Sample Coronary Heart Disease Research Paper. Browse other research paper examples and check the list of research paper topics for more inspiration. iResearchNet offers academic assignment help for students all over the world: writing from scratch, editing, proofreading, problem solving, from essays to dissertations, from humanities to STEM. We offer full confidentiality, safe payment, originality, and money-back guarantee. Secure your academic success with our risk-free services.
1. Introduction
A comprehensive review of the epidemiology and prevention of cardiovascular disease is given in Labar-the (1998). In industrialised countries, the commonest cause of death is coronary heart disease (CHD). This research paper will thus focus on CHD and its associated risk factors. Consideration of all of these risk factors is relevant, as virtually all are strongly influenced by psychosocial processes. Large differences in disease rates between countries, evidence that risk of disease changes on migration, large differences within countries according to socioeconomic position and area of residence, and relatively rapid changes over time, suggest that the disease is preventable.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
CHD has been defined as ‘myocardial impairment due to an imbalance between coronary blood flow and myocardial requirements caused by changes in the coronary circulation.’ Atherosclerosis is an important underlying pathological process. The process of atheroma deposition in coronary arteries, however, cannot be observed directly in life without the use of invasive clinical procedures. Even so, the study of symptomatic disease may actually be more appropriate. The clinical disease is, after all, what is experienced and may represent the culmination of a number of pathological processes.
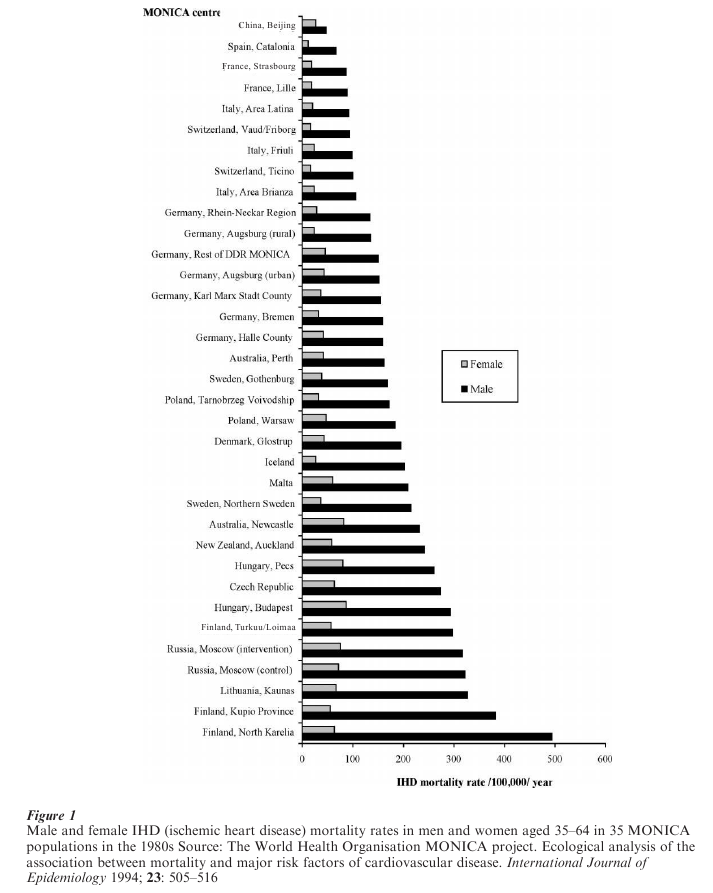
Large differences in disease rates between countries, evidence that risk of disease changes on migration, large differences within countries according to socio-economic position and area of residence and relatively rapid changes over time, suggest that the disease is preventable. To illustrate this international variation the rates of death attributed to CHD in men and women from the populations participating in the World Health Organisation MONICA (monitoring trends and determinants in cardiovascular disease) study are shown in Fig. 1.
CHD was until recently viewed largely as a twentieth century epidemic. In retrospect it seems clear that CHD occurred before this. William Heberden de-scribed the typical symptoms of angina pectoris in 1768. Later in the eighteenth century Dr Samuel Black of Newry, County Down, described many cases of angina pectoris and produced a list of factors associated with increased and decreased susceptibility to angina, which are similar to those currently considered plausible (Evans 1995). While angina pectoris occasionally was recorded as a cause of death, less than 2 percent of all deaths attributed to heart disease in Britain fell into this category even by the early part of the twentieth century.
Atherosclerosis has been demonstrated in Egyptian mummies, but the first contemporary descriptions occurred in the sixteenth century. As CHD is associated with advanced coronary atherosclerosis, the in-crease in CHD mortality in the first half of the twentieth century would be expected to be accompanied by increases in severe atheroma. However, studies of postmortem records of the London Hospital suggested that there was no such increase. Later data comparing the coronary arteries at postmortem of US soldiers who died in the Korean and Vietnam War reported more atheroma in the early 1950s than the 1960s, while CHD mortality in the USA was high and stable over this period. The relative contribution of atherosclerosis and other pathological processes, such as thrombotic tendency, to trends over time and differences between countries in CHD mortality is unclear.
2. International Trends In CHD
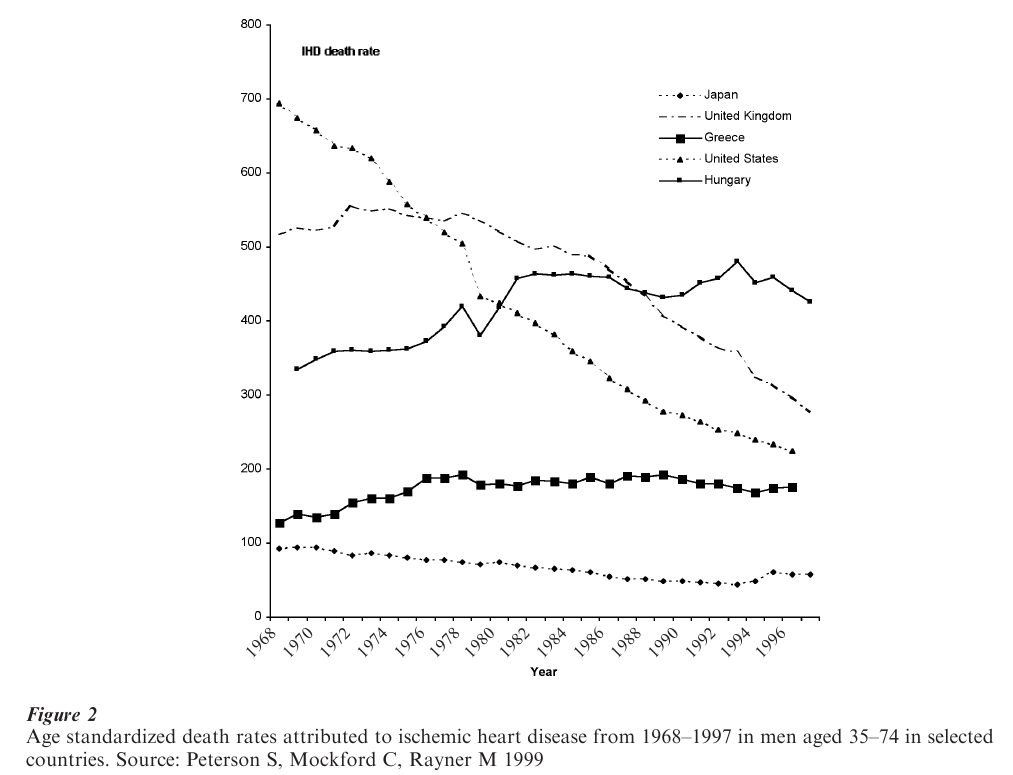
Nonsocialist developed countries have generally shown a similar pattern of rise and then fall in CHD mortality. Some, like the United States, experienced an early and rapid fall, whereas others, such as the UK, experienced a relatively late onset decline. Rates in Japan and the Mediterranean countries of Europe are low. These international time trends for men are illustrated in Fig. 2. The MONICA (Monitoring Trends and Determinants in Cardiovascular Disease) study has shown that the recent trends in mortality are attributable to both changes in event rates and changes in case fatality. Changes in case fatality suggest that medical interventions are reducing mortality in groups with existing CHD.
3. Migrant Studies
Migrant studies provide valuable insights into the heritability of disease and the stage of life at which risk is determined. Studies of Japanese migrants to Hawaii and mainland America suggest that as they adopt Western lifestyles their CHD risk increases. More puzzling is the fact that migrants to Australia from Greek islands, despite adopting many of the detrimental habits of their host country, are at lower risk of CHD. It may be that Greek Australians adopt healthier lifestyles in other respects that counterbalance their increased fat consumption and smoking prevalence (Powles 1994).
4. Overview Of Risk Factors For CHD
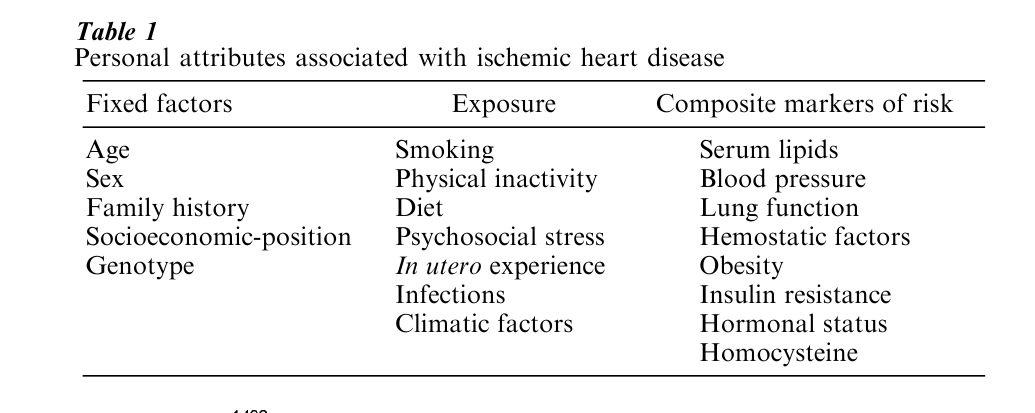
There are a number of personal attributes, often described as risk factors, associated with the development of CHD. Some of these—like age—are fixed. Others, like smoking, are modifiable. And some, like serum cholesterol, though modifiable, are a product of the interplay between an individual’s genetic make-up and environmental exposures. A list of some of the attributes associated with CHD is set out in Table 1. This list is not dissimilar to the list proposed by Samuel Black 200 years earlier, although Black considered that more affluent people were at greater risk of CHD.
Stamler suggests that the major modifiable risk factors are smoking, high blood pressure, high serum cholesterol, and diet. These major risk factors are powerful predictors of CHD. In a large study of middle-aged US men, smokers in the highest quintiles for serum total cholesterol and systolic blood pressure were around 20 times more likely to die from CHD over the next 12 years as nonsmokers in the lowest quintiles of serum cholesterol and blood pressure (Neaton and Wentworth 1992). Though they are powerful individual predictors of risk these factors only accounted for 23 percent of the variance in CHD incidence in men and 14 percent of the variance in women observed between populations in the WHO MONICA study.
4.1 Age
Age is a strong risk indicator for CHD incidence and mortality. Compared to men aged 40, 50-year old men have five times the risk, 60-year old men have 15 times the risk, and 70-year old men have over 40 times the risk of dying from CHD (Labarthe 1998). A similar steep gradient with age is seen for women. Risk continues to increase into older age groups. Recent evidence suggests that the elderly benefit from risk factor control. This combined with their higher absolute level of risk means that sizeable absolute reductions in CHD risk can be achieved in older people and where therapies may be particularly cost effective.
4.2 Gender
Rates of death attributed to CHD in men are consistently three to four times higher than those in women. There are, however, marked variations in the rates of death between countries, such that women in Northern Ireland/or Scotland have CHD death rates that are four times higher than those experienced by Japanese men. The rates of death attributed to CHD in women correlate closely with those in men, suggesting that common environmental factors explain these international differences.
Despite the fact that women have been under represented in epidemiological studies of CHD, it nevertheless appears that risk factors such as serum total cholesterol, blood pressure, and smoking per-form similarly in women. But as the disease is commoner in men, the differences in absolute risk are much greater for men.
Men are more likely to smoke than women are, but differences in smoking and other coronary risk factors do not fully explain the observed excess of CHD seen in men. The lower risk of coronary heart disease among women has understandably led to studies of sex hormones. There is at present, however, little evidence to support a decisive role for sex hormones. Many observational studies (of women who had elected to take hormone replacement therapy (HRT)) appeared to support this contention, but the findings of randomized controlled trials (where women were allocated at random to HRT or placebo), while still preliminary, suggest no such protection is given by HRT (Barrett-Connor 2001).
4.3 Family History And Genetic Factors
A family history of CHD in first-degree relatives is associated with an increased risk of CHD (Labarthe 1998). Currently identified major single-gene conditions, for example, familial hypercholesterolemia, are uncommon, so while they are associated with a large increase in risk for an individual, they contribute little to population CHD rates. Other polymorphisms with lower relative risks but greater prevalence are under investigation. Individuals with a family history of premature CHD are at higher risk and thus may have more to gain from risk factor control.
4.4 Early-Life Influences
The majority of epidemiological research on CHD has focussed on risk factors acting in adulthood. More recently, it has been appreciated that environmental factors acting in utero or in childhood may be important. A series of studies has demonstrated that birth weight is inversely related to risk of CHD, suggesting that suboptimal intrauterine environments result in offspring who, many years later, are more likely to succumb to CHD (Barker 1998). Further-more, several CHD risk factors have been shown to be related to birth weight. However, taking these risk factors into consideration does not appear to fully account for the influence of fetal development on CHD risk, which seems to involve other, as yet unspecified, pathways. It is also possible that genetic factors could underlie both low birth weight and increased disease risk in adulthood. Whether modifying fetal development will modify later CHD risk is a matter which requires further investigation.
Exposures acting in infancy, childhood, and adolescence may also be of importance. A frequently replicated and long-standing observation is that taller individuals are at reduced CHD risk. Recently, it has been shown that stature in childhood is inversely related to later CHD risk, indicating that the association between height and CHD mortality is not due to differential shrinkage occurring in adulthood amongst individuals most prone to CHD (Gunnell et al. 1998). Growth occurs during infancy and child-hood, being influenced by nutrition and infections, as well as genetic factors. Childhood growth may also be influenced by stress. Of the infections acquired in childhood, Helicobacter pylori infection has been most widely investigated, but the overall evidence does not strongly point in the direction of a direct causal association between this infection and CHD risk.
4.5 Diet
Various dietary characteristics have been associated with risk of CHD. These include alcohol, dietary fat, and dietary antioxidants such as ß-carotene.
Moderate consumption of alcoholic drinks appears to protect against CHD, with higher rates of CHD in teetotallers and heavy drinkers. Ecological comparisons suggest that wine may exert additional protection but cohort studies appear to show that the type of beverage is unimportant. People who indulge in sporadic—or binge—drinking appear to be at in-creased (rather than reduced) risk of CHD.
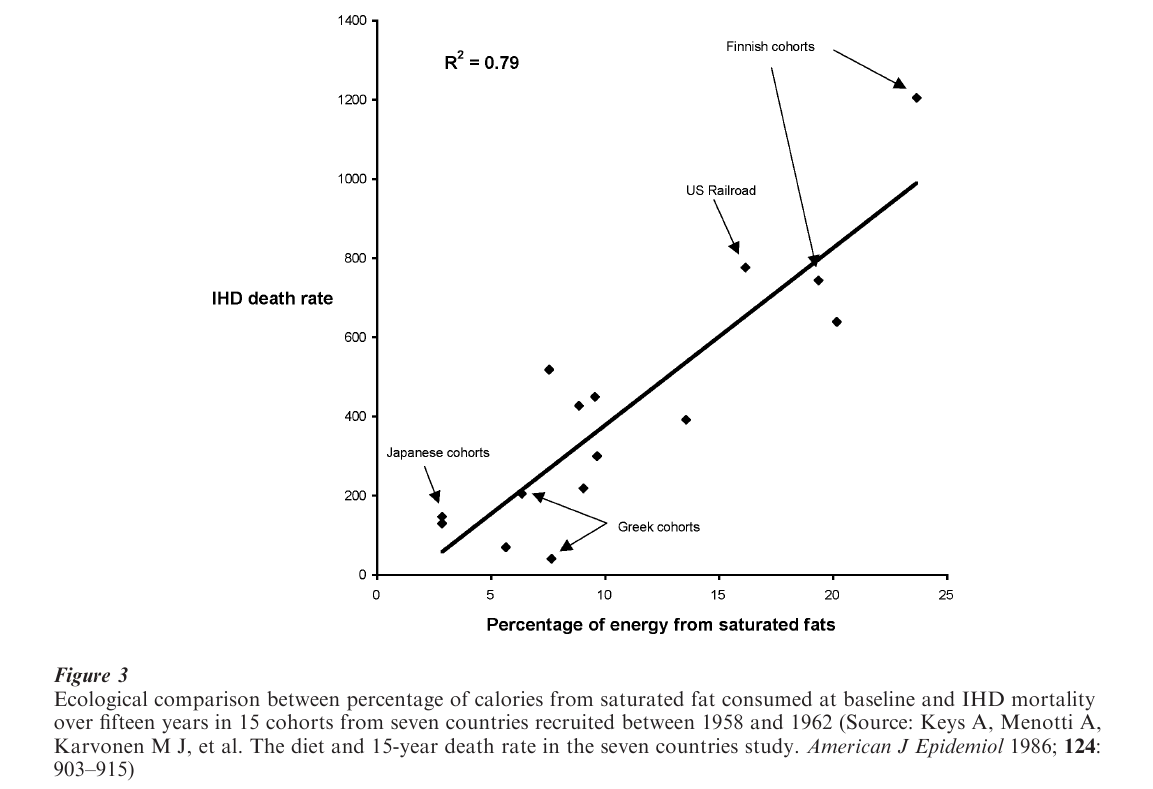
The Seven Countries Study compared the diets of individuals from populations with different rates of CHD. It showed a strong ecological association between CHD mortality and saturated fat consumption. The results of this study are shown in Fig. 3. The relationship between fats and CHD may be complex with different fatty acids increasing, decreasing or having no effect on CHD risk.
Prospective studies of β-carotene intake showed a significantly lower risk of cardiovascular death among those consuming more β-carotene. The results from the trials, however, indicated a moderate adverse effect of β-carotene supplementation. The results are summarized in Fig. 4
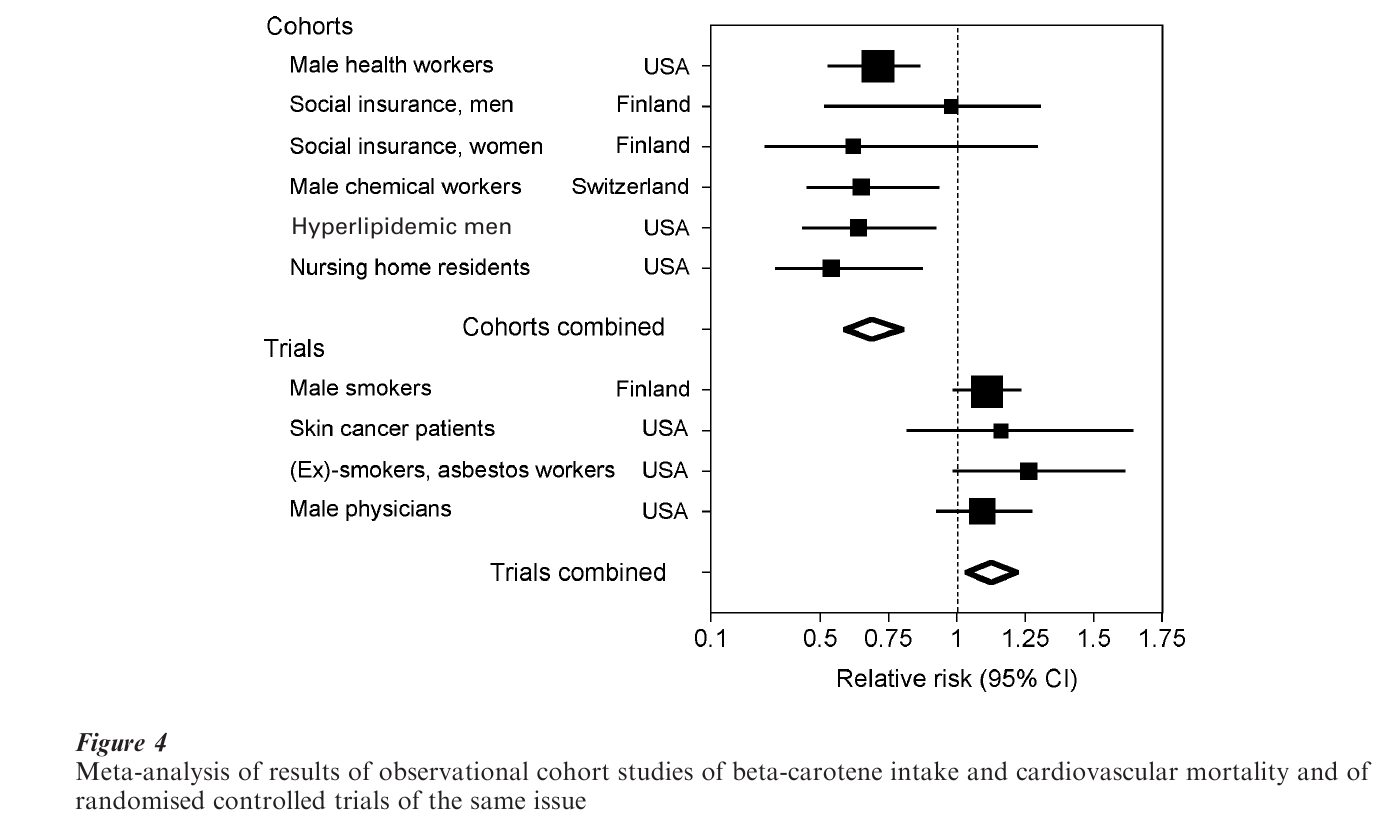
It is likely that the apparent protective association in observational studies represents confounding evidence, as people who eat diets rich in β-carotene or who take supplements are more socioeconomically advantaged and adopt a number of protective health-related behaviors. This finding is of importance both in itself, and as a demonstration of the kinds of spurious findings which can be observed in observational epidemiological studies. The same cautious approach to the interpretation of evidence is certainly required with respect to studies of psychosocial factors.
4.6 Smoking
Smoking was identified as a cause of lung cancer by German researchers in the 1930s and 1940s. Since the results of prospective epidemiological studies in the 1950s it has been clear that heavy cigarette smokers have approximately twice the risk of CHD (Labarthe 1998). This risk is reduced by giving up cigarettes, and returns to that of non-smokers after about 10 years.
4.7 Obesity
Very obese individuals have an increased risk of CHD. A U-shaped association between adiposity and CHD mortality has been seen in many studies. It seems likely that the high mortality among thin people occurs because some thin people are ill and some thin people smoke or drink heavily. Obesity is at least partially related to higher CHD risk because it is associated with higher blood pressure and an unfavorable blood lipid profile (Labarthe 1998). Hereditability models suggest that obesity is, to a remarkable degree, a genetic characteristic of individuals, with only a small proportion of the variance being accounted for by environmental factors. However, the substantial changes in the prevalence of obesity which have occurred within populations such as the UK over a relatively short period of time indicate that environ-mental factors (notably low levels of physical activity) are of great importance.
4.8 Physical Inactivity
Initially, it was thought that exercise predisposed to coronary heart disease, through cardiac strain. However, research starting in the mid-twentieth century suggested that occupational physical activity was associated with reduced risk of CHD. Clearly, health-related selection is a serious problem in studying the relationship between physical activity and coronary heart disease, since those with early signs of the disease will be less active. Engagement in leisure time physical activity is also associated with other important risk factors for CHD, such as socioeconomic position. However, the evidence suggests that increased physical activity does protect against CHD, although there is uncertainty about the type, intensity, and frequency of exercise required. A formulation consistent with the current data is that physical activity, which is at a sufficient level to produce cardio-respiratory training, reduces the risk of coronary heart disease, while the value of lower intensity physical activity is unclear. The level of activity which is protective will therefore depend upon the fitness level of an individual. For the unfit individual, even very mild exercise would produce a cardio-respiratory training effect. As the individual gets fitter, a higher degree of exercise will be required.
4.9 Cholesterol
Circulating blood cholesterol is strongly and positively associated with CHD risk. A series of large therapeutic trials of cholesterol reduction demonstrated that this process is reversible and risk reductions of the magnitude predicted from the observational data can be produced. A 20 percent reduction in cholesterol is associated with around 25 percent reduction in coronary heart disease mortality risk (Ebrahim et al. 1998). Early epidemiological studies only measured total circulating cholesterol, but it is evident that subfractions of cholesterol have differential effects on CHD risk. The adverse effects are restricted to the low-density lipoprotein cholesterol fraction, with high-density lipoprotein cholesterol (HDL) levels being inversely associated with coronary heart disease risk.
4.10 Blood Pressure
There is a strong dose–response relationship between increased blood pressure and increased risk of CHD. Large randomized trials of pharmacological blood pressure reduction in middle age have confirmed that blood pressure reduction reduces subsequent risk of CHD (Collins and MacMahon 1994). Several observational studies have also shown that increased blood pressure in early adult life is associated with increased CHD mortality in later life, suggesting that risk trajectory may be set early (McCarron et al. 2000).
4.11 Hemostatic Factors
In the middle of the nineteenth century, Karl Freiherr von Rokitansky of Vienna proposed that CHD had a thrombogenic basis. Since the 1980s, a number of cohort studies have examined the association between hemostatic factors and coronary disease (Labarthe 1998). There is a consistent independent association
between increased fibrinogen levels and increased risk of coronary disease. Some prospective studies have reported increased coronary risk with factors VII and VIII but the data are less extensive and less consistent. Smokers have higher fibrinogen levels than non- smokers and this may in part explain the excess coronary risk observed in smokers. However, the causal nature of these associations is still unresolved, as both risk factors and pre-existing disease may alter hemostatic factor levels, generating associations between hemostatic factors and disease which are noncausal.
4.12 Socioeconomic Position
In most industrialized countries CHD risk is higher amongst people living in worse social circumstances. Whether the apparent gradients in the opposite direction seen during the early stages of the CHD epidemic in industrialized countries, and in newly industrialized countries currently, are real or reflect differential disease coding and reporting, remains uncertain (Davey Smith 1997). Social disadvantage can influence CHD risk in a wide variety of ways, and act across the entire life-course. People born into worse social circumstances are likely to have lower birth-weight. Socioeconomic deprivation in childhood is associated with poor nutrition and growth, and possibly higher incidence of childhood infections. Behavioral patterns—in particular with relation to diet, physical activity, alcohol consumption, and smoking—are developed in childhood in a socially patterned manner and track into adulthood. In most industrialized countries smoking and dietary patterns associated with increased CHD risk are more common among poorer adults.
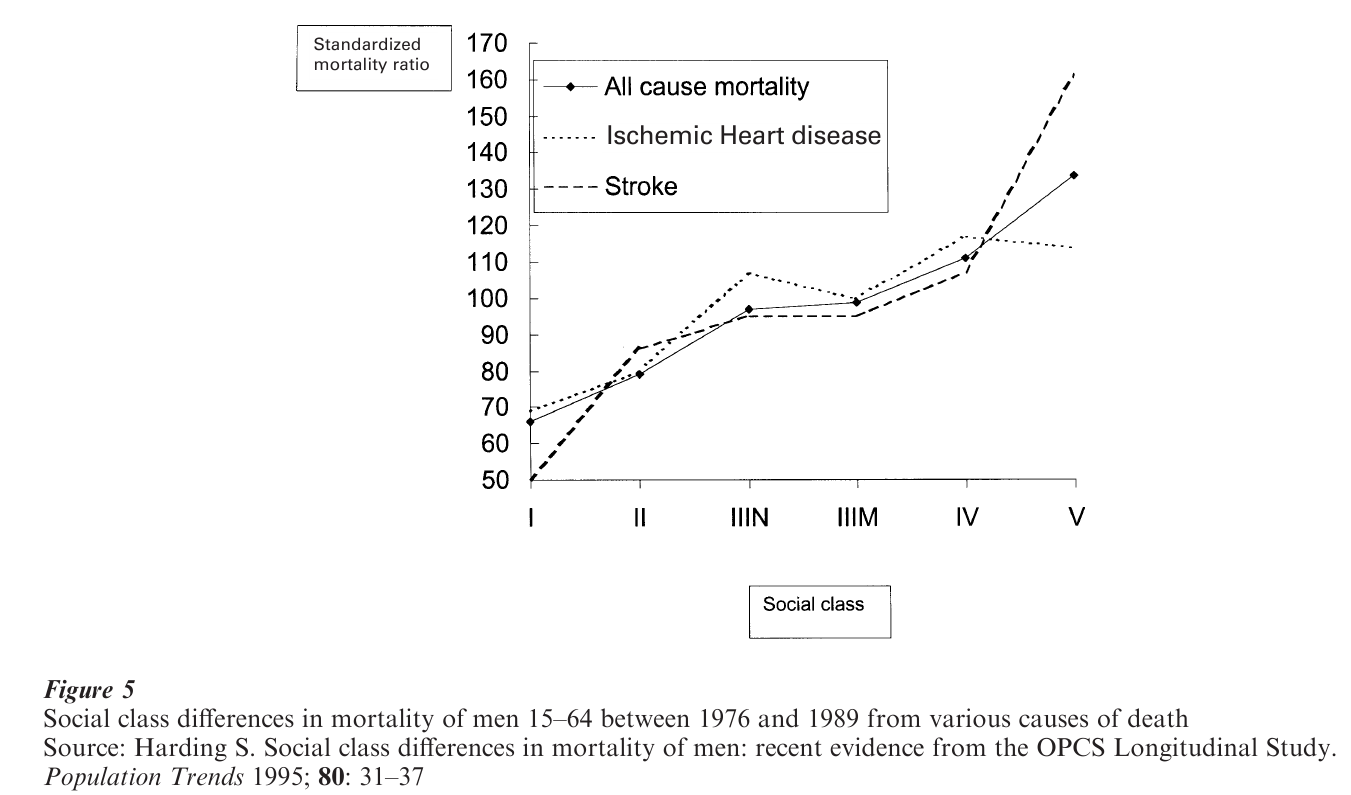
Given this wide array of exposures associated with socioeconomic deprivation which could increase the risk of CHD, it is not surprising that studies which have taken into account a limited number of these find they fail to account fully for the socioeconomic distribution of CHD. The large (and in many countries increasing) socioeconomic differentials in CHD risk provide both a model for testing etiological hypotheses and also evidence of an important potential locus for public health interventions. Figure 5 shows the three-fold difference in CHD mortality between men in unskilled manual occupations in Britain compared to those in managerial and professional occupations, and the graded difference in risk between these occupational extremes. Clearly, reducing CHD risk among the less socioeconomically advantaged to the same level as that of the most advantaged would have a dramatic influence on overall diseases rates in the population. A further implication is that since socio-economically disadvantaged people have a considerably increased risk of CHD, which is not purely dependent upon conventional risk factors, they have the most to gain from intervention.
4.13 Stress
Stress is considered by the general public to be an important cause of CHD. Stress is, however, difficult to define or measure. Epidemiological studies have examined a wide range of potential exposures that fall under the general heading of ‘stress.’ These include measures which are essentially of personality traits— such as the Type A behavior pattern—through to records of stressful life events or global measures of perceived stressfulness of daily activities. A broader conceptual category of ‘psychosocial factors’ is now widely used in the epidemiological literature. This includes aspects of social life such as the strength of social support networks or the level of control over their work which people have.
The type A behavior pattern was investigated from the 1950s as a potential cause of CHD. Type A individuals—those who are involved in an incessant struggle to achieve more and more in less and less time—were found to have higher risk of CHD in several early prospective studies (Labarthe 1998). More recent studies have failed to find any association between type A behavior and CHD. It may be that this association no longer exists because CHD is not now considered a disease of the wealthy, stressed, businessman, who in the past was more likely to be diagnosed with the condition. Research on behavioral traits now focuses on those elements of the original type A classification, which are related to adverse social background (such as hostility). These may predict CHD risk because of this, rather than because of any causal link with the disease. Ongoing studies should help to resolve this issue in particular trials of stress management instituted to establish whether interventions in this area can produce beneficial changes.
Measures of self-reported global stress and other self-reported indicators such as low control at work or poor social networks tend to be related to self-reported CHD symptoms. They less consistently relate to objective measures of CHD. This may reflect an underlying reporting tendency such that people who report higher levels of adversity also report higher levels of symptoms. People with low control over their work (e.g., shift workers in a factory) are, in general, in less favorable social locations than those with higher control over their work. It is not surprising that the former have higher rates of CHD, given the strong social patterning of the disease. Whether these adverse psychosocial factors are one of the causes of the high CHD mortality in the less advantaged or is merely another consequence of material inequalities is currently not clear.
Further, more methodologically robust, studies employing objective measures of both stress and CHD outcomes are required. It is remarkable that the supposed biological mediators between stress and disease–disturbed functioning of the hypothalamo-pituitary-adrenal axis and possible immune system outcomes of this—have not themselves been related to CHD risk in prospective observational studies. The current controversy—with enthusiastic proponents of stress as a cause of CHD on one side lined up against the majority of academic and research cardiologists and epidemiologists who dismiss the association as spurious—will only be resolved when studies employing better methods report their findings.
5. Lifecourse Approach
The long incubation period for CHD has been recognized for many years (Rose 1982), and a life-course approach to its etiology is a natural extension of this view. In this discussion we have focused on studies for which the main focus is the social patterning of CHD risk.
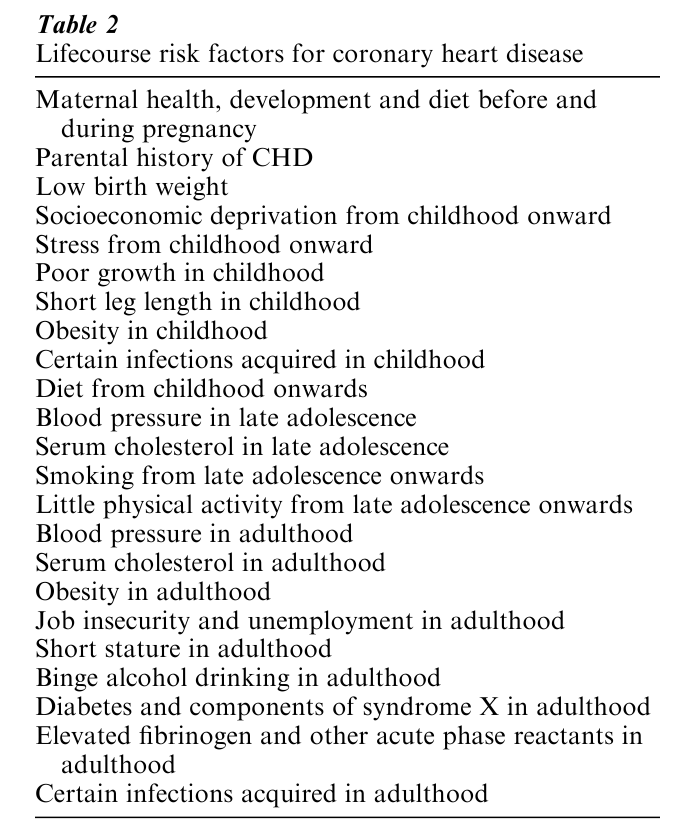
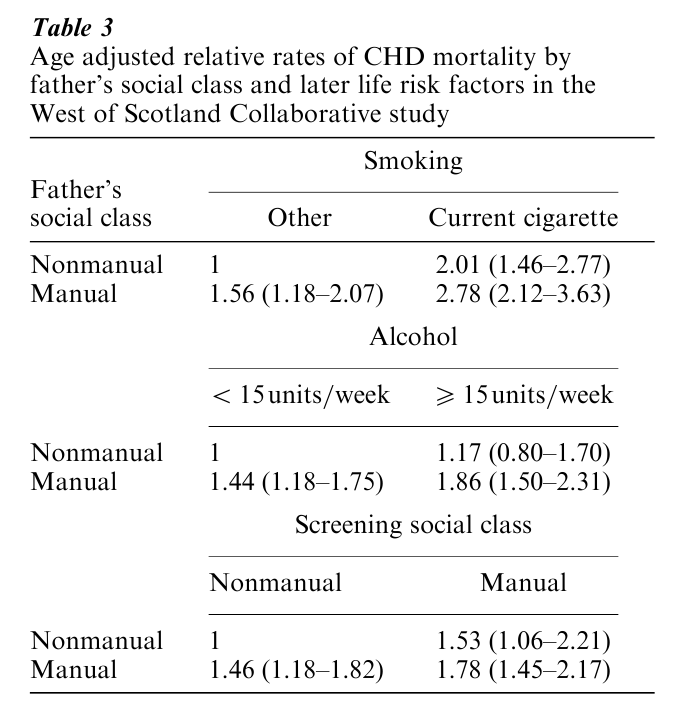
However, most of the important risk factors identified for CHD are socially patterned. Table 2 summarizes factors which are putative or established CHD risk factors and/or are of particular interest from a life-course perspective, according to their period of influence. It is clear that CHD can be considered the archetype of diseases whose determinants should be sought across the entire life-course—from conditions existing at the time of conception and during intrauterine development, through nutrition, growth, and health in childhood, to social conditions, occupation, diet, physical activity, and smoking throughout adult life. In Table 3, we combine a marker of early life circumstances—father’s social class—and behavioral and socioeconomic factors acting in adulthood and demonstrate their joint influence on CHD mortality. If factors acting at different stages of life—such as childhood social circumstances, education, deprivation level of area of residence in adulthood, adulthood occupational social class, smoking, and drinking in adulthood—are combined, then very large differences in cardiovascular disease risk can be observed (Davey Smith and Hart 2001). Socioeconomic inequalities in CHD can only be understood through consideration of how a variety of exposures which increase CHD risk are influenced by social circumstances, how this social dependence leads to them clustering across time, such that some individuals are adversely influenced by a wide array of risk factors, and thus how the accumulation of—and interaction between—influences acting at different stages of life determines the pattern of CHD within and between populations.
6. The Prevention Of Coronary Heart Disease
There are two differing but complementary approaches to prevention: the high-risk approach and the population approach. The high-risk approach seeks to identify those at highest risk of developing disease and intervene to prevent disease. With this approach it may be easier to encourage people at high risk to alter their lifestyles as these people have a considerable amount to gain personally. The recent results from the WHO MONICA study seem to confirm that the widespread use of effective treatments can reduce the number of symptomatic episodes and deaths attributed to CHD. Such an approach, how-ever, requires that those at high risk be identified and ignores the people who develop symptomatic disease who are at moderate risk. For example, in the Whitehall study only around 40 percent of the coronary deaths occurred in the 20 percent at highest risk.
The alternative approach is the population approach, which seeks to alter behavior across the whole population. The advantage is that it is likely to produce large improvements in population health, for fairly modest changes in behavior. The disadvantage is that the absolute benefit for each individual who makes a lifestyle change is small. This mismatch between the likely size (Rose 1985) of the benefits to the individual and population has been called the ‘Prevention paradox.’
It has been shown that brief advice from physicians leads to small, but worthwhile, reductions in smoking rates. Nicotine replacement gum can also aid smoking cessation. School-based antismoking programs have, however, shown disappointing results. The detection and treatment of high blood pressure reduces the risk of CHD and has the added benefit of substantially reducing the risk of stroke. Similarly, lowering cholesterol levels with the statin drugs reduces CHD risk in primary prevention.
Health-related behaviors are influenced strongly by societal, legislative, and fiscal forces, perhaps more so than by individual levels of knowledge and degree of willpower. This is the case with smoking, where cigarette use in a country is responsive to the competing incentives offered by tobacco companies and government policies. The prevention of smoking can only be ultimately successful if the world community accepts the need to restrict the growing, marketing, and use of tobacco.
The differences in both behaviors and CHD disease rates clearly illustrate the capacity for populations to change. While simple invocations have modest effects on behavior, social change can result in profound improvements in health. Conversely, where cultures fail to adapt or social structures collapse (as happened in Russia with the demise of the Soviet Union) CHD can increase. Effecting societal change is complex but the potential public health benefits are profound. The concentration of CHD among those in society who are least advantaged suggest that any such policies will be more effective if we seek to improve their lot by improving their income, opportunities, and self- esteem. More inclusive and extensive programs that seek to reduce inequalities in health and improve health for all offer real opportunities to reduce CHD.
Bibliography:
- Barker D J P 1998 Mothers, Babies and Health in Later Life. Churchill Livingstone, Edinburgh, UK
- Barrett-Connor E 2001 Hormone replacement therapy: Risks and benefits. International Journal of Epidemiology. 30: 423–6
- Collins R, MacMahon S 1994 Blood pressure, anti-hypertensive drug treatment and the risks of stroke and coronary heart disease. British Medical Bulletin 50: 272–98
- Davey Smith G 1997 Socioeconomic diff In: Kuh D, Ben-Shlomo Y (eds.) A Life Course Approach to Chronic Disease Epidemiology. Oxford University Press, Oxford, UK, pp. 242–73
- Davey Smith G, Hart C 2001 Life-course socioeconomic and behavioral influences on cardiovascular disease mortality: The collaborative study. American Journal of Public Health
- Ebrahim S, Davey Smith G, McCabe C, Payne N, Pickin M, Sheldon T A, Lampe F, Sampson F, Ward S, Wannamthee G 1998 Cholesterol and coronary heart disease: Screening and treatment. Quality in Health Care 7: 232–9
- Evans A 1995 Dr. Black’s favourite disease. British Heart Journal 74: 676–7
- Gunnell D J, Davey Smith G, Frankel S, Nanchahal K, Braddon F E M, Pemberton J, Peters T J 1998 Childhood leg length and adult mortality: Follow up of the Carnegie (Boyd Orr) survey of diet and health in pre-war Britain. Journal of Epidemiology and Community Health 52: 142–52
- Labarthe D R 1998 Epidemiology and Prevention of Cardiovascular Disease: A Global Perspective. Aspen, Gaithersburg, MD
- McCarron P, Davey Smith G, Okasha M, McEwen J 2000 Blood pressure in young adulthood and mortality from cardio-vascular disease. Lancet 355: 1430–1
- Neaton J D, Wentworth D 1992 Serum cholesterol, blood pressure, cigarette smoking and death from coronary disease: Overall findings and differences by age for 316,099 white men. Archives of International Medicine 152: 56–64
- Peterson S, Mockford C, Rayner M 1999 Coronary Heart Disease Statistics. British Heart Foundation, London
- Powles J W 1994 Greek migrants in Australia: Surviving well and helping their hosts. In: Marks L, Worboys M (eds.) Migrants, Minorities and Medicine: Historical and Contemporary Perspectives. Routledge, London
- Rose G 1982 Incubation period of coronary heart disease. British Medical Journal 284: 1600–1
- Rose G 1985 Sick individuals and sick populations. International Journal of Epidemiology 14: 32–8




