View sample migraine research paper. Browse research paper examples for more inspiration. If you need a health research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
The Clinical Picture
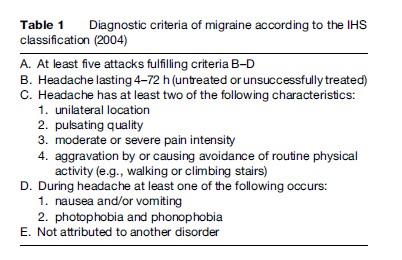
Migraine is an idiopathic headache disorder characterized by moderate to severe, often unilateral and pulsating headache attacks, which are typically aggravated by physical activity. The individual attacks are accompanied by a loss of appetite (almost always), nausea (80%), vomiting (40–50%), light sensitivity (photophobia, 60%), noise sensitivity (phonophobia, 50%) and odor hypersensitivity (10%). If the headaches are unilateral, they can change sides within an attack or from attack to attack. The diagnostic criteria for migraine attacks and the migraine aura are presented in Table 1. The duration of attacks is typically 4 to 72 h; at least five attacks must have occurred before the diagnosis can be established. The frequency and duration of migraine attacks varies widely between individuals, though the median frequency is around one attack per month and median duration is roughly 24 h. In up to 15% of cases, the migraine headache is preceded by a recurrent disorder manifesting itself in attacks of reversible focal neurological symptoms, usually developing gradually over a period of 5 to 20 min and lasting for less than 60 min. This neurological sign known as an aura consists mostly of visual phenomena, typically jagged zig-zag lines that move slowly across the visual field, often followed by visual loss (scotoma). Cortical spreading depression (CSD) has been suggested to underlie migraine visual aura, based on the slow spread of clinical and electrophysiological events in animal experiments.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
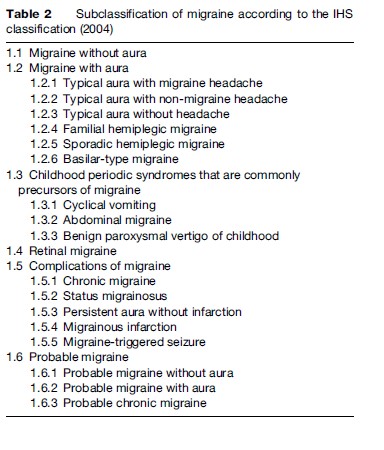
Most patients suffer from migraine attacks without aura. However, there are several migraine syndromes with particular aura features and migraine syndromes with uncommon histories or complications. These syndromes have their own diagnostic criteria; the subclassification of these syndromes is outlined in Table 2. These diagnostic criteria for migraine syndromes are also available on the homepage of the IHS (International Headache Society).
In children, migraine attacks can be shorter (e.g., for only 1 or 2 h) and the accompanying symptoms can be more prominent, including syndromes such as abdominal migraine or periodic syndromes in childhood.
Epidemiology And Genetics of Migraine
Migraine is one of the most frequent headache disorders. from migraine attacks. The lifetime prevalence in females may be up to 25%. Before puberty, the prevalence of migraine is about 5% both in boys and girls. The highest incidence of migraine attacks occurs between the ages 35 and 45, potentially the most productive period of life, with a female preponderance of three to one. The median duration of untreated migraine attacks is 18 h; the median attack frequency is one per month. Epidemiological and twin studies indicate that migraine and in particular migraine with aura is an inherited disease. However, multiple genes must be involved. Familial hemiplegic migraine (FHM) is a dominantly inherited disease in which the affected family members have severe and long-lasting migraine auras sometimes leading to hemiplegia or even loss of consciousness. Several years ago a French group and a Dutch group independently identified a gene locus on chromosome 19 as the responsible culprit. Several genetic loci have been identified by now, encoding P/Q calcium channels, Na2þ/Kþ pump, and a neuronal voltage-gated sodium channel. Consequently, FHM is considered a ‘channelopathy,’ but whether these genetic variants play a role in nonhemiplegic migraine with aura and in migraine without aura is not known.
The Burden Of Migraine
Migraine attacks can have a profound effect on the quality of life of the sufferer. In the long term, migraine may cause emotional changes and result in coping strategies that interfere with work, social, and family life. Consequently, the results of health-related quality-of-life studies demonstrate that migraine has a considerable impact on functional capacity, resulting in disrupted work and social activities. The impact of migraine on many quality of life parameters is similar to that of other chronic conditions, such as osteoarthritis, diabetes, and depression.
The direct costs of migraine (due to medical care) are small compared with the indirect costs caused by absence from work and reduced productivity. Many migraineurs, however, do not seek medical attention, have not been accurately diagnosed by a physician, or do not use prescription medication. Epidemiological studies reveal that migraine is often underdiagnosed and undertreated. Identifying and treating appropriate patients will reduce the impact of migraine on the individual level and the burden of migraine on the society.
Migraine Diagnosis
The diagnosis of migraine is based on the typical patient’s history (see above: clinical picture) and a normal neurological examination. Further investigations, in particular brain imaging, are necessary if secondary headache is suspected (e.g., if the headache characteristics are atypical), when the course of headache attacks changes, or if persistent neurological or psychopathological abnormalities are present. In particular, a diagnostic investigation including imaging of the brain in migraine is recommended when
- the neurological examination is not normal
- typical migraine attacks occur for the first time after the age of 40
- frequency or intensity of migraine attacks continuously increases
- the accompanying symptoms of migraine attacks change
- new psychiatric symptoms occur in relation to the attacks.
Comorbid neuropathologies in migraine may involve mood disorders, such as depression and anxiety, as well as epilepsy and essential tremor. Epidemiological data suggest that migraine may be associated with subclinical vascular brain lesions and that migraine may be a risk factor for cerebral ischemia. However, prospective data evaluating the association between specific headache forms and stroke are sparse. In a recent prospective study including nearly 40 000 women, an increased risk of total and ischemic stroke was found for migraineurs with aura. However, the absolute risk increase was low, with 3.8 additional cases per year per 10 000 women.
Migraine Treatment
The medical treatment of migraine includes both acute therapy aimed at aborting the attacks and prophylactic therapy aimed at reducing attacks in the long term.
Acute Therapy
Several large randomized, placebo-controlled studies have been undertaken to establish the best drug treatment regimen for the acute management of migraine. In most of these trials, successful treatment of migraine attacks was defined as one or a combination of the following criteria:
- pain free after 2 h
- improvement of headache from moderate or severe to mild or none after 2 h
- consistent efficacy in two out of three attacks
- no headache recurrence and no further drug intake within 24 h after successful treatment (so-called sustained pain relief or pain free).
Analgesics And Antiemetics
Analgesics are the preferred drugs of choice for mild or moderate migraine attacks. Evidence of efficacy in migraine treatment in at least one placebo-controlled study has been obtained for acetylsalicylic acid (ASA) up to 1000 mg, for ibuprofen from 200 mg to 800 mg, for diclofenac from 50 mg to 100 mg, 1000 mg for metamizol, and 1000 mg for paracetamol. In addition, the fixed combination of ASA, paracetamol, and caffeine is effective in acute migraine treatment and is also more effective than either of the single substances alone. In order to prevent drug overuse headache, the intake of simple analgesics should be restricted to 15 days per month and the intake of combined analgesics to 10 days per month. Coxibs are not recommended for acute migraine treatment because of cerebrovascular adverse side effects. Opioids are of only minor efficacy; no modern controlled trials are available for these substances. Table 3 presents an overview of analgesics with efficacy in acute migraine treatment.
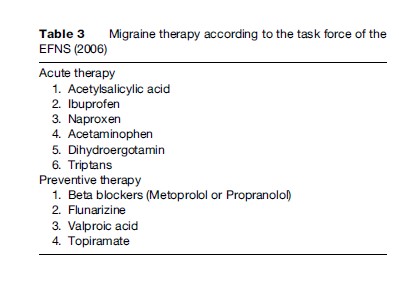
The use of antiemetics in acute migraine attacks is recommended for the treatment of vegetative symptoms and because it is assumed that these drugs improve the resorption of analgesics. However, prospective, placebocontrolled randomized trials to prove this assumption are lacking. There is no evidence that the fixed combination of an antiemetic with an analgesic or with a triptan is more effective than the analgesic or triptan alone. Regarding ergot alkaloids, the only compound with sufficient evidence of efficacy is ergotamine tartrate 2 mg (oral or suppositories). Ergot alkaloids can induce drug overuse headache very fast and at very low doses. Therefore, their use must be limited to 10 days per month. Major side effects include nausea, vomiting, paresthesia, and ergotism. Contraindications are cardiovascular and cerebrovascular diseases, Raynaud’s disease, arterial hypertension, renal failure, and pregnancy and breastfeeding.
Triptans (5-HT1B/1D-Agonists)
The 5-HT1B/1D agonists sumatriptan, zolmitriptan, naratriptan, rizatriptan, almotriptan, eletriptan, and frovatriptan (ordered by year marketed), so-called triptans, are specific migraine medications and should not be used for other headache disorders, except for cluster headache. The efficacy of all triptans has been proven in large placebo-controlled trials of which several meta-analyses have been published. It should be noted that in about 60% of nonresponders to NSAIDs, triptans are effective. Triptans can be effective at any time during a migraine attack.
However, there is evidence that the earlier triptans are taken, the better the efficacy. However, a strategy of strictly early intake may lead to frequent drug treatment in certain patients. The use of triptans is restricted to a maximum of 10 days per month. Otherwise, there is a danger of developing a drug overuse headache.
Preventive Therapy
Prophylactic drug treatment of migraine is possible with several drugs. Substances with good efficacy and tolerability are beta blockers, calcium channel blockers, antiepileptic drugs, NSAIDs, and antidepressants. The use of all these drugs, however, is based on empirical data rather than on proven pathophysiological concepts. The decision to introduce a prophylactic treatment has to be carefully discussed with the patient. A prophylactic drug treatment of migraine should be considered and discussed with the patient when
- the quality of life, business duties, or school attendance are severely impaired
- frequency of attacks per month is two or higher
- migraine attacks do not respond to acute drug treatment
- frequent, very long, or uncomfortable auras occur.
A migraine prophylaxis is regarded as successful if the frequency of migraine attacks per month is decreased by at least 50% within 3 months. For therapy evaluation, a headache diary is mandatory. The drugs of choice, according to the consensus of the task force, are outlined in Table 3.
Specific Situations
Menstrual Migraine
Headaches may occur as a result of natural ovarian cycles, or in response to the withdrawal of exogenously administered estrogen. For some women, these headaches are more severe, are of longer duration, and lead to greater disability than those occurring at other times in the menstrual cycle. Consequently, one prophylactic treatment regimen of menstrual migraine involves estrogen replacement therapy. Supplemental estrogen may be administered in the late luteal phase of the natural menstrual cycle or during the pill-free week of traditional combination oral contraceptives. In menopause, hormonally associated migraine is most likely due to estrogenreplacement regimens. However, evidence regarding the safety and efficacy of hormonal replacement/modulating regimens is limited, and evidence particularly is lacking regarding its long-term dangers or side effects. Consequently, hormonal treatment of migraine is not a preferred treatment strategy for most women with migraine. Alternatively, Naproxen sodium (550 mg twice daily) has been shown to reduce pain including headache in the premenstrual syndrome.
Migraine In Pregnancy
Migraine does not increase the risk of complications of pregnancy either for the mother or for the fetus. Several retrospective studies have shown a tendency for migraine to improve with pregnancy. Between 60 and 70% of women either go into remission or improve significantly, mainly during the second and third trimesters. It seems as if women with migraine onset at menarche and those with perimenstrual migraine are more likely to go into remission during pregnancy. It is in the first trimester that the fetus is at the greatest risk from drugs. Fortunately, most of the pregnant migraineurs experience fewer or even no migraine attacks. However, migraine often recurs post-partum. There are no specific clinical trials evaluating drug treatment of migraine during pregnancy; most of the migraine drugs are contraindicated. If migraine occurs during pregnancy, only paracetamol is recommended. Triptans and ergot alkaloids are contraindicated. The use of prophylactic agents during pregnancy should be the exception, not the rule, and preferably only during the second and third trimesters; only magnesium and metoprolol are recommended.
Migraine In Children And Adolescents
Pediatric headache is a common health problem in children, with a significant headache reported in more than 75% by the age of 15 years. Pediatric migraine occurs in up to 10% of children and in up to 28% of adolescents between the ages of 15 and 19 years. Nevertheless, migraine diagnosis and treatment in these age groups present unique challenges. The attacks are shorter in children than in adolescents, the headache is less specific (may be holocranial, may lack photoor phonophobia, abdominal pain is frequently associated). Children with migraine miss more school days in a school year than their matched controls. Non-drug treatments (relaxation training, self-hypnosis, and biofeedback) have been shown to have good efficacy as prophylactic measures. The only analgesics with evidence of efficacy for acute migraine treatment in children and adolescents are ibuprofen 10 mg per kg body weight and paracetamol 15 mg per kg body weight. The only antiemetic for use in children up to 12 years is domperidon. For migraine prophylaxis, flunarizine and propranolol in low doses showed positive effects in controlled trials. Other drugs have not been studied or did not show efficacy in appropriately designed studies.
The Pathophysiological Puzzle
Migraine has long been considered a vascular headache, based on the idea that changes in vessel diameter or gross changes in cerebral blood flow would trigger pain and could, in part, explain the mechanism of action of vasoconstrictor drugs, such as ergotamine. Modern theories explaining the peripheral pain mechanisms suggest, based on experimental and clinical data, an activation of the trigeminal innervation of the cranial circulation with involvement of vasoactive neuropeptides, such as calcitonin gene-related peptide. To account for the periodicity and other clinical features in migraine, a primary dysfunction of central brain structures seems more likely.
Early studies have emphasized a dysfunction of the cerebrovascular regulation in headache, while little attention has been given to the central processing of headache. Recent data incorporating genetic, electrophysiological, and neuroimaging techniques have revolutionized our understanding of the pathophysiology of migraine and provided unique insights into this syndrome. Modern imaging studies point, together with the clinical picture, toward a central triggering cause, possibly based on genetic variations. The early functional imaging work has recently been reworked and implies involvement of highly specific activation of the brainstem in migraine, though it is still unclear whether in a permissive or triggering manner. Additionally, most studies show that information processing is abnormal in migraineurs. The best documented abnormality is an interictal lack of habituation in migraineurs, with normalization during the headache state. Together with a diminished energy reserve found in MRspectroscopy studies, a possible role of increased energy consumption in attack generation has been suggested. Following this line of thought, migraine is understood as a paroxysmal central nervous system dysfunction.
Regarding the development of head pain, both vascular and neuronal mechanisms have been proposed. A much discussed scenario begins with CSD, which in turn activates the trigeminovascular system and causes headaches. As most of the migraine patients never experience an aura, silent CSD attacks have been proposed to explain why these patients suffer from recurrent attacks. In summary, modern concepts suggest that migraine is, in essence, a neurovascular headache, and that the susceptibility to CSD and to migraine is probably genetically determined.
Bibliography:
- Bolay H, Reuter U, Dunn AK, et al. (2002) Intrinsic brain activity triggers trigeminal meningeal afferents in a migraine model. Nature Medicine 8(2): 136–142.
- Diener HC, Steiner TJ, and Tepper SJ (2006) Migraine—the forgotten epidemic: Development of the EHF/WHA Rome Declaration on Migraine. Journal of Headache and Pain 7(6): 433–437.
- Evers S, Afra J, Frese A, et al. (2006) EFNS guideline on the drug treatment of migraine–report of an EFNS task force. European Journal of Neurology 13(6): 560–572.
- Ferrari MD, Roon KI, Lipton RB, et al. (2001) Oral triptans (serotonin 5–HT(1B/1D) agonists) in acute migraine treatment: A meta-analysis of 53 trials. Lancet 358(9294): 1668–1675.
- Goadsby PJ (2005) Advances in the understanding of headache. British Medical Bulletin 73–74(1): 83–92.
- Goadsby PJ (2005) Migraine pathophysiology. Headache 45 (supplement 1): S14–S24.
- Goadsby PJ (2006) Recent advances in the diagnosis and management of migraine. British Medical Journal 332(7532): 25–29.
- Headache Classification Committee of the International Headache Society (2004) The International Classification of Headache Disorders, 2nd edn. Cephalalgia 24(supplement 1): 1–160.
- Kelman L (2004) The aura: A tertiary care study of 952 migraine patients. Cephalalgia 24(9): 728–734.
- Kurth T, Slomke MA, Kase CS, et al. (2005) Migraine, headache, and the risk of stroke in women: A prospective study. Neurology 64(6): 1020–1026.
- Lance JW and Goadsby PJ (2005) Mechanism and Management of Headache. Oxford, UK: Butterworth-Heinemann Ltd.
- Lipton RB, Stewart WF, and Von Korff M (1994) The burden of migraine: A review of cost to society. Pharmacoeconomics 6(3): 215–221.
- Lipton RB, Stewart WF, Diamond S, et al. (2001) Prevalence and burden of migraine in the United States: Data from the American Migraine Study II. Headache 41(7): 646–657.
- Lipton RB and Bigal ME (2006) Migraine and cardiovascular disease. Journal of the American Medical Association 296(3): 332–333.
- Olesen J, Tfelt–Hansen P, and Welch K (2006) The Headaches. Philadelphia, PA: Lippincott Williams & Wilkins.




