View sample alternative medicine research paper. Browse research paper examples for more inspiration. If you need a health research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Abstract
The term “alternative medicine” (AM) is broadly used in the Western world to refer to a group of therapeutic systems and interventions that exist largely outside of the established, conventional healthcare system. In some countries, primarily developing nations, as many as 80 % are said to rely on some form of indigenous AM for their primary healthcare where it is more commonly termed, “traditional medicine.” Elsewhere, demand for AM is high and increasing, in spite of the ready availability of conventional care. Many specific ethical challenges to AM are described here, including issues such as the lack of research evidence for the efficacy of many AMs, the quality control and safety of products, the regulation and competence of practitioners, issues affecting informed choice, and that AM treatment may delay or prevent patients from seeking mainstream healthcare. In addition, ethical considerations that extend beyond the autonomy and well-being of patients and practitioners are considered, including issues such as sustainability, respect for biodiversity, fairness and equity in healthcare, and protection of traditional knowledge and products. The World Health Organization is working closely with countries around the globe to determine how best they can promote health while protecting consumers who wish to use, or rely upon, AM.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
Introduction
The wide-scale use of alternative medicines (AM) and the associated practical and ethical concerns are the focus of attention for the World Health Organization (WHO) in their traditional medicine strategy 2014–2023 (WHO 2013). The range of AMs available includes ancient forms of healthcare such as traditional Chinese medicine, Western herbal medicine, traditional Indian medicine (Ayurvedic), and traditional Arabic medicine (Unani), as well as more recently developed systems such as homeopathy, naturopathy, chiropractic, and osteopathy. While AMs have largely developed independently in their own geographic locality, over extended periods of time, AM products and practices from specific regions are now often found throughout the world making AM a truly global phenomenon (WHO 2013).
According to the WHO, different forms of AM are found in almost every country in the world, and the demand is increasing (WHO 2013). Precise figures for global usage are elusive as demand differs greatly between regions, socioeconomic groups, cultures, and health complaints, even within individual countries. However, estimates suggest that usage may be as high as 80 % in some parts of Asia and Africa where many people rely upon some form of AM for their primary healthcare (WHO 2008). Elsewhere in the world, there is evidence to suggest that demand for AM is high and increasing, in spite of the ready availability of conventional care.
Potentially, there are a myriad of reasons for the popularity of AM, but for those in developing countries, it is often the case that appropriate conventional medicine is cost prohibitive, inaccessible, or simply not available, such that AM treatments are the only available healthcare option. In some localities, people are largely dependent on some form of local, traditional AM for their primary healthcare, utilizing specific types of AM that have a cultural connection and are readily available and affordable. For instance, in Africa, the majority of medical doctors are situated within urban areas and cities, inaccessible by those living in rural areas. Moreover, the ratio of traditional healers to population in Africa is 1:500 compared to a ratio of 1:40,000 medical doctors to population (Abdullahi 2011).
In addition to being cheaper and more accessible, there may be a distinct preference for indigenous forms of healthcare. For instance, traditional African healers may be sought because they offer treatments for the more intangible necessities of health and well-being that are not part of the conventional medic’s toolkit, such as the warding off of evil, bringing luck and good fortune, and protection against demonic attacks.
In China, Korea, and Japan, East Asian medicine predates conventional medicine by several thousand years, is highly valued, and is utilized by 40–76 % of the populations. In these three countries, the East Asian medicine methods of acupuncture, herbal medicine, moxibustion, cupping, and manual therapies are integrated into the national healthcare systems in a manner that is respectful of the historical and cultural background and allows people relatively equal access to both AM and conventional medicine (Park et al. 2012).
In regions of the world where conventional medicine is readily available and more the norm, a substantial number of people are electing to use AM either as an alternative or as an adjunct to conventional care. For instance, in Australia and Europe, as many as 1 in 2 adults have used some form of AM, and in the USA, the figure is estimated at almost 4 in 10 adults. These figures have remained relatively constant in surveys over recent years. Many reasons have been cited for the popularity of AM, such as a dissatisfaction with conventional medicine, a lack of effective conventional medication, the presence of unwanted side effects from conventional care, and a preference for a more holistic or “natural” approach. Individual needs often determine when people use AM, and usage for specific complaints has been well documented showing that different forms are currently being utilized for the treatment of a broad spectrum of both chronic and acute health complaints.
For those in more developed nations, and who can afford it, the choice of healthcare options can be considerable. AM practitioners are easy to find in most countries, and AM products are even more readily available. For example, a person with a chronic complaint such as arthritis or eczema might visit a practitioner such as an acupuncturist or reflexologist or try a range of different AM products, such as herbal remedies or nutritional supplements, either instead of, or alongside, conventional medications. In recent years, there has been a vast increase in the global market for traditional healthcare products and services driven, at least in part, by a desire to supplement or replace the available conventional treatments. The Internet abounds with claims about the effectiveness of such treatments, and many AM products can be obtained and self-prescribed with ease without medical advice or quality control.
As the demand for AM in developed countries has expanded, education and training centers have been established to meet an increasing demand for skilled practitioners. For example, for many years now, it has not been necessary to visit China for training in acupuncture; there are courses available all over the world. In the absence of agreed global standards, educational levels in AM vary considerably across the globe, from well-developed and accredited courses in universities, to short, unregulated courses available online. While many countries are attempting to develop policy and regulation for AM, patterns are inconsistent and vary from country to country. In some countries, AM remains completely unregulated.
The full practical, legal, and ethical implications of the wide-scale use of AMs have only relatively recently become a subject of scrutiny. Many specific ethical challenges to AM have been cited including issues such as the quality control and safety of products, the regulation and competence of practitioners, how to ensure informed choice of patients, the giving of misleading information, and that AM treatment may delay or prevent patients from seeking mainstream “effective” healthcare. These ethical issues clearly call into question the potential for benefit (beneficence) and how to avoid harm (non-maleficence), which in turn must be considered in the light of a person’s right to use their healthcare of choice (autonomy). In addition, there are ethical considerations that extend beyond the autonomy and the well-being of patients and practitioners to embrace issues such as fairness and equity (justice) and sustainability (concern for future generations).
In this research paper, some of the main ethical issues associated with the use of AM will be examined with examples of approaches that are being taken to address the challenges. Firstly, however, an overview of what AM comprises and the differences between AM and conventional medical approaches are provided as context for the ethical considerations.
What Is Alternative Medicine?
The term “alternative medicine” was first popularized in the USA and Europe in the 1970s when it was noted that some people, when given the choice, were electing to use certain unconventional forms of healthcare, also then termed “irregular medicine” or “fringe medicine.” In the late 1980s, the expression “complementary medicine” was introduced in an attempt to present a more accurate reflection of the way in which most people use AM therapies as an adjunct to conventional treatment. Currently, the words “complementary” and “alternative” are often used interchangeably to describe this body of therapeutic systems and frequently designated by the acronym CAM, complementary and alternative, denoting usage either as an alternative to conventional treatment or in a complementary manner. In some circles, AM is also referred to as holistic medicine, natural medicine, or integrative medicine.
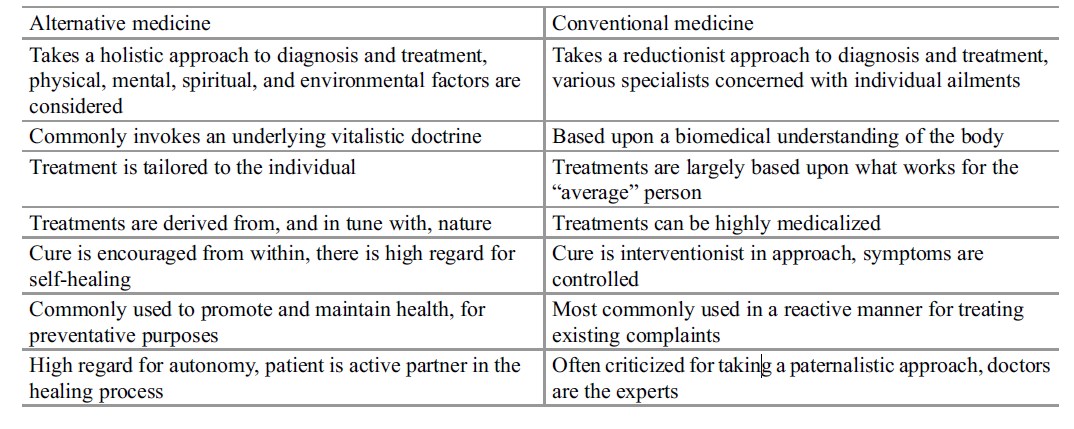
AM is comprised of a broad range of disciplines with diverse medical philosophies, diagnostic methods, therapeutic interventions, and lifestyle approaches that are collectively termed because they are in some way dissimilar to healthcare that is offered by the prevailing healthcare system. AM therapies differ from conventional medicine not only in their methods but also in some of their underlying philosophies. The way that many AM disciplines define health, illness, and the healing process can depart significantly from the beliefs that underlie the practice of conventional medicine. While AM therapies are diverse in nature, there are some common underlying assumptions that apply to most, if not all, AMs and differentiate them from a conventional biomedical approach. Some of the most widely accredited differences in perspective between AM and conventional medicine are summarized in Table 1.
Table 1. Comparison of alternative and conventional medical approaches
The task of defining and categorizing AM has proven to be highly problematic, in part due to the vast array of products and practices but also because the boundaries between what is considered AM and what is considered conventional medicine are often blurred. A precise and meaningful definition of AM is likely to evade consensus; the AM community has been struggling for over 30 years to come up with a single definition that can be broadly agreed. Currently, many different forms of categorization are applied by different AM-associated bodies.
In the USA, the National Center for Complementary and Integrative Health (NCCIH), formerly known as the National Center for Complementary and Alternative Medicine (NCCAM), is the federal government’s lead agency for scientific research and source of government information. NCCIH categorizes AM into two overarching domains, natural products and mind and body practices and one third category of others (NCCAM 2014). According to NCCIH, natural products include substances such as herbs, vitamins and minerals, and probiotics. They are generally widely available and often sold as dietary supplements.
Mind and body practices comprise procedures or techniques administered or taught by a trained practitioner or teacher. Examples include:
- Acupuncture
- Massage therapy
- Meditation
- Movement therapies such as Alexander technique and Pilates
- Relaxation techniques, such as breathing exercises and guided imagery
- Spinal manipulation such as chiropractic and osteopathy
- Tai chi and qi gong
- Yoga
- Hypnotherapy
A third, loose category of other complementary approaches is reserved for approaches that do not fit neatly into either of the above two domains, such as the practices of traditional healers, Ayurvedic medicine, traditional Chinese medicine, homeopathy, and naturopathy.
Unlike most other attempts to classify and categorize AM, the WHO distinguishes between AM that is used in a complementary or alternative manner, away from its geographical origins, and AM that is rooted in local tradition and culture (traditional medicine) in their definition (WHO 2000). According to the WHO, any form of healthcare that is indigenous to a particular locality can be classified as traditional medicine within that locality, but outside that locality may be considered as complementary or alternative. Thus, acupuncture and the use of Chinese herbal medicines should be classified as traditional medicine when used within China but as complementary or alternative medicine elsewhere in the world; what is considered traditional and what is considered AM will vary from country to country and region to region.
In this research paper, the term alternative medicine is used as representative of all forms of healthcare products and services that are not widely regarded as part of conventional biomedicine, whether they are used in a traditional, complementary, or alternative manner.
The Ethical Dimension Of Alternative Medicine
In spite of the potential for benefit, the widespread usage, and apparent acceptance of AM by the general public, discussion about AM can lead to emotionally charged debate. In some parts of the world, there are particularly vocal objectors to the wide-scale usage of AM, and it has variously been described by opponents as a form of “medical heresy,” no better than “superstition,” and “pseudoscientific.”
The primary objection to the use of AM interventions is focused upon the lack of a rigorous evidence base for most types of AM as is required for conventional medical healthcare. The question asked is certainly reasonable: Is it ethical to prescribe treatments that have no scientific evidence of efficacy or safety? No new conventional medications are introduced without rigorous testing through established scientific methods such as clinical trials.
The practice of AM, however, is primarily rooted in case-based, empirical evidence, passed down through generations. This form of knowledge, whether in written or purely verbal form, is subject to testing for effectiveness and safety, only when applied in practice with individuals. For some types of AM, such as Ayurveda, development has taken place over many centuries.
This type of historical evidence does not satisfy those who demand that all healthcare interventions should be rooted in a scientific evidence base. In conventional healthcare, the introduction of evidence-based medicine (EBM) in the late 1980s was heralded as revolutionary. The notion of EBM is predicated upon the assumption that there is a hierarchy of evidence for medical interventions, such that certain types of evidence are deemed of greater value than others. At the top of this hierarchy are placed results from randomized controlled trials (RCTs) and systematic reviews or meta-analyses of these trials. The synthesis of large amounts of clinical trial data into manageable systematic reviews or meta-analyses is designed to offer objective and politically transparent criteria for treatment choice and funding decisions. Since the broad adoption of EBM principles, there has been increasing pressure on all forms of AM to provide the kind of evidence that is deemed of high value from RCTs and reviews of these trials, to enable comparative assessment of efficacy and safety. Without this type of evidence, most governments are unwilling to fund provision, research, or development of AM on anything but a small scale.
In response to the demand for an evidence base, attempts have been made to conduct the type of clinical trials that are considered of high value, but in so doing, many challenges have been identified by AM researchers including the claim that the RCT can never be an adequate test for the complex and holistic nature of AM as treatments are rarely targeted at a specific symptom or complaint.
The greatest challenge for AM research, however, is undoubtedly the scarcity of research funding. Government, charitable, and private funding for research into AM is low with the result being that research funding for AM is vastly out of proportion to the prevalence of AM use. This can be seen clearly in the USA where funding for NCCIH activity in 2013 amounted to $123.813 million, while total funding of health research and development activity in the USA amounted to $330383 million in 2012 (Research America 2014), suggesting that NCCIH funding is equivalent to less than 0.1 % of all medical research funding.
The funding for wide-scale AM research, of the type that would be needed to develop a robust evidence base, is simply not available. Some argue that it would be unethical to provide funds for investigation of products and services, deemed implausible, as funding research in these circumstances would constitute a waste of resources. Hence, to a large degree, there is currently a stalemate position on the issue of evidence in AM; on the one hand, AM is criticized for not having a robust evidence base, and on the other, AM research is denied funding.
Argument is ongoing about what constitutes reliable evidence and how that evidence might be assembled as can be seen in Table 2 which summarizes the contrasting polarities of opinion in the debate about evidence.
Table 2. Contrasting opinions on evidence for effectiveness of AM
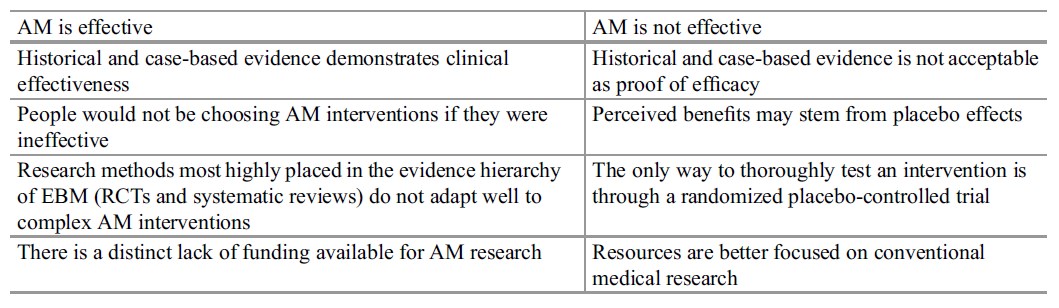
Clearly, the above two positions cannot be easily reconciled, and the debate about efficacy remains unresolved in most areas of AM. However, if it is to be deemed unethical to use medicines and interventions that do not have a robust research evidence base, then much of conventional medicine will be removed from use. Estimates vary widely (from 11 % to 70 %) as to the exact proportion of conventional interventions that are robustly evidence based.
Regardless of whether or not the available evidence is sufficient to meet the requirements of evidence-based medicine, the current global demand for, and reliance upon, AM needs to be acknowledged and respected. Patient autonomy, especially in the developed world, is highly valued in healthcare, as is evidenced by the trend toward patient-centered medicine and patient choice. Many patients exercise their right to choose their preferred healthcare options by using AM treatment either as an adjunct or alternative to conventional care. In the developing world, many people rely upon AMs for their primary source of healthcare either because they are culturally more acceptable or because they are the only form of healthcare that is affordable/available. Given that much of AM is under-researched in terms of efficacy, safety, and cost-effectiveness, this inevitably generates ethical concerns. In addition, the practice of AM has largely existed as an independent, parallel, and disparate healthcare system, and professional standards are extremely variable. As the complexities of this situation become better understood, clear specific ethical challenges are highlighted that demand attention. The following examination of ethical issues is divided into sections relating to the ethical principles of beneficence, non-maleficence, autonomy, concern for future generations, and justice.
Beneficence And The Potential For Benefit Of Alternative Medicine
The value of the contribution that AM makes to global health should not be underestimated, as emphasized by the WHO Director General, Dr Margaret Chan, who, when addressing the International Conference on Traditional Medicine for Southeast Asian Countries in 2013, declared that:
Traditional medicines, of proven quality, safety, and efficacy, contribute to the goal of ensuring that all people have access to care. For many millions of people, herbal medicines, traditional treatments, and traditional practitioners are the main source of health care, and sometimes the only source of care. This is care that is close to homes, accessible and affordable. It is also culturally acceptable and trusted by large numbers of people. The affordability of most traditional medicines makes them all the more attractive at a time of soaring health-care costs and nearly universal austerity (As cited in WHO 2013).
Aside from any direct medicinal benefits of AMs, there are broader benefits of potentially immense proportion.
Herbal medicines in particular contribute directly to the development of conventional medications with as many as one-third to one-half of pharmaceutical drugs being derived from plants (Abbott 2014). These include many widely used forms of medicine, for example:
- Taxol, an antitumor agent that is derived from Taxus brevifolia (Pacific yew)
- Morphine and codeine, widely used analgesics that are derived from Papaver somniferum (poppy)
- Digoxin, a cardiotonic that is derived from Digitalis purpurea (purple or common foxglove)
- Quinine, an antimalarial drug that is derived from Cinchona ledgeriana (quinine tree)
Economic benefits are significant for some countries where AM is an important source of income for many individuals and communities. According to the WHO (2013), the AM sector now plays a significant role in the economic development of a number of countries. This is highly evident in China, for example, where global promotion of TCM services and products has been used to foster economic development generating billions of US dollars in revenue annually (Abbott 2014).
A further noteworthy benefit, highlighted by the WHO (2013), is that AMs are very often used for disease prevention, to enhance and maintain health. Appropriate use has the potential to make AMs highly cost-effective, helping to reduce pressure on healthcare systems by reducing overall costs. This is a particularly vital consideration given burgeoning healthcare costs and the growing need for development of sustainable forms of healthcare.
Non-Maleficence And The Safety Of Alternative Medicine
Safety issues in AM fall broadly into two categories:
- Issues pertaining to the safety of the product
- Issues pertaining to the safety of the practitioner
Concerns about the safety of AM products are primarily focused upon herbal products and other dietary supplements, whether prescribed by a practitioner or self-medicated.
Concerns about the safety of practitioners apply to all forms of AM and include issues such as education and regulation, working within bounds of competence, provision of reliable information, and integration with other forms of healthcare.
Both categories of safety issues are equally as important; they can both lead to potentially life-threatening situations, and each will be addressed here in more detail.
The Safety Of Alternative Medicine Products
For herbal medications in particular, it may be reasonable to assume that ancient and extensive use will inevitably reveal safety implications. Information about who might be at risk, how much to take, and potential side effects is gleaned from years of real-world experience and guidance developed accordingly. This type of information evolves as it is passed down through generations and is vital to locally based, traditional forms of AM for effective healthcare. However, when products are removed from their cultural and traditional roots and applied in completely different environments, under different conditions and in different formats, the consequences of such use are unpredictable. Such was the case for kava kava (Piper methysticum). For over 3,000 years, the people of the South Pacific Islands have been using kava kava for medicinal, religious, and social purposes. There is a great local respect for this plant that holds deep cultural significance. In Fiji, for example, the kava kava ceremony often accompanies important occasions when the root of the plant is chewed or pounded, then mixed with water, strained, and drunk. The effects of the kava kava are sedative and have been likened in some respects to alcohol. Following reports of great benefits, the leaves and the root of the kava kava plant were used to make herbal products that became popular in many other parts of the world for treatment of anxiety, tension, insomnia, and restlessness. Clinical studies backed up the efficacy claims for the use of kava kava in the treatment of anxiety.
In 2001, concerns were raised about the safety of kava kava after a number of cases of acute liver failure were reported, leading to restrictions, regulations, and outright bans in some countries. Kava kava, it appears, has highly beneficial properties, but it also has the potential for hepatotoxic effects in certain individuals. More research has been needed to identify the precise requirements for safe use of kava kava.
In the UK, warnings about herbal medicines are published and regularly updated on the website of the Medicines and Healthcare Products Regulatory Agency (MRHA 2014). A glance at entries in November 2014 reveals the following additions:
- Warning about Ayurvedic herbal medicine for treatment of asthmatic symptoms containing undeclared pharmaceuticals
MHRA is advising consumers not to use Ayurvedic herbal medicine Shwasa Sanjeevani as it has been found to contain dexamethasone, a prescription-only medicine which has not been declared on the packaging.
- Warning about slimming pills containing undeclared pharmaceuticals
MHRA is advising consumers not to use specific slimming pills as these products have been found by regulators in other countries to contain prescription-only drug ingredients that are not declared on the product labels.
- Warnings about unlicensed traditional Chinese medicines containing undeclared pharmaceuticals and heavy metals
The MHRA is advising consumers not to use the following traditional Chinese medicines as there are concerns about possible side effects. These products are not authorized for sale in the UK and have not been found on the UK marketplace, but they could be available on the Internet.
It is clear, from these examples, that the potential for harm from unlicensed and unregulated AM products is pervasive and multifactorial. Potential for harmful effects stems not only from toxicity associated with poor quality, adulterated, or contaminated products but also from the possibility of overdose, side effects, drug/herb interactions, and interference with biological tests even from high quality herbal products. Many plants are potent or toxic, and there is typically far less safety data available for herbal products than would be required for conventional medications. Hence, there are two broad requirements pertaining to the safety of AM products. Firstly, AM products require quality control and licensing on a global scale, and secondly, more safety data is needed to assess toxicity levels, appropriate dosage, likelihood of side effects, and potential for interactions with other medications.
Worldwide, there is increasing scientific study of herbal medicines together with improved sharing of information between regulators. The WHO is taking a proactive role in driving forward the development of policies and regulation of herbal products. According to the WHO, most Member States now regulate herbal products, although new regulations are continually being developed, updated, and implemented. These regulatory approaches are aimed at protecting consumer health by ensuring that medicines are safe and of high quality. As the market is now truly international with products often being made in a country other than that in which they are sold, it is acknowledged that it may be a challenge to ensure products are safe and of high quality. In order to address this issue, Member States and regulatory agencies are cooperating and learning from each other’s experiences. Some regional bodies have been working on harmonizing regulations on herbal medicines and other herbal products within their region (WHO 2013). It is therefore anticipated that over time, levels of safety of AM products will improve, but in the meantime, caution must be urged, particularly in the use of products from unregulated sources.
Safety And Alternative Medicine Practitioners
While rare, over the past 20 years, there have been reports emerging of serious consequences for some who have opted to use AM treatments. Some forms are deemed more risky than others such that incompetence on the part of the practitioner could lead to serious adverse effects. For example, chiropractic and osteopathy carry a risk of trauma and injury; acupuncture also carries this risk together with potential for infection, and herbal medicines can be misprescribed.
Aside from the potential direct adverse effects of incompetent practice, there are also indirect risks that are of a more intangible nature. Misdiagnosis, delayed diagnosis, and failure to use effective treatments can have fatal consequences. In addition, practitioners can do harm through inappropriate advice, provision of misleading information, lack of professional boundaries, and poor standards of care.
Children can be put at risk when parents opt for AM treatments as was tragically highlighted by the deaths of four children in Australia in 2010 that were reported to relate to a failure to use conventional treatment. One case involved an 8-month-old infant admitted with malnutrition and septic shock following naturopathic treatment with a rice milk diet for “congestion.” Another death was of a child who was prescribed anticoagulants following pulmonary emboli but was treated with a complementary medicine instead. The child died following complications relating to a pulmonary infarction.
Undeniably, concerns about incompetence and malpractice can also apply to practitioners of conventional medicine; being qualified to practice conventional medicine is no assurance of complete safety. Mistakes are made by health professionals on a routine basis; in the USA, deaths from medical errors have been estimated to be as high as 440,000 per year. However, the professions associated with conventional medicine have rigorous educational, professional, and ethical standards in place that are designed to protect the wellbeing of the patient and help to minimize risks. Unfortunately, the same cannot be said of all AM professions.
The application of similar standards in AM practice would help to minimize practice risks by enforcing appropriate safety standards, but, according to the WHO, AM practice varies widely from country to country. Member States currently diverge to an extraordinary degree with regard to levels of education, accreditation, and regulation of practices and practitioners, but the situation is improving. In line with attempts to regulate products, many Member States have been making great efforts to advance, establish, or develop national and regional policies and regulations to promote the safe and effective use of AM. In the period 1999–2012, the number of Member States with an AM policy rose from 65 to 119, while the number regulating herbal medicines more than doubled, rising from 25 to 69 (WHO 2013).
Educational standards may prove more challenging to harmonize. In some countries, knowledge and skills of indigenous forms of AM have been transferred from generation to generation through an oral tradition. In other countries, training in AM takes place in universities at bachelors, masters, and doctoral levels. Even across neighboring regions, there are wide variations. For instance, in Europe, the education and training of AM practitioners differ greatly from country to country, and in some countries, it is illegal for non-medics to practice AM. The fact that AM can be practiced by traditional healers in some countries, conventional healthcare professionals in others, or people who have been specifically trained in an AM discipline in other situations means it is virtually impossible to enforce universal educational standards. Individual countries therefore need to make pragmatic decisions about the level of education and training necessary for each type of AM practitioner in order to best safeguard the public.
Autonomy And Alternative Medicine
In simple terms, the principle of respect for autonomy in healthcare is normally associated with allowing or enabling patients to make their own decisions about which healthcare interventions they will or will not receive. It is a principle that has been awarded increasing attention over the last 30 years, particularly in developed nations, but in practice, the application of this principle can be challenging. For example, there are times when respect for patient autonomy conflicts with a health practitioner’s opinion about potential for benefit and harm in all forms of healthcare, conventional as well as AM. Decisions about when it is appropriate and ethical to overrule autonomy in favor of well-being are complex and involve many factors. Overprotection can infringe upon patient choice invoking paternalism; underprotection can lead to harm. The way in which these two factors are kept in balance varies between countries and practices, but there is general agreement that, as far as possible, individuals must be informed about the likely benefits and risks of using any forms of treatment, whether AM or conventional.
Making An Informed Choice About The Use Of Alternative Medicine
An absence of data regarding efficacy and safety, together with widespread variation in standards of education and regulation, will inevitably affect an individual’s ability to make an informed choice about treatment options.
Informed choice is broadly accepted as one of the cornerstones of good healthcare practice. It involves the exchange and understanding of relevant information so that a knowledgeable, reasoned, and unpressured decision can be made. It is vital that people are neither deceived nor coerced when making decisions about their healthcare. Informed choice is a necessary ingredient for patient autonomy, and it relies upon accuracy and reliability of information. If there is a paucity of research evidence available to support the use of certain treatments, then individuals should be informed that this is the case. The reliability of claims that are made for some AM products and services has been seriously questioned, especially those advertised via the Internet as they are extremely difficult to police. Here, the onus falls upon the AM community to improve on ways in which they inform people about its products, practices, and practitioners and avoid unsubstantiated claims.
Individual Versus Community Choice
In some cultures, decisions about healthcare are not primarily a matter of individual autonomy because the well-being of the community is more highly valued than that of the individual. For example, many African cultures operate through tightly bound communities that have their own core values and their own modus operandi. The elders of such communities are often the holders of the power and make decisions on behalf of, and for the good of, the community as a whole. In these circumstances, personal choice and informed consent are not highly valued, and paternalism may be the norm. Inevitably, increasing globalization is leading to a degree of erosion of certain long held traditions, and the situation may be changing, but without the resources to bring conventional medicine into the poorer and more rural areas, choice in healthcare will remain a luxury that many cannot afford.
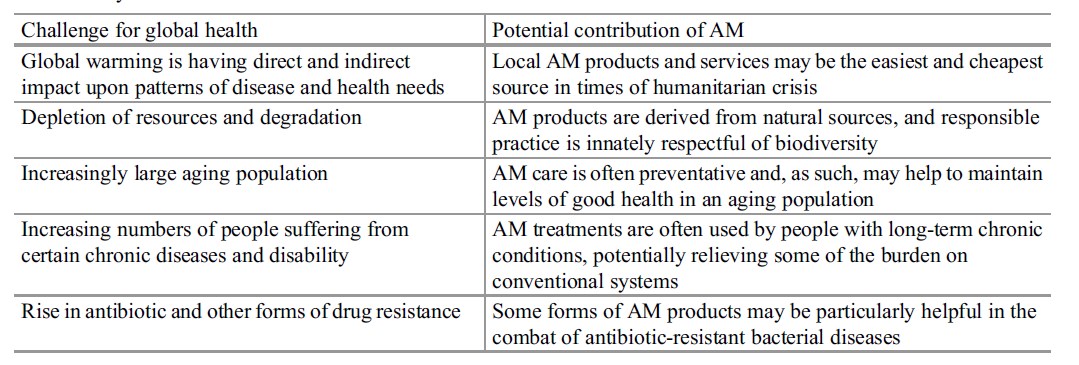
Sustainable Healthcare And Alternative Medicine
At a time when the whole world is facing considerable threats to health and well-being, with healthcare systems that are largely unsustainable, dramatic changes may be needed in order to avoid a crisis in healthcare provision. Conventional healthcare approaches are notoriously costly in terms of resources and detrimental environmental impact. The predominance of curative, hospital based, disease-oriented services has been described by the WHO as “top-heavy services,” responsible for huge inefficiencies that could be redirected toward achieving universal health coverage (WHO 2013). Here, the WHO proposes that the use of AM could make a positive contribution to universal health coverage. The full potential for AM requires further investigation, but Table 3 details some areas of potentially fruitful contribution.
Table 3. Challenges for global health and the potential contribution of AM to a sustainable healthcare system
Justice And Alternative Medicine
In countries such as China, Japan, and Korea, there is relatively equal access to both conventional and AM treatments in an integrated healthcare system. Elsewhere, however, equity issues associated with AM use are a cause of concern both for the availability of conventional medicine for those who only have access to AM and for those with a preference for AM treatment who cannot afford to pay for it. In most countries, people pay out of pocket for AM treatments, and in developed nations, AM use is mostly associated with higher income and educational levels. Genuine choice in healthcare options is largely the privilege of an elite group.
In both developing and developed countries, the poor may sacrifice basic needs such as food and education in order to pay for healthcare. In developing countries, those who cannot afford to pay for properly regulated AM treatments may be forced to purchase unregulated products from unlicensed vendors. In developed countries, ethnic minorities often continue to use traditional forms of AM from their culture even when conventional medicine is free of charge (Bodeker and Burford 2007). Clearly, there are global concerns about equity in healthcare as patient choice is limited by availability and affordability.
A further great concern for developing countries is the potential for misappropriation of natural resources and preservation of biodiversity. For instance, Artemisia annual grown in Tanzania is exported to Europe for processing antimalarial drugs and the resulting products reimported for over 6 dollars per dose which is out of reach of most of the people who need them (Bodeker and Burford 2007). Consequently, there has been a great drive toward greater protection of traditional knowledge and products. This is proven to be problematic. Modern notions of intellectual property often conflict with traditional systems of knowledge ownership, and current intellectual property regimes were not designed to accommodate traditional knowledge. Many experts have claimed that conventional patent laws are inadequate to protect traditional knowledge and biodiversity (Abbott 2014).
The WHO (2013) stresses the importance of balancing the need to protect the intellectual property rights of indigenous peoples and local communities and their healthcare heritage while ensuring access to AM and fostering research, development, and innovation. They advise that adequate protection of AM through conventional intellectual property or sui generis rights can help prevent its unauthorized use.
This in turn, they say, as well as encouraging innovation, is likely to protect traditional knowledge that might otherwise be lost.
The Best Of Both Worlds
The WHO traditional medicine strategy 2014–2023 has been developed to help countries determine how best they can promote health and protect consumers who wish to use AM. In their strategy, the WHO clearly specifies that individual Member States will need to develop national approaches that reflect their specific needs in dealing with the most popular forms of AM practiced in their country. This will not be a case of “one size fits all,” but given that AM products and practices from one region may be used throughout the world, cooperation will be needed between Member States as the sector continues to work on supporting access to safe products and practices. Essential for this process, the WHO suggests, is that AMs are properly integrated into national health systems to enable consumers to have a wider choice when they wish to use such services (WHO 2013), a vision that is, as yet, far removed from the systems in most countries.
The preference for, and use of, one type of medicine over another is not in itself an ethical problem; the danger comes from overreliance on any one type of healthcare to the exclusion of all others. Many of the potential risks of AM stem from the notion that a particular modality can be the alternative, that it is the best and the only thing necessary for cure. Rather than treating healthcare decisions as an “either-or” situation, an ideal, patient-centered solution would be to treat all forms of healthcare as complementary. Each has their own strengths and weaknesses, and no one type of medicine is the best for all people in all situations.
Appropriate integration of healthcare systems has the potential to offer the best of both worlds. As suggested by Dr Margaret Chan (2008):
The two systems of traditional and Western medicine need not clash. Within the context of primary health care, they can blend together in a beneficial harmony, using the best features of each system, and compensating for certain weaknesses in each. This is not something that will happen all by itself. Deliberate policy decisions have to be made. But it can be done successfully
Conclusion
In many respects, the ethical challenges facing AM are the same as those facing conventional medicine: how to ensure beneficial, safe, and cost-effective treatment while respecting patient choice and broader considerations such as sustainability.
AMs are regularly used in almost every country of the world and relied upon by many, but the amount of research funding available is disproportionate to this use, being a tiny fraction of total spending on healthcare research. Consequently, the data needed for adequate assessment of benefits, safety, and costs is simply not available for most types of AM.
Given that AM makes such an important contribution to global health, the WHO is attempting to drive forward the development of regulation and policies regarding AM in all Member States. Much is already being done to improve standards in products and care.
There are an enormous variety of AMs globally, many with untapped potential. With burgeoning healthcare costs and the growing need for development of sustainable treatments, care must be taken to preserve traditional products and knowledge.
Bibliography :
- Abbott, R. (2014). Documenting traditional medical knowledge. World Intellectual Property Organization. http://www.wipo.int/export/sites/www/tk/en/resources/ pdf/medical_tk.pdf.
- Abdullahi, A. A. (2011). Trends and challenges of traditional medicine in Africa. African Journal of Traditional, Complementary and Alternative Medicines, 8 (5S):115–123.
- Bodeker, G., & Burford, G. (2007). Traditional, complementary and alternative medicine: Policy and public health perspectives. London: Imperial College Press.
- Chan, M. (2008). Address at the WHO congress on traditional medicine, Beijing, November 2008. Geneva: World Health Organization.
- NIH. (2014). Complementary, alternative or integrative health: What’s in a name? https://www.nccih.nih.gov/health/complementary-alternative-or-integrative-health-whats-in-a-name
- Park, H. L., Lee, H. S., Shin, B. C., Liu, J. P., Shang, Q., Yamashita, H., & Lim, B. (2012). Traditional medicine in China, Korea, and Japan: A brief introduction and comparison. Evidence-Based Complementary and Alternative Medicine. Article ID: 429103. doi:10.1155/2012/429103.Bodeker, G., & Burford, G. (2007). Traditional, complementary and alternative medicine: Policy and public health perspectives. London: Imperial College Press.
- UK Herbal Medicines Advisory Committee (HMAC) (2014). Safety, regulation and herbal medicines: a review of the evidence. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/545681/HMAC_-_HerbalsafetyOctober2014Final.pdf
- WHO. (2013). WHO traditional medicine strategy: 2014–2023. Hong Kong SAR: World Health Organization.




