limb pain and anxiety, which are sustained for up to three years.
Psychological or emotional processes can bring about transient but profound alterations in the quality and intensity of phantom limb sensations. These processes include concentration, distraction, relaxation, fright, forceful reminders of the events that led to amputation, and witnessing cruel and violent acts. One amputee, interviewed by the present writer, described his reaction to an accident involving his wife by reporting ‘goose bumps and cold shivering down the phantom [leg]. It went through me. Everything emotional will get you that.’ Another amputee stated, ‘It’s like everything I feel goes there—the good and the bad’ (Katz 2000).
2.5 A Centrally-Triggered Sympathetic-Efferent Somatic-Afferent Mechanism
The model schematically represented in Fig. 2 outlines a mechanism through which cognitive and affective processes associated with higher cortical and limbic centers may alter phantom limb sensations. The reciprocal connections between cortical, limbic, and lateral hypothalamic structures are well documented. The lateral hypothalamus is involved in the control and integration of neural activity associated with affectively charged behavior, and has direct projections to the lateral horn of the spinal cord. The intensity of phantom limb paresthesias and dysesthesias may thus be modulated by higher brain centers involved in cognitive and affective processes via a multisynaptic network of descending inputs, which impinges on preganglionic sympathetic neurons, producing diffuse peripheral autonomic discharge and activation of primary afferent fibers located in stump neuromas.
3. Summary And Conclusions
The phantom limb is not perceived as a static entity but as a frequently changing perceptual experience dependent upon the current sensory input, emotional state, and past experience of the individual amputee. Phantom limb phenomena range from simple, diffuse sensations of tingling to perceptually complex experiences of pains and lesions that originally were felt in the limb prior to amputation. While phantom pains and other sensations frequently are triggered by the perception of salient events, thoughts, and feelings, there is no evidence that the painful or painless phantom limb is a symptom of a psychological disorder. The sympathetic nervous system may provide an important link between higher brain centers involved in cognitive and affective processes and phantom limb sensations through its peripheral actions on primary afferents located in stump neuromas.
Bibliography:
- Fields H L 1987 Pain. McGraw-Hill, New York
- Jensen T S, Nikolajsen L 1999 Phantom pain and other phenomena after amputation. In: Wall P D, Melzack R (eds.) Textbook of Pain, 4th edn. Churchill Livingstone, Edinburgh, UK, pp. 799–814
- Jensen T S, Krebs B, Nielsen J, Rasmussen P 1985 Immediate and long-term phantom pain in amputees: Incidence, clinical characteristics and relationship to pre-amputation limb pain. Pain 21: 268–78
- Katz J 2000 Individual differences in the consciousness of phantom limbs. In: Kunzendorf R G, Wallace B (eds.) Individual Differences in Conscious Experience. John Benjamins, Amsterdam, pp. 45–97
- Katz J, Melzack R 1987 Referred sensations in chronic pain patients. Pain 28: 51–9
- Katz J, Melzack R 1990 Pain ‘memories’ in phantom limbs: Review and clinical observations. Pain 43: 319–36
- Merzenich M M, Nelson R J, Stryker M P, Cynader M S, Schoppmann A, Zook J M 1984 Somatosensory cortical map changes following digit amputation in adult monkeys. Journal of Comparative Neurology 224: 591–605
- Mitchell S W 1871 Phantom limbs. Lippincott’s Magazine of Popular Literature and Science 8: 563–9
- Nikolajsen L, Ilkjaer S, Krøner K, Christensen J H, Jensen T S 1997 The influence of preamputation pain on postamputation stump and phantom pain. Pain 72: 393–405
- Sherman R A, Devor M, Jones D E C, Katz J, Marbach J J 1997 Phantom Pain. Plenum Press, New York




