Sample Health In Developing Countries Research Paper. Browse other research paper examples and check the list of research paper topics for more inspiration. If you need a research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our custom research paper writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Human health and wellbeing worldwide are profoundly affected by complex interactions between economic, social, and political forces as well as by behavioral patterns and the application of technology (Wilkinson 1996). When considering health in countries around the world, use of the terms ‘developed’ and ‘developing’ countries implies a linearity of progress towards a condition that has been achieved by some countries but not others. It is clear that such a simplistic approach equating development with economic status in terms of average per capita gross national product (GNP) or the level of industrialization is both inaccurate and unhelpful. So-called developed countries may lack what many would consider very important aspects of development; for example, a sensitivity to the impact of consumption on ecology, or concern for the adverse effects of opulent and aggressive lifestyles on billions of people in other countries, or more obviously in relation to health, the achievement of universal access to health care. Similarly, some so-called developing countries are more developed than may be apparent from their economic status; for example in Kerala, India, the degree of social solidarity and health status achieved exceeds that expected from economic status alone—revealing the impact of human capital resources such as female literacy and empowerment.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
A more sophisticated model of development (such as that used in the United Nations Human Development Report 1991) emphasizing achievements in health, education, female literacy, gender equality, and political liberty, more accurately reflects the real human development required. However, it should be acknowledged that even such development indices are incomplete, as they do not measure some important aspects of human flourishing. When comparing development and health in countries around the world, it is also necessary to appreciate that consumption patterns and the ways of life in industrialized countries cannot become the norm for the whole world. For example, while the world’s population has grown fivefold in the past 150 years, human consumption has increased 30-fold. The USA, with 5 percent of the world’s population, accounts for 24 percent of annual global energy consumption compared to China with 20 percent of the world’s population using 10 percent. Within health care, even a nation that spends $4,000 per person per year on health care cannot afford to provide access for all citizens to all that modern medicine can offer (Iglehart 1999). Modern consumption patterns and health care practices are thus neither universalizable nor sustainable. Such considerations reveal the inadequacy of the terms ‘developed’ and ‘developing’ countries.
1. A Polarized World
While the twentieth century is considered by many to be the most successful in world history, with spectacular achievements in science, technology, and health care, the above considerations make it necessary to focus on the down side of progress—as reflected in widening disparities in economic and health status, the extent of expenditure on weapons of mass destruction, and the social construction of human rights abuses. Improvements in human health globally in the twenty-first century and achieving real development of all people throughout the world will be dependent on acknowledging such adverse features of modern life, and on developing new paradigms of thinking that will promote widespread human flourishing.
1.1 Economic Disparities
At the beginning of the twentieth century the wealthiest 20 percent of the world’s population were nine times richer than the poorest 20 percent. This ratio has grown progressively—to 30 times by 1960, 60 times by 1990, and to over 70 times by 1997. The extent of absolute poverty has also increased. Today almost half the world’s population lives on less than US$2 per person per day and more than a billion people live on less than US$1 per day. Tens of millions of people, including many children, die every year of starvation—in a world with enough food to feed all.
1.2 Disparities In Health And Disease
At the end of the twentieth century patterns of diseases and of longevity also differ markedly across the world. Of the approximately 52 million people who die each year, 17.5 million die of infectious and parasitic diseases (16 million of these—many in their youth—in the developing world), 10 million die of diseases of the circulatory system (4.5 million of these in the developing world), and 6 million die of malignant diseases (3.5 million of these in the developing world) (see Table 1).
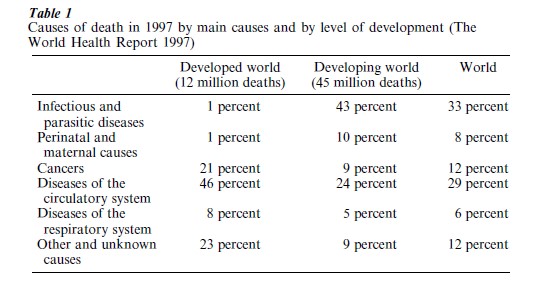
Among the poorest quintile of people in the world, 55 percent die of communicable diseases, as compared with 5 percent of the richest. The World Health Organization (WHO) estimated that in 1998, 11 million children and adults of working age died of six infectious diseases that could have been prevented at the cost of US$20 per life saved. Poor countries bear over 80 percent of the global burden of disease in disability adjusted life years (DALYs). This burden is likely to increase as the epidemiological transition progresses, with added disability and suffering from noncommunicable causes of disability such as vascular disease, malignant neoplasms (especially of the lung associated with smoking), neuropsychiatric disease, accidents, and trauma.
Life expectancy at birth ranges from well over 70 years in highly industrialized countries to below 50 years in many poor countries. Wide disparities in life expectancy are also observed between rich and poor in rich countries. In sub-Saharan Africa gains in longevity achieved during the first half of the twentieth century are rapidly being reversed by the HIV AIDS pandemic.
1.3 Mental Health
Improvements in physical health over the past 50 years have not been matched by improvements in mental health—even in developed countries. Mental illness accounts for 8 percent of the global burden of disease (measured in DALYs), and a further 34 percent of the global burden of disease is accounted for by behavior related problems such as violence, diarrhoeal diseases, AIDS and other sexually transmitted diseases, and motor vehicle accidents and other nonintentional injuries (Desjarlais et al. 1995). The inadequacy of the knowledge base about mental disease (compiled almost exclusively in North America and Europe) to explain psychiatric diseases in other parts of the world poses formidable challenges for progress.
1.4 Militarization And The Social Construction Of Human Rights Abuses
Industrialized countries spend on average 5.3 percent of GNP on the military but only 0.3 percent on economic aid to developing countries (Sivard 1996). The arms trade and its link to economic aid has contributed significantly to the escalating number of wars, conflict, and widespread torture since the Second World War which have rendered over 25 million people to refugee status and displacement—with profound disruptive effects on life and health. Global military expenditure in 1990 amounted to US$1 trillion (Sivard 1996). The annual budget of the WHO is equivalent to 2.5 hours of global military expenditure. While money is always available to make war, it is less readily available to promote peace. Military expenditure has decreased in recent years, but released resources have not been channeled towards effective human development processes.
2. Relationship Between Economics And Health
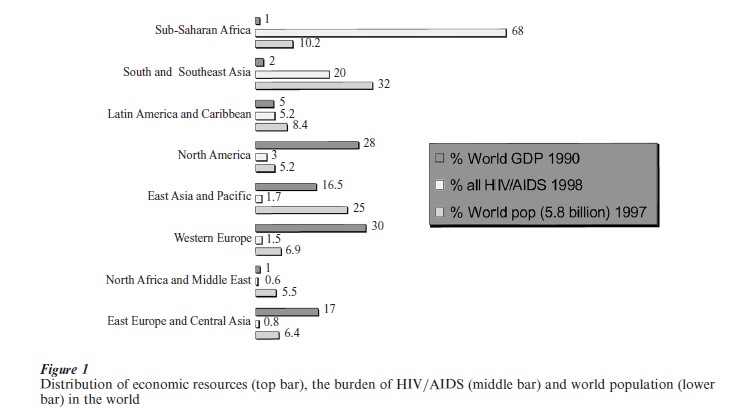
It is now well established that there is a definite relationship between wealth poverty and health disease, although this relationship is complex and not linear. For example, one of the wealthiest nations in the world (the USA) has worse health statistics (infant mortality and longevity) than some other highly industrialized countries, and a particularly poor state (Kerala) in India has achieved lower infant mortality rates and greater longevity than many wealthier nations (Wilkinson 1996). Both absolute and relative wealth affect health. Among the developed countries it is not the richest societies that have the best health, but rather those with the smallest income differentials between rich and poor (Wilkinson 1996). Despite the nonlinearity of the relationship between wealth and health, its existence underscores the need to see health and disease as intimately linked to social and economic conditions (Fig. 1).
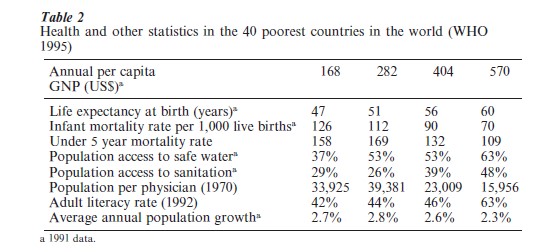
Poverty (defined as lack of economic resources, lack of education, lack of access to basic life resources such as food water and sanitation, and lack of control over the reproductive process) directly accounts for almost one-third of the global burden of disease. Poverty leads to poor health, which in turn aggravates poverty. Of the 40 poorest countries in the world, 11 have annual per capita GNPs ranging from US$80 (Mozambique) to US$210 (Sierra Leone), 10 from US$220 (Bangladesh) to US$340 (Nigeria), 9 from US$370 (China) to US$450 (Nicaragua), and 10 from US$500 (Sri Lanka) to US$600 (Zimbabwe) (WHO 1995). The relationship between income and some health indicators for these groups are shown in Table 2. Despite the difficulty in making accurate intercountry comparisons, it is clear that improvements in economic status are associated with better health statistics, and that economic growth is necessary to improve the living conditions conducive to good health, independent of benefits that may arise directly from health care.
3. Health Care Expenditure
Since the 1960s, major advances in medicine and technology have been associated with escalating expenditure on their application in health care—most of this in highly industrialized countries. Annual per capita expenditure on health care ranges from $4,000 in the US to less than $5 in the poorest countries in Africa. Half the world’s population lives in countries that cannot afford annual per capita health expenditures of more than $5–10, and many people do not have access to even basic drugs. The WHO has estimated that in 1990 the annual cost of providing a basic package of public health and essential clinical services in a low-income country was at least $12. In most such countries health care expenditure is typically less than $6. Even though some parasitic diseases (for example, onchocerciasis, schistosomasis, and lymphatic filariasis) could be controlled by mass treatment campaigns using inexpensive drugs, the infrastructure required to provide such coverage is inadequate. Effective treatment of diseases such as tuberculosis and leprosy, and HIV AIDS requires more complex infrastructures than can be afforded on current health care budgets in poor countries.
In the 1990s, 89 percent of annual world expenditure on health care was spent on 16 percent of the world’s population who bear 7 percent of the global burden of disease (in DALYs) and less than 10 percent of medical research expenditure was on health problems of the developing world. These are examples of global injustice that we should surely find intolerable if we have a real commitment to universal human rights and human dignity. Vaccine development programs and drug donation programs for poor countries, admirably promoted and supported by pharmaceutical companies, are necessary but insufficient responses to such injustices. Modest increments in economic status combined with a provision of a basic health care package have the potential to improve health in poor countries significantly. However, it should be noted that health is not merely a resource issue even in rich countries—as exemplified by comparative health statistics around the world (Wilkinson 1996).
4. The Global Political Economy And Health
The world at the end of the twentieth century is thus characterized by widening disparities in economic and health status (within and between countries), and by suffering, conflict, and alienation associated with pervasive social forces (Wilkinson 1996, Sivard 1996, Benatar 1998). Erosion of the economy of many poor countries, under the impact of globalization and the ‘debt trade,’ has obstructed the introduction of effective forms of modern medicine into many poor countries and thus prevented achievement of widespread access to even basic health care for billions of people (Falk 1999). Third world debt requires special mention. The ways in which such debt have been created, the fact that third world debt is a small component of total world debt and can never be repaid, and that in sub-Saharan Africa four times as much is spent on debt repayment each year than on health and education combined, makes insistence on repayment unconscionable (Pettifor 1996).
The emergence of new diseases such as AIDS, that afflict predominantly those marginalized by poverty (80 percent of HIV-positive persons live in the poorest countries in the world), has been attributed to the social and environmental niches created by the nature of the global political economy and its ideology (Lee and Zwi 1996). Failure to appreciate such associations will result not only in failure to control such diseases as HIV AIDS (as with tuberculosis in the past, Benatar 1995), but more importantly, will probably favor the emergence of new infectious diseases in the future. The changing spatial dimensions of human relations resulting from urbanization, migration, travel, ethnic conflict, and displacement of people and refugees, facilitates the spread of such diseases from which no one should feel immune.
5. Access To Health Care, And The Nature Of Health Care Systems
Today many countries consider access to at least a minimum package of health care as a basic human right that nation-states should be committed to providing for their citizens. Some form of socialized and equitable health care is provided in all Western European nations and in Canada.
Medical care, delivered as a marketable commodity—albeit with considerable state assistance for the poor and the aged—is the example that has been set by one of the wealthiest nations in the world. However, this results in many citizens having inadequate access to health care. In considering how to overcome this, while recognizing that private public alliances cannot be avoided and indeed may be beneficial, Buchanan has provided cogent arguments for the nine elements he considers essential for a just health care system. He argues further that achieving a just health care system as a cooperative between the public and private sectors requires an organization, such as the state, to act as a coordinator and guarantor of equitable access to care and fair distribution of costs. Such a balance between private and public medicine with appropriate coordination could over-come the deficiencies of either system when one dominates (Buchanan 1995; see also Benatar 1996).
The effects of intensive privatization, aided and abetted by the structural adjustment programs promoted by the International Monetary Fund (IMF) and the World Bank, have been much more marked in poor countries, with severe adverse effects on health. Acknowledging the need for, and the right to, universal access to a basic health care package and achieving this goal pose challenges for the future. The WHO’s renewal strategy for health-for-all places emphasis on equity, solidarity, and appropriate technical, political, and economic strategies that could promote health and sustainable health care systems as central to development. Here too an appropriate balance needs to be struck between public and privately funded medicine. How this balance can be struck and how health can be coordinated within an effective strategic alliance between many parties remain hotly debated subjects.
6. Traditional Healers
Despite the pervasiveness of Western influences, traditional healers have survived and play an increasing role in some countries. For example, while there are about 25,000 Western trained medical practitioners in South Africa, and Western medicine has a powerful foothold in this middle-income country, over 200,000 traditional healers carry out a thriving trade. Increasing contact and collaboration between Western medicine and traditional healers is being encouraged and the potential impact of their contributions to health, in particular through development of a primary health care approach, in many countries in Africa in the future should not be underestimated (Van Rensburg and Benatar 2000).
7. Prospects For The Future
As we stand at the threshold of a new era in which exponential increments in genetic information will be applied to medical practice, we need to contemplate whether such new power will be used for the benefit of all humankind or whether it will be reserved for the privileged. Acquiring a deeper understanding of the forces promoting health and diseases in developing countries needs to be coupled to a commitment to address these if health and human flourishing are to be achieved on a wider scale (Benatar 1999).
Bibliography:
- Benatar S R 1995 Prospects for global health: Lessons from tuberculosis. Thorax 50: 487–9
- Benatar S R 1996 Editorial on Buchanan (1996). British Medical Journal 313: 1567–8
- Benatar S R 1998 Global disparities in health and human rights. American Journal of Public Health 88: 295–300
- Benatar S R 1999 A perspective from Africa on human rights and genetic engineering. In: Burley J (ed.) The Genetic Revolution and Human Rights. Oxford Amnesty Lectures. Oxford University Press Oxford, UK, pp. 159–89
- Buchanan A 1995 Privatization and just health care. Bioethics 9: 220–39
- Desjarlais R, Eisenberg L, Good B, Kleinman A 1995 World Mental Health: Problems and Priorities in Low-income Countries. Oxford University Press, New York
- Falk R 1999 Predatory Globalization: A Critique. Polity Press, Cambridge, UK
- Iglehart J 1999 The American health care system: expenditures. New England Journal of Medicine 340: 70–6
- Lee K, Zwi A B 1996 A global political economy approach to AIDS. New Political Economy 1: 355–73
- Pettifor A 1996 Debt, the Most Potent Form of Slavery. Debt Crisis Network, Christian Aid, London
- Sivard R L 1996 World Military and Social Expenditures, 16th edn. WMSE, Leesburg, VA
- Van Rensburg H C J, Benatar S R 2001 History of medicine in Africa. In: Last J, Lock S (eds.) The Oxford Illustrated Companion to Medicine. Oxford University Press, Oxford
- Wilkinson R G 1996 Unhealthy Societies: The Afflictions of Inequality. Routledge, London
- World Health Organization 1995 Poverty and health in developing countries. No. 16 in the WHO series Macroeconomics, Health and Development. World Health Organization, Geneva




