View sample migrants’ health research paper. Browse research paper examples for more inspiration. If you need a health research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Definition Of Migrants, Demography, And Types Of Migration
Definition Of Migrant
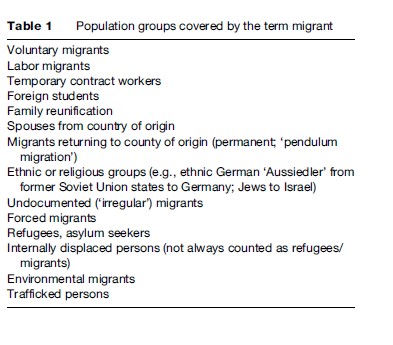
Migrants are individuals who move from one country or place of residence to settle in another. The move can be either across an international border or within a state, and it can be temporary or permanent. People migrate for economic reasons or to join their relatives; others are refugees, displaced persons, or uprooted people. Voluntary migrants are those who have made their own decision to migrate; the decision could, however, have been brought about due to economic or other pressures. Forced migrants are people who have to move because of external factors such as individual persecution, general conflict, or natural disasters (Braunschweig and Carballo, 2001; IOM, 2005). Any such classification remains theoretical, however. Often, push-and-pull effects are at work simultaneously; whether the migration is permanent may only be decided in the future, or the decision may be revised. Table 1 provides an overview of population groups covered by the term migrant.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
For health reporting and epidemiological purposes, foreign-born persons or holders of foreign passports are categorized as migrants. This underestimates the profound heterogeneity of foreign-born populations: they may be migrant workers, refugees, asylum seekers, or students. Their history and legal status, in turn, affects health determinants and outcomes. The offspring of immigrants may face similar problems but often do not appear in routine migration statistics because they are not foreign-born. Different regulations make comparisons of the health status of migrants between neighboring countries difficult.
Number Of Migrants Globally And Sex Distribution
The number of international migrants worldwide has been increasing steadily over the last decades and is expected to continue doing so. In 1960, there were 76 million international migrants globally (IOM, 2005). By 2000, this number had reached an estimated 175 million, meaning that 1 out of every 35 persons in the world was an international migrant (Table 2). The total number was predicted to rise up to between 185 and 192 million by early 2005 and to reach 230 million by 2050 (IOM, 2005).
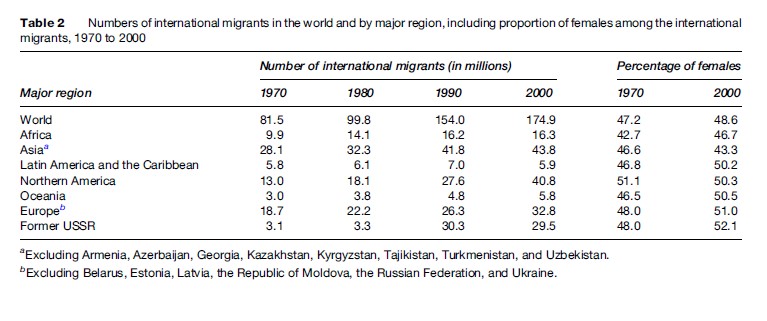
The proportion of women migrants went up from 47% in 1970 to 49% in 2000, and is higher in developed than in developing regions (Table 2). It is usually easier for men than for women to migrate legally: Efforts to recruit labor frequently focus on employment in construction and agriculture, which tends to be male-dominated.
Changing Motives For Migration
People have been moving from one place to another, internally and across borders, throughout human history. Contemporary movement, however, differs significantly from that of past times. Continued economic disparities within nations – between rural and urban areas, regions or states, and among nations – have always played an important role in furthering internal and international migration. Today’s migration patterns and the environment in which people migrate are defined by economic and humanitarian crises. In addition, modern communication and transportation, as well as the opening up of borders between countries and regions, have made it possible for people to travel farther, faster, and more easily than ever before. Migration has become a global issue, with all states of the world now functioning as either points of origin, transit, or destination, and, at times, all three at once (UNFPA/IMP, 2004; IOM, 2005). In 2000, the United States was the country with the largest number of international migrants with 35 million people, equivalent to 20% of world migrant stock. Regionally, Asia (excluding Armenia, Azerbaijan, Georgia, Kazakhstan, Kyrgyzstan, Tajikistan, Turkmenistan, and Uzbekistan) had the largest number: 43.8 million, or 25% of world migrant stock (IOM, 2005).
Traditional countries of immigration such as Australia, Canada, and the United States continue to be attractive destinations for international migrant workers. However, recently there have been significant shifts in labor migration. In the 1980s, for example, economic development in Japan and in East and Southeast Asia offered alternative destinations for migrant workers from economically less well-off countries in the region (IOM, 2005). In sub-Saharan Africa, the political liberalization of the Republic of South Africa in the 1990s and the continued deterioration in the economies of many neighboring countries led to a marked increase in migrant flows from the region into that country (Gushulak and MacPherson, 2004).
Internal migration, although often voluntary or economically based, can also be involuntary due to environmental degradation, natural disaster, human rights abuse, or political upheaval and armed conflict. Currently, 25 million persons in more than 50 countries are internally displaced due to conflict. While they remain within the borders of their own country, they are often without access to basic services such as health care and education, and beyond the reach of international aid organizations (UNFPA/IMP, 2004).
Migration: A Challenge To Individuals And Societies
Migration offers opportunities and is associated with risks – for individual migrants and their families, for the societies from which migrants originate, and for the receiving countries. Many countries are not well prepared and lack policies needed to make migration a healthy and socially productive process. This has public health implications for the people who move, for the families they have left behind, and for the communities they come in contact with during transition or in the host countries (Carballo and Nerukar, 2001).
Migration And Health
Under normal circumstances migration in itself should not pose a risk to health. However, the conditions surrounding the migration process can increase vulnerability for ill health. Some of the health risks are related to the conditions before departure, to travel conditions, and to the arrival or transit stage. The reasons why the movement is taking place – whether the individual can control them or not (voluntary or forced migration), the mode of movement, as well as the regulations and level of acceptance in the receiving country – all play a role in determining the health of migrants (Braunschweig and Carballo, 2001; IOM, 2004). These factors are examined later.
Exposures In Country Of Origin
Persons fleeing persecution, leaving areas with high disease prevalence or limited access to health care, are likely to have different health profiles from those voluntarily emigrating from countries where health services are optimal and disease prevalence is low. A considerable number of migrants come from developing countries where infectious diseases such as tuberculosis (TB) and HIV/AIDS contribute significantly to morbidity. Persons originating from such a country and migrating to a developed country have, at the time of arrival, a higher risk of suffering from these diseases than persons of the same age in the general population of the country of destination (Cookson et al., 1998; Carballo and Nerukar, 2001; Razum and Twardella, 2002; Gushulak and MacPherson, 2004; IOM, 2004). The problem is compounded by poor living conditions and the barriers to accessing preventive and curative health care that migrants often face (see following section titled ‘Access to health services’).
Between 1995 and 2000, the incidence of TB cases in Denmark increased steadily and the proportion of foreign-born persons among all cases rose from 18% in 1986 to 60% in 1996. Approximately 40% of all TB infections in England and Wales are occurring in immigrants from the Indian subcontinent. The incidence of TB in the Netherlands rose by 45% between 1987 and 1995, with more than half of the new cases being reported among immigrants. In Germany and France, migrants are three to six times more likely to be diagnosed with TB than nonmigrants. The risk of HIV/AIDS among migrants in many EU countries reflects the global epidemiologic pattern of the disease. For example, migrants of African origin residing in Sweden have a higher HIV/AIDS incidence than Swedish nationals. A similar pattern can be observed in Germany, where the number of HIV-infected persons among migrants is rising (Carballo and Nerukar, 2001; Robert Koch-Institut, 2005a, 2005b).
Exposures in the country of origin can also be to the benefit of migrants. Lifestyle factors such as diet, tobacco, and alcohol consumption are often more favorable for health in developing than in developed countries. With regard to smoking, the proportion of smokers in lower income countries might be higher, but the amount consumed per person will often be substantially lower than in the high-income countries. Besides lung cancer, the incidence of breast cancer and colon cancer also tends to be lower. Studies show that migrants ‘take along’ their low risk for some chronic diseases and keep this advantage for many years, depending on the adopted lifestyle in the host country and the lag time of the disease in question. The risk of diseases, such as stomach cancer and stroke that are associated with poor hygienic and living conditions in childhood, tends to be higher, however (Razum and Twardella, 2002).
Patterns Of Mobility (Regular Versus Irregular)
Movement as such can constitute a considerable and immediate health risk if it involves fleeing, forceful displacement, or illegal crossing of borders. Planned migration, in which the necessary travel documents have been organized beforehand and entry requirements are met, will be safer than a journey taken clandestinely or under duress.
Health Risks Of Irregular Migration
In June 2000, an attempt by 54 Chinese would-be immigrants to enter the United Kingdom in a sealed truck designed to carry fruit ended in their death by suffocation. Thousands of people are taking similar risks on a daily basis, with many of them losing their lives in the process. The death toll at sea among Africans and Albanians trying to enter Europe through Spain and Italy, respectively, is giving rise to international concern (Carballo and Nerukar, 2001).
The International Organization for Migration (IOM) reports that the number of irregular migrants is increasing. Precise figures are not available, but IOM estimates that one-third to one-half of migrants to developed countries travel without documents or with false ones, which is said to constitute an increase of 20% over the past 10 years (UNFPA/IMP, 2004). Correspondingly, the number of migrants in an irregular situation (which includes persons who enter legally but whose legal status has expired) within a country is difficult to estimate. Irregular migration does not necessarily involve traffickers; however, trafficking and smuggling of humans have become major criminal enterprises, often involving exploitation and abuse. Women and children are more vulnerable than men (Carballo and Nerukar, 2001; UNFPA/IMP, 2004).
Healthy Migrant Effect
It has frequently been observed that migrants have a lower mortality (and occasionally also morbidity) compared to the majority population of the host country, in spite of being socioeconomically disadvantaged. This phenomenon is known as ‘healthy migrant effect.’ Attempts to explain it have focused on a selection or self-selection of particularly healthy individuals into migration and on the differentials in risk of chronic diseases (e.g., cardiovascular disease) between populations. Hence, people migrating from countries with low mortality from coronary heart disease (CHD) to countries with high cardiovascular disease (CVD) mortality, initially experience a mortality advantage. Examples for such a scenario are the migration from southern to northern Europe and from Latin American countries to the United States. Due to the long lag periods in chronic disease, such mortality advantages may persist for years or even decades after migration (see following paragraph). Ultimately, as was shown in the Nihosan study of Japanese men migrating to Hawaii and San Francisco, mortality rates converge with those of the majority population. There is considerable evidence that initially advantageous cause-specific mortality rates of immigrants may turn into a mortality disadvantage when socioeconomic conditions are unfavorable and access to health care is difficult.
Exposures In Country Of Immigration
By migrating to industrialized countries, migrants from lower-income countries benefit from environmental and public health measures that prevent the epidemic spread of infectious diseases, and from better access to biomedical care that provide a cure for many conditions (Razum and Twardella, 2002; Razum and Geiger, 2003). Changes in lifestyle (diet, tobacco, alcohol) can quickly lead to unfavorable changes in risk factor profiles for cardiovascular disease, lung and colon cancer, and other noncommunicable diseases. Due to long lag periods, disease and death rates may show appreciable increases only after decades of exposure. This potentially positive situation becomes problematic when public health policies of the host countries only target the general population but elude migrants.
Migrants are exposed to an excess risk of contracting infectious diseases even in high-income countries. For example, many migrant workers travel without their spouses or partners and might resort to unsafe sexual practices, thereby risking the contraction of sexually transmitted diseases (STDs). In Belgium and Sweden, the number of STD cases among foreign-born men is higher than that of men born in the two countries (Carballo and Nerukar, 2001).
Social Class
Social class is a strong determining factor for health. Migrants, upon the time of arrival, frequently become part of the lower social stratum of the host country. They then are exposed to similar risk factors, and face similar health risks, as the lower social class within the general population, such as a high smoking prevalence and poor working as well as housing conditions.
Housing can both determine the health of people, as well as indicate the quality of life they enjoy and are allowed to enjoy. Many migrants arrive with little money and usually have temporary official status that does not allow them to ‘invest’ in good-quality housing. Often this is further reinforced by social barriers. Newcomers from abroad (or rural areas in the case of rural to urban migration) tend to move to low-income areas of towns and cities where they are exposed to crowding, substandard housing, and poor sanitation (WHO, 2003). The situation is more problematic for seasonal workers.
In an agricultural site in southern Spain, 85% of the workers were living in crowded temporary structures. These were situated in close proximity to greenhouses and warehouses where pesticides were used and stored. In Portugal, more than three-quarters of migrant shantytowns had no running water, toilet facilities, electricity, or refuse collection (Braunschweig and Carballo, 2001).
Exposure to poor housing, hazardous working conditions and social disruption is also common among migrant workers in various parts of Africa (WHO, 2003). In many industrialized countries, asylum seekers who formally lodge application for refugee status are confined in detention centers. These centers are generally overcrowded, increasing the risk of spread of infectious diseases.
Between October 2001 and October 2002, 56 cases of active TB, many with pulmonary involvement, were diagnosed among residents of an overcrowded migrants’ shelter in Paris. The outbreak was the result of transmission that had occurred in France, as became evident from the clustering of the cases in time and place, the large number of cases with early-stage disease, and from typing of the isolates (Valin et al., 2005).
Choosing to live in proximity of persons of the same ethnic ancestry can, however, also be one of the coping strategies used by migrants. By living close together, migrants of similar ethnic background can maximize social interaction and maintain group norms and values. Furthermore, a large size and concentration will help ensure the success of ethnic clubs, churches, language newspapers, and specialty stores (Balakrishnan and Maxim, 2005).
Being a migrant can affect the socioeconomic situation in ways different from those experienced by the host population. One example is de-skilling, or ‘brain waste,’ which relates to the considerable number of highly skilled migrants who work as unskilled labor. University graduates from Africa and Latin America often fail to find jobs in their fields of training after migration to industrialized countries; doctors or engineers may end up earning a living as cleaners or taxi drivers. Doctors from the former Eastern Block countries face difficulties when seeking recognition of their medical qualifications in western European countries. In Sweden, the unemployment rate for migrants with a tertiary level education is twice as high as that of the native-born population with similar qualifications. De-skilling is assumed to lead to psychosocial and health problems (see following section titled ‘Psychosocial problems particular to migrants’).
Migration And Gender
Women are marginalized in many societies in respect to education, employment, goods and services, and basic human rights. By migrating to industrialized countries, they may improve their opportunities in personal, educational, and economic terms. However, women with a migration background have a higher probability of working in gender-segregated and unregulated sectors of the economy such as domestic work, entertainment, and sex industries. They are more exposed to forced labor and to sexual abuse by employers or by personnel and inhabitants of refugee camps than men or women of the majority population (UNFPA/IMP, 2004).
Migration can also be stressful and traumatic for women due to the loss of their established social setting and familiar surroundings. Their initial lack of education and occupational experience may limit their social integration in new settings. Moreover, second-generation immigrant girls and women may experience substantial pressure from their parents to conform to traditional values that may not be compatible with the lifestyle of their peers from the majority population. In the case of forced migration (see section ‘Irregular Migration and Trafficking in Persons’), women are greatly disadvantaged. In complex emergencies such as war, the social cohesion characteristic of stable societies is disrupted and families are dispersed, increasing people’s vulnerability, especially that of women (Carballo et al., 1996; IOM, 2005).
Access to Health Services
In many countries, migrants have limited access to health services in comparison to the majority population. Health-care-seeking behavior is culturally determined, so migrants have to overcome cultural as well as language barriers. People coming from countries or regions of countries where services may have been lacking will have developed coping strategies that make them more fatalistic about disease, more tolerant of pain, and less likely to seek help when ill (Braunschweig and Carballo, 2001; Carballo and Nerukar, 2001). Language problems and lack of information regarding the location and structure of local health services often limit the capacity of migrants to make optimal use of services. Many migrants cannot communicate with health providers effectively. Few countries routinely use interpreters in health-care facilities or provide multilingual information packs, which also include visual and audiovisual media (Razum and Geiger, 2003).
The different cultural understandings of health and concepts of disease make communication and interaction with migrants more difficult. Culture influences the interpretation and presentation of symptoms, as well as the treatment expected. In many cultures, illness is perceived as coming from ‘outside.’ Health care in industrialized countries, which is based on a biomedical paradigm, does not adequately respond to the migrants’ perception. This can lead to misdiagnoses, inappropriate treatment, and poor compliance on the part of the patients (Braunschweig and Carballo, 2001; Razum and Geiger, 2003).
The legal status of migrants also determines their level of access to health and social services provided in the host country. Legal immigrants, permanent residents, and other long-term migrants often have the same access to health and social services as the local population. The access to health services for asylum seekers varies widely. Most countries provide medical screening to asylum seekers upon arrival, followed by limited access during the processing of their asylum claims. This might take months or years. Although the reasons for these restrictive policies vary, they share one underlying aim: to reduce health and welfare costs (IOM, 2005; Norredam et al., 2005).
Psychosocial Problems Particular To Migrants
Even under the best of conditions, the process of migration often entails uprooting, and separation from family and familiar surroundings, as well as traditional values. Migrants find themselves in new social and cultural situations in which job and legal security may be minimal. Highly educated migrants often consider themselves to be overqualified for the jobs they hold (see the paragraph about de-skilling in the preceding section titled ‘Social class’). For many, social integration is difficult. The loss of status and social support can lead to dissatisfaction and depression (Carballo and Nerukar, 2001; Razum and Geiger, 2003).
Persons fleeing war and victims of trafficking may experience posttraumatic stress; this may lead to heightened aggression and health-related problems. Their condition may be aggravated by overcrowding and poor living conditions in migrant detention centers and by the way they are treated. Detention is an additional stressor for asylum seekers that may worsen psychological symptoms. Often, there are no mechanisms to identify victims of torture or sexual abuse in need of specialist care (Braunschweig and Carballo, 2001; Steel and Silove, 2001).
Stigma and discrimination (overt and implicit) can lead to, or aggravate, psychosocial problems. Whereas stigma refers to perceiving certain population groups – for example, because of their ethnic origin – as inferior, discrimination describes the practical consequences of stigmatization in everyday life and in health care. Migrants face stigma and discrimination depending on their country of origin, their religion, and even more so when they are living with stigmatized diseases such as HIV/AIDS.
Working Conditions
Migration for employment is not always safe, and in some cases is not covered by regulations protecting migrant workers. Migrants frequently obtain jobs that are temporary, poorly paid, require low skills, and are therefore unattractive to local labor forces. Carballo and Nerukar (2001) report that the number of industrial accidents and injuries in construction and public works fields is higher among migrant workers than among citizens in many western European countries. Work-related risks are compounded by language barriers, poor communication, a lack of familiarity with the technology used, and by different attitudes to work safety. For example, it is not uncommon that migrant workers are insufficiently protected against exposure to pesticides and other chemical products. Long-term exposure to such products has been linked to depression, neurological disorders, and miscarriages (Carballo and Nerukar, 2001). These problems are compounded where migrant child labor is concerned. Hispanic children of migrant farm workers make up a considerable proportion of farm labor in the United States. These children face even higher risks of injury or death from accidents than their elders (IOM, 2005).
Irregular Migration And Trafficking In Persons
Irregular migration not only poses the highest risk to migrant health; it is also a public health concern in regard to communicable disease control, reproductive health, occupational and environmental health, and sanitation. Undocumented migrants often live in crowded, unsanitary conditions that add to their health risks. When ill, they may not be able to access health services for fear of being reported to immigration authorities and being deported. Providing preventive services for these populations is particularly challenging (Braunschweig and Carballo, 2001; WHO, 2003; Gushulak and MacPherson, 2004; IOM, 2005).
Trafficking, according to the UN General Assembly, is ‘‘the recruitment, transportation, transfer, harboring or receipt of persons, either by the threat or use of abduction, force, fraud, deception, coercion, or by the giving of unlawful payments or benefits to achieve the consent of a person having the control over another person for the purpose of exploitation’’ (UN General Assembly, 1999: 3). Health-related issues are among the most severe consequences of trafficking in persons. Trafficked persons often fall victim to various forms of sexual and physical abuse, which can have devastating and lasting effects on their mental, reproductive, and general physical health and well-being (IOM, 2005). The trafficking of children and adolescents for economical and sexual exploitation demands special attention (Tautz et al., 2006).
Migration And Reproductive Health
Changes in social and economic environment, differential access to health care, changes in sexual behavior and social status affect reproductive health, especially among women. Language or cultural barriers can lead to unfavorable health consequences, for example, during pregnancy. In several EU countries, migrants have a higher proportion of difficult pregnancies, and experience more pregnancy-related illnesses and complications, relative to local women (Razum et al., 1999; Carballo and Nerukar, 2001). In Sweden, for example, Ethiopian and Somali women have an increased perinatal morbidity compared to the general population, while in Denmark ethnic minority and migrant women underuse reproductive checkups (Ackerhans, 2003). In Spain, migrant women from sub-Saharan Africa and Central and South America have particularly high rates of premature births, low birth weight, and complications of delivery (Carballo and Nerukar, 2001).
Perinatal and neonatal mortality rates are frequently higher among immigrants than in the host population. In the UK, perinatal and postnatal mortality rates are higher among immigrants born in Pakistan and the Caribbean than in the general population; a similar gradient is visible among Turkish immigrants in Germany. In Belgium, Turkish immigrants experience perinatal and infant mortality rates that are 3.5 times as high as those of Belgian women (Carballo and Nerukar, 2001; Razum and Geiger, 2003). Conflicting values, as described in the previous section titled ‘Migration and gender,’ may limit access to contraceptives and to strategies for women to protect themselves against sexually transmitted diseases. A lack of adequate information on contraception, and on where to obtain appropriate advice, is common among immigrant women, in particular among those from the north and sub-Saharan African countries (Carballo and Nerukar, 2001).
Migration And Aging
Due to steady increases in migration and the temporal nature of work migration in many settings, migrant populations are often young in comparison to the host populations. Social and health services are often not prepared for elderly migrants who remain in the host country. Often, the migrants themselves are unprepared, because they had always planned to return to their country of origin. Elderly Turkish work migrants in western European countries, for example, increasingly decide not to return to Turkey where access to health care is more restricted, or where they cannot be close to their children who grew up in the host country and decided to stay there (Razum et al., 2005).
Effects On Health-Care Systems
International migration poses challenges to health-care systems in various ways, both in countries of origin and in host countries of migrants. Developing countries are losing many of their better-educated nationals to richer countries (brain drain). For example, up to 75% of persons emigrating from Africa to the United States, Canada, or to OECD (Organisation of Economic Cooperation and Development) countries are assumed to have completed university-level or equivalent technical training/tertiary education (Saravia and Miranda, 2004). This brain drain includes trained health workers, thus affecting the health-care delivery in countries of origin. Host countries of migrants, however, have to adapt their health-care systems to the needs of heterogeneous minority populations.
Brain Drain In Health Care
Unsatisfactory working conditions, poor remunerations, a high risk of infection, lack of equipment, and lack of further education opportunities are some of the reasons why health-care workers such as physicians, nurses, dentists, and pharmacists leave their countries (Bach, 2003; Diallo, 2004; Saravia and Miranda, 2004; Stilwell et al., 2004). The proportion of trained health workers that has migrated from individual developing countries is not usually known, as the characteristics of emigrants are rarely recorded. Vacancy levels in the health services can serve as a proxy indicator for the brain drain. A 1998 survey of several African countries showed widely varying vacancy levels for medical personnel in the public health sector. For example, a 7.6% vacancy level was reported for doctors in Lesotho compared to 72.9% for specialists in Ghana. Malawi had a vacancy level of 52.9% for nurses. The impact of migration of health-care workers on such countries, which generally have few health workers to start with and whose capacity for reinvestment in education is limited, can be devastating. The loss of health-care professionals almost inevitably leads to inadequate coverage and difficulties in meeting some of the population’s health needs. In addition to having to continue working under poor conditions, the health professionals who stay behind also experience higher workloads and additional stress. This might undermine their motivation to work in their current settings and lead to further migration (WHO, 2003; Stilwell et al., 2004; UNFPA/IMP, 2004). To mitigate effects on the source countries, mechanisms have to be developed so that migration of health workers remains temporary, contributes to their further education, and leads to indirect development support through remittances (Bach, 2003; IOM, 2005).
Brain Gain In Health Care
Doctors and nurses in developed countries also complain of low salaries and poor working conditions in the public sector. More and more of them are joining the private sector or leaving their countries for better-paying jobs. To make up for the loss in manpower, the affected countries are turning to developing countries, mainly in Africa and Asia, for personnel. Examples of this brain gain are as follows: the UK loses about 8000 nurses every year through emigration to Australia, the United States, Canada, Ireland, and New Zealand, and recruits 15 000 from overseas. Without the sustained increase in overseas nurses employed, the United Kingdom would not have been able to reach its 2004 goal of increasing the nursing workforce by 20 000. And, as another example, at least 20% of physicians working in Australia, Canada, and the United States are supposedly from other countries, with a considerable proportion of them from developing countries (Diallo, 2004; Saravia and Miranda, 2004; Stilwell et al., 2004). This phenomenon is not restricted to Europe and the United States: South Africa, which loses almost half of its newly qualified doctors to Canada, the United Kingdom, and Australia, attracts health personnel from poorer countries such as Kenya, Malawi, and Zimbabwe. Eighty percent of the doctors working in South Africa’s rural areas come from these three countries (Diallo, 2004).
Challenges For Public Health In Countries Of Immigration
Healthy migrants are more likely to be successful in education and employment, and to actively participate in society. Investing in migrant health thus aids their effective integration into communities and makes sense even when seen solely in economic terms (IOM, 2005). Successful integration calls for a comprehensive interpretation of migrant health, comprising not only infectious disease control, but also chronic noncommunicable conditions, mental health concerns, and human rights issues (Grondin, 2004). Providing appropriate services for a minority group such as migrants not only promotes understanding and cohesion in mixed societies; it can also serve as a model for making health systems more responsive to the diverse needs of all clients, irrespective of their nationality or geographic origin (thus employing ‘diversity management’). Unfortunately, many politicians see the challenges that migrant health poses to health systems in terms of expenditure rather than investment, and cost rather than benefit.
Health systems, as well as migrant populations, are too diverse, and public health needs too contextual, to offer general advice. There are a number of issues, however, that are pertinent in many different settings. These include: Health information needs. Reliable data on the health status, behavior, and health resources of migrants need to be collected, analyzed, and reported in a systematic way so that public health policy is based on sufficient information. A relevant practical problem is an appropriate definition of migration status in health statistics. However, information regarding such statistics is often restricted – for example, to nationality or country of birth – thus failing to identify second-generation immigrants.
Language. Health systems in many countries with migrant populations still lack interpreter services and visual aids to lower language barriers in communication.
Seemingly ‘pragmatic’ solutions, such as asking relatives or menial hospital staff of the same origin to act as translators, are unacceptable, both in terms of privacy and of quality of information obtained.
Preventive interventions. Motivating migrants to take up preventive activities is often difficult. A frequent response consists of uncoordinated activities by various well-meaning, and often small, activist groups. Few of the interventions are evidence-based, and sustainability is doubtful after funding runs out. Whereas the importance of such activities should not be denied, networking among the groups is essential. Until interventions and ways of accessing migrant groups have been evaluated, ‘best practice’ models should be documented and used.
International collaboration. With respect to best practice models, public health scientists and practitioners should also look across national borders to share information and learn from other countries. Research involving countries of origin can help to elucidate reasons for differences in risk between migrants and the majority population, which may be due to such factors as socioeconomic disadvantages, cultural background, or genetic polymorphisms.
Traumatized migrants. The vast majority of health problems experienced by migrants is of the same kind as those of the majority population and can be treated by existing health services. An exception is torture victims, whose condition is often underdiagnosed among refugees and asylum seekers. Most of them require treatment in specialized centers.
In summary, today’s decision makers and service providers worldwide are faced with the challenge ‘‘to plan and provide effective and accessible health services for communities with diverse languages, cultural backgrounds, migration circumstances and socio-economic status’’ (Grondin, 2004).
Conclusion
Migration will continue to increase, affecting literally all countries and populations worldwide. Given their minority status and the potential health disadvantages migrants are facing, public health and other sectors should be striving for policies to make migration a healthy and socially productive process. Intervention strategies should be conceptualized and developed within the framework of new public health – that is, they should not just consider migrants as a separate at-risk group, but address them in a systemic approach through which all population groups will benefit. The ultimate goal is the provision of adequate services to all persons, irrespective of their nationality or cultural background (diversity management). This requires changes not only in individual attitudes and in health systems, but also in immigration and integration policies. Yet, there is no room for ‘unreflected actionism’ – interventions should be based on evidence, or at least follow best practice models, and they should be systematically evaluated. Research on migrant health should be based on conceptual models, rather than be driven by the data available.
Bibliography:
- Ackerhans M (2003) Health issues of ethnic minority and migrant women: Coping with cultural barriers. Entre Nous 55: 9–11 Copenhagen, Denmark: WHO.
- Bach S (2003) International migration of health workers: Labour and social issues, WP 209. Geneva, Switzerland: International Labour Office (ILO). https://www.researchgate.net/profile/Stephen_Bach/publication/242394141_International_Migration_of_Health_Workers_Labour_and_Social_Issues/links/02e7e53201f6607745000000/International-Migration-of-Health-Workers-Labour-and-Social-Issues.pdf
- Balakrishnan TR and Maxim P (2005) Residential segregation and socioeconomic integration of visible minorities in Canada. IUSSP Conference. Tours, France, 23 July 23, 2005.
- Braunschweig S and Carballo M (2001) Health and Human Rights of Migrants. Geneva, Switzerland: International Centre for Migration and Health (ICMH).
- Carballo M, Grocutt M, and Hadzihasanovic A (1996) Women and migration: A public health issue. World Health Statistics Quarterly 49(2): 158–164.
- Carballo M and Nerukar A (2001) Migration, refugees, and health risks: Panel summary from the 2000 Emerging Infectious Diseases Conference in Atlanta, Georgia. Emerging Infectious Diseases 7(supplement 3): 556–560.
- Cookson S, Waldman R, Gushulak B, et al. (1998) Immigrant and refugee health. Emerging Infectious Diseases 4(3): 427–428.
- Diallo K (2004) Data on the migration of health-care workers: Sources, uses, and challenges. Bulletin of the World Health Organization 82(8): 601–607.
- Grondin D (2004) Editorial: Well-managed migrants’ health benefits all. Bulletin of the World Health Organization 82(8): 561.
- Gushulak BD and MacPherson DW (2004) Globalization of infectious diseases: The impact of migration. Clinical Infectious Diseases 38(12): 1742–1748.
- IOM (2004) Migration health report 2004. Geneva, Switzerland: International Organization for Migration (IOM). https://www.iom.int/health-and-migration-2004
- IOM (2005) World migration 2005. Costs and benefits of international migration. Geneva, Switzerland: International Organization for Migration (IOM). https://publications.iom.int/books/world-migration-report-2005-costs-and-benefits-international-migration
- Norredam M, Mygind A, and Krasnik A (2005) Access to health care for asylum seekers in the European Union – a comparative study of country policies. European Journal of Public Health 16(3): 285–289.
- Razum O and Geiger I (2003) Migranten. In: Schwartz FW, Badura B, Busse R, et al. (eds.) Das Public Health Buch – Gesundheit und Gesundheitswesen, pp. 686–692. Munich, Germany: Urban and Fischer Verlag.
- Razum O, Jahn A, Blettner M, and Reitmaier P (1999) Trends in maternal mortality ratio among women of German and non-German nationality in Germany, 1980 to 1996. International Journal of Epidemiology 28(5): 919–925.
- Razum O and Twardella D (2002) Time travel with Oliver Twist – towards an explanation for a paradoxically low mortality among recent immigrants. Tropical Medicine and International Health 7(1): 4–10.
- Razum O, Sahin-Hodoglugil N, and Polit K (2005) Health, wealth, or family ties? Why Turkish work migrants return from Germany. Journal of Ethnic and Migration Studies 31(4): 719–739.
- Robert Koch-Institut (2005a) Bericht zur epidemiologie der tuberkulose in Deutschland fu¨ r 2003. Berlin, Germany: Robert Koch-Institut (RKI).
- Robert Koch-Institut (2005b) Epidemiologisches bulletin, Sonderausgaben A und B/2005. Berlin, Germany: Robert Koch-Institut (RKI).
- Saravia NG and Miranda JF (2004) Plumbing the brain drain. Bulletin of the World Health Organization 82(8): 608–615.
- Steel Z and Silove DM (2001) The mental health implications of detaining asylum seekers. Medical Journal of Australia 175(11–12): 596–599.
- Stilwell B, Diallo K, Zurn P, Vujicic M, Adams O, and Dal Poz M (2004) Migration of health-care workers from developing countries: Strategic approaches to its management. Bulletin of the World Health Organization 82(8): 595–600.
- Tautz S, Ba¨ hr A, and Wo¨ lte S (2006) Kommerzielle sexuelle Ausbeutung von Kindern und Jugendlichen. In: Razum O, Zeeb H, and Laaser U (eds.) Globalisierung – Gerechtigkeit – Gesundheit. Einfu¨ hrung in International Public Health, pp. 245–258. Bern, Switzerland: Huber.
- UNFPA/IMP (2004) Meeting the challenges of migration: Progress since the ICPD. New York, Geneva, Switzerland: United Nations Fund for Population Activities/The International Migration Policy Programme (UNFPA/IMP). https://www.unfpa.org/publications/meeting-challenges-migration
- UN General Assembly (1999) Article 2, revised draft protocol to prevent, suppress and punish trafficking in persons, especially women and children, supplementing the United Nations convention against transnational organised crime. AC/254/4/Add.3/Rev.4. Geneva, Switzerland: UN General Assembly. https://www.ohchr.org/en/professionalinterest/pages/protocoltraffickinginpersons.aspx
- Valin N, Antoun F, Chouaid C, et al. (2005) Outbreak of tuberculosis in a migrants’ shelter, Paris, France, 2002. International Journal of Tuberculosis and Lung Diseases 9(5): 528–533.
- WHO (2003) International migration, health and human rights. Health and Human Rights Publication Series vol. 4. Geneva, Switzerland: World Health Organization (WHO). https://apps.who.int/iris/bitstream/handle/10665/42793/9241562536.pdf




