View sample vitamin D research paper. Browse research paper examples for more inspiration. If you need a health research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Introduction
A vitamin is an organic substance needed in micro amounts per day, and whose lack results in deficiency disease. Gross deficiency of vitamin D results in rickets or osteomalacia. However, recent research implicates vitamin D insufficiency in the risk for, and the prospective outcomes of, many diseases.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
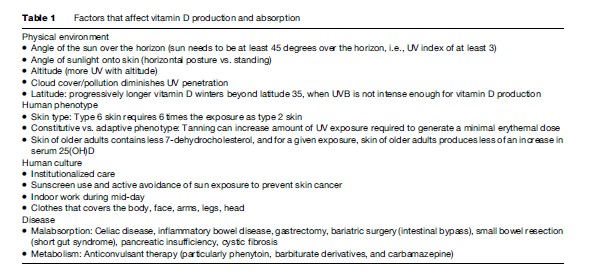
Vitamin D is produced in skin exposed to sunshine when the UV index is at least 3. The supply of vitamin D to humans is affected by the factors listed in Table 1, each of which can increase the need for oral intake of vitamin D. Vitamin D is unique among vitamins, because traditional food intake cannot deliver amounts now deemed optimal for health. A further distinction is that vitamin D is the precursor of a hormone, 1,25dihydroxyvitamin D, whose concentration in plasma is regulated, and which signals nuclear processes that affect an array of biological responses. Vitamin D from skin or the gut is metabolized readily in the liver to 25-hydroxyvitamin D (25(OH)D), which is the objective measure of vitamin D nutrition. The 25(OH)D concentration diagnostic of nutrient deficiency rickets is a serum or plasma 25(OH)D concentration below 10 ng/ml (25 nmol/l). A deficiency in 25(OH)D impairs deposition of calcium into the protein matrix of bone. In children this results in rickets, with its classic bowed legs. In adults, 25(OH)D deficiency causes osteomalacia, a curable disease of low bone density, which is a cause of osteoporosis if left untreated.
Despite abundant sunshine, many people in the developing world exhibit clinically deficient 25(OH)D concentrations, which adversely affects neuromuscular function and balance. Many women reportedly suffer back pain that is curable with vitamin D supplementation. Epidemiologic studies associate higher 25(OH)D with lower risk of cancers of colon, breast, and prostate, better neuromuscular function and improved overall well-being. Elderly adults with higher 25(OH)D concentrations are less likely to require institutional care in subsequent years. The challenge for public health is whether or how to respond to the evidence for health effects of vitamin D.
Chemistry
There are two molecules accepted as nutritional vitamin D, namely, vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Vitamin D3 is the form physiologically present in all animals. When light of UVB wavelength, 280–315 nanometers, reaches the epidermal layer of skin, this breaks open a molecule on the pathway to becoming a cholesterol molecule. This disruption of the B-ring of 7-dehydrocholesterol produces what is called secosteroid which spontaneously isomerizes to become vitamin D3. A different molecule, vitamin D2, can be synthesized from ergosterol, a plant steroid. Vitamin D2 has been used as a supplement since the 1930s, but is about half as potent as vitamin D3.
Vitamin D and its more active metabolites share most of the multiring structure of classical steroid hormones like cortisol, estradiol, progesterone, aldosterone, and testosterone. Vitamin D and its metabolites have poor solubility in water, they require binding to vitamin D-binding protein for transport in the circulation, and they need to be metabolized into an active form. Metabolites of vitamin D should not be thought of as the nutrient vitamin D. The liver readily converts vitamin D into 25(OH)D, which resides in the body for many weeks. The active metabolite, 1,25-dihydroxyvitamin D, enters cells, and binds to the vitamin D receptor (VDR), a specific, cytosolic nuclear protein that then binds to DNA to affect transcription.
The Hormone And Signaling Molecule Made From Vitamin D
A hormone is a signaling molecule produced and secreted by specific glands and cells within the body. After secretion into the bloodstream, a hormone regulates the behavior of one or more distant target organs that respond to it. Like cholesterol, vitamin D per se is not a hormone, but rather an inactive precursor. The terminology of signaling molecules is illustrated in Figure 1, and Figure 2 relates this to the vitamin D system.
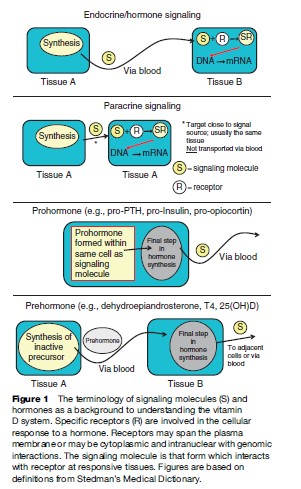
Vitamin D that enters the body is stored in approximately equal proportions in adipose and muscle tissues. The residence time of vitamin D in the body, expressed as a half-life, is about 2 months. Virtually all the vitamin D related molecules in the blood are in the form of 25(OH)D, produced by 25-hydroxylase enzymes that are mostly in the liver. Cells in the kidney take up 25(OH)D bound to vitamin D binding protein (DBP). DBP has a half-life of about 3 days and if the 25(OH)D it carries is not needed for metabolism by the kidney, it is recycled back into plasma. The kidney synthesizes and secretes 1,25(OH)2D in response to the need for calcium. Thus, one function of the kidney is to serve as a classic endocrine gland producing the hormone, 1,25(OH)2D, which stimulates active absorption of calcium across the intestine, and which promotes the incorporation of the calcium into bone.
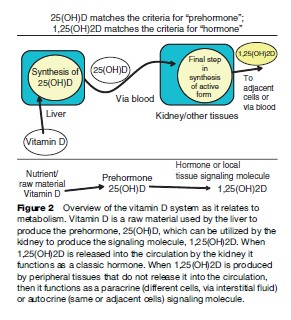
Vitamin D nutrition is measured with a serum 25(OH)D assay. This metabolite is required for a growing number of nonclassical effects that are not related to bone and mineral metabolism. Nonclassical effects are thought to be the result of enzyme present in various tissues that produce 1,25(OH)2D. Those tissues do not normally release their 1,25(OH)2D into the circulation. The activation in various tissues of 25(OH)D into the signaling molecule, 1,25(OH)2D, accounts for the broad-range, health-related effects being attributed to vitamin D nutrition. These effects range from influencing neuromuscular functions that include well-being and muscle function, responsiveness to other hormones, and cell behavior. The nontraditional effects of vitamin D are mediated through local, paracrine, and autocrine signaling within tissues.
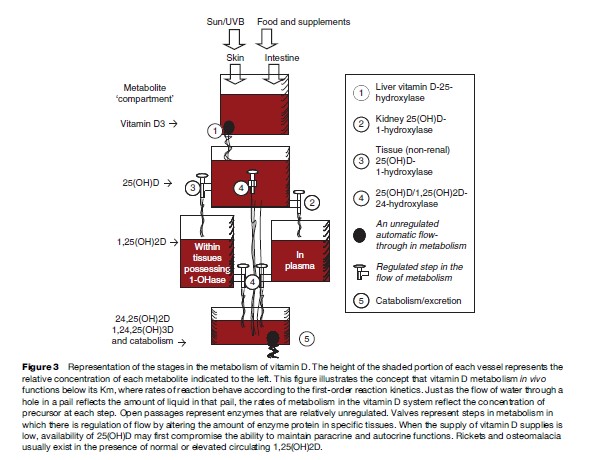
The feature that makes the principles of the vitamin D system especially difficult to understand is that in contrast to other hormones, the material needed to produce 1,25(OH)2D is scarce. Limited availability of substrate poses challenges to the systems that regulate production of 1,25(OH)2D. To illustrate this, Figure 3 depicts 25(OH)D metabolism as a series of flow-through buckets, because like water in a pail, the flow through an opening is determined very much by the amount of material present. More substrate – that is, a higher 25(OH)D concentration in the circulating plasma – increases the capacity of various cells to produce 1,25(OH)2D. This relationship between substrate and hormone is called a first-order reaction. It is in stark contrast to the situation typical for other steroid hormones. The concentration of serum 25(OH)D is expressed as nanomoles per liter (10 -9 M), whereas the concentration of cholesterol is millimolar (10 3 M; 1 millimol = 1 million nanomoles). It does not matter what the cholesterol level is, there is always more than enough to make steroid hormones – this relationship with substrate is called a zero-order reaction. Hormone production is almost always a zeroorder reaction – except for 1,25(OH)2D. Although vitamin D and 25(OH)D are not molecules that send signals to cells, they sometimes appear to behave as if they were, because they can increase the cellular concentration of the signaling molecule, 1,25(OH)2D.
Rickets And Osteomalacia, The Traditional Vitamin D Deficiency Diseases
When there is a dietary absence of vitamin D or if there is too little exposure of skin to ultraviolet light, then bone mineralization is impaired. In children, the resulting disease is called rickets and in adults, it is known as osteomalacia. The classical skeletal characteristic of rickets involves anatomic deformity of the bones, especially in the pelvis, ribs, knees, wrists, and ankles. Moreover, a myopathy (muscle disease) accompanies the lack of vitamin D. Even before anatomic changes are evident, an affected infant may be described as a weak, floppy, crying baby. Rachitic infants are especially susceptible to pneumonia, because of the inefficient respiratory function caused by the myopathy and because vitamin D adequacy is necessary for optimal function of the immune system.
Regular access to vitamin D throughout life is necessary so that the body can adapt to variation in dietary calcium. A positive balance of calcium is essential for normal growth and skeletal development. In mature adults, a negative balance of calcium causes declines in bone density. This is, first, because of inadequate mineralization of the protein matrix laid down in the normal process of bone turnover. Poor mineralization of bone matrix in adults is called osteomalacia, and it is not normally accompanied by anatomic changes. The most widely known bone disease, osteoporosis, occurs when bone tissue is normally mineralized but the mass, density, and strength of bone are decreased, resulting in an increased risk of fracture. Osteomalacia is not distinguishable from osteoporosis by dual photon bone densitometry (the usual measure of bone density). Rather, either a diagnosis of osteomalacia is achieved with a pathology examination of a bone biopsy sample taken from the individual, or osteomalacia is assumed to be present if the serum 25(OH)D is low. Patients with osteomalacia show a strong clinical response when vitamin D supplement is given, with a rapid (within 1 year) gain in bone density. Osteomalacia is thought to be a preliminary, predisposing factor in a natural progression toward osteoporosis.
The accepted biochemical criterion that poor vitamin D nutrition is causing rickets or osteomalacia is a serum 25(OH)D concentration that is <10 ng/ml (<25 nmol/l). If calcium intake is particularly low, then vitamin D deficiency rickets or osteomalacia may occur with 25(OH)D concentrations higher than this, likely <40 nmol/l (<16 ng/ml).
Osteoporosis, A Vitamin D Deficiency Disease
The weight of clinical trial evidence shows that if healthy older adults are compliant and indeed take their vitamin D and calcium, then their risk of fractures declines by about one third (Bischoff-Ferrari et al., 2006). Balance, muscle function, rate of falls, calcium absorption, and bone mineralization are all affected by vitamin D status. However, UVB-related synthesis of vitamin D in the skin significantly declines with age. Synthesis rates in the elderly ( 70 years of age) are about one third those of young adults. Not only are the elderly at a biological disadvantage with respect to their ability to make vitamin D in the skin, they are exposed to less total sunlight if they reside in nursing homes or hospitals or if they have reduced mobility. Therefore, the elderly population is particularly susceptible to vitamin D deficiency, and this exacerbates osteoporosis and its complications.
Health Effects Of Higher Vitamin D Nutrition
In addition to clinical trials focusing on osteoporosis, a host of epidemiologic studies have been conducted in diverse populations. Disease relationships such as tuberculosis, multiple sclerosis and diabetes, cancers of the colon, prostate, breast, and lung all suggest that higher 25(OH)D concentrations are desirable. Beyond the statistical event of a disease per se, higher 25(OH)D concentrations are associated with less depression, improved well-being, and lower risk of nursing home admission. In 2007, a randomized trial of American women was the first clinical trial of vitamin D that used 1100 IU/day (>28 mg/day) of vitamin D3 in addition to the usual vitamin D intake. The study showed a substantial reduction in the rate at which new cancers were diagnosed over the subsequent 4 years (Lappe et al., 2007). Those findings have been criticized because the study was designed to look at osteoporosis, and cancer was an incidental, secondary finding. If the opposite had been found, that is, if the vitamin D and calcium had produced a substantial increase in cancer rates, would there have been such questioning of the findings? This illustrates the tendency to accept bad news at face value, and to question the beneficial effects evident with vitamin D.
Requirements For Vitamin D
Human biology evolved to be optimized for sun-rich tropical environments without clothing. Under the conditions present during human evolution, the supply of the 25(OH)D substrate would have been optimal for the endocrine, paracrine, and autocrine systems that depend on 25(OH)D supplies – with blood 25(OH)D concentrations in the order of 150 nmol/l (60 ng/ml). In comparison, modern populations exhibit serum 25(OH)D concentrations that are a fraction of that. Skin color is the most obvious phenotypic adaptation of human populations that have migrated to temperate latitudes. If skin color was optimized to ancestral latitude, then the relatively recent, large-scale migration of humans with dark skin away from the equator is probably contributing to an unnecessary burden of disease for those with dark skin living in temperate latitudes. Reduced ability to produce vitamin D because of dark skin (in temperate climates) imposes a substantially higher requirement for vitamin D supplementation, but as of 2007, this problem has not been taken into account by government-mandated nutrition guidelines.
The current ‘adequate intake’ for vitamin D, as recommended in 1997 by the Food and Nutrition Board of the U.S. Institute of Medicine from birth to age 51 years is 200 IU/day (5 mg/day). For infants, the recommendation is based, historically, on the amount of vitamin D in a teaspoon of cod-liver oil; many years of experience have proven this to be appropriate for preventing rickets. Since adults have at least ten times the body mass of infants, the 200 IU/day adult recommendation (Food and Nutrition Board, 1997) is obviously a gross underestimation of the amount of vitamin D that may be useful to adults.
When it comes to formal advice for any nutrient, not just vitamin D, the goal of the recommended intake is to ensure that practically all people who follow the recommendation will reach or exceed some objective measure of nutrient adequacy. For vitamin D the objective measure of adequacy is especially straightforward. The concentration of 25(OH)D in serum or plasma is a long-term, stable measure of adequacy. Based on clinical trials, the desire is now to ensure that serum 25(OH)D concentration is at least 30 ng/ml (75 nmol/l). Many studies show that on average, the long-term intake of every additional 100 IU/day (2.5 mg/day) of vitamin D3 will raise the average 25(OH)D concentration by a further 1 ng/ml (2.5 nmol/l). These numbers offer a straightforward way to estimate the requirement for vitamin D. For example, an adult whose serum 25(OH)D concentration is 10 ng/ml (25 nmol/l) should want to raise this by 20 ng/ml (50 nmol/l) to 30 ng/ml. The dose required to achieve this would be 20 times 100 IU/day, which equals 2000 IU/day. This is an estimate for the average adult, so that about half of adults whose serum level starts from 10 ng/ml (25 nmol/l) will need more than this dose to reach the goal. It takes at least 3 months before the 25(OH)D response to a steady, new daily vitamin D intake starts to approach its final concentration.
Why Vitamin D Is Controversial In Public Health
Many strands of evidence point to higher serum 25(OH)D as a positive contributor to health. For instance, randomized, placebo-controlled clinical trials (RCTs) investigating the effects of daily supplementation with 800 IU (20 mg) vitamin D have shown that this dose prevents over 20% of hip or nonvertebral fractures compared with placebo, in older adults (>65 years) who are taking vitamin D regularly. Furthermore, the minimum serum 25(OH)D concentration associated with fewer fractures was 75 nmol/l. A few clinical trials in which adults were given calcium with 800 IU (20 mg) vitamin D failed to produce fewer fractures because compliance was so poor that average blood levels of participants did not reach 75 nmol/l. Thus, 25(OH)D levels in older adults should exceed this amount, but the problem is, how do you get people to follow advice to take vitamin D?
The totality of evidence favoring a higher serum 25(OH)D is increasingly compelling. However, the issue of how to implement public health measures to raise 25(OH)D across the population is extremely controversial, and complicated by a remarkable resistance of government-mandated advice to adapt to the evidence at hand. Advice to spend time in the sun is complicated by the factors listed in Table 1 and by risk of skin cancer for some. Food fortification with vitamin D is difficult because people vary in their dietary preferences, possibly over-consuming or not at all consuming the fortified food. The debate about fortification would be simplified if higher doses of vitamin D were regarded as safe, but there is still a widespread fear of vitamin D. Supplementation with vitamin D in multivitamins is controversial, because of the expense, because most people do not take them regularly, and because there is sparse evidence that widespread supplementation with a mix of vitamins improves health. Supplementation with a single nutrient, vitamin D, would be simple and inexpensive, but this is complicated by the need of public health professionals to adhere to the advice mandated by governments. For vitamin D, the current advice mandated by governments for intake is too low to have a meaningful effect on adults.
Bibliography:
- Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, and Dawson-Hughes B (2006) Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. American Journal of Clinical Nutrition 84: 18–28.
- Lappe JM, Travers-Gustafson D, Davies KM, Recker RR, and Heaney RP (2007) Vitamin D and calcium supplementation reduces cancer risk: Results of a randomized trial. American Journal of Clinical Nutrition 85: 1586–1591.
- Heaney RP (2006) Barriers to optimizing vitamin d3 intake for the elderly. Journal of Nutrition 136: 1123–1125.
- Vieth R (2005) The pharmacology of vitamin D, including fortification strategies. In: Feldman D, Glorieux F, and Pike JW (eds.) Vitamin D, 2nd edn., pp. 995–1015. New York: Elsevier.
- Vieth R, Bischoff-Ferrari H, Boucher BJ, et al. (2007) The urgent need to recommend an intake of vitamin D that is effective. American Journal of Clinical Nutrition 85: 649–650.
- https://ods.od.nih.gov/factsheets/Vitamind-HealthProfessional/ – National Institutes of Health (NIH), Office of Dietary Supplements (ODS). The ODS provides the official perspective about vitamin D nutrition in the United States.




