View sample elderly health research paper. Browse research paper examples for more inspiration. If you need a health research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
The elderly population is a population with more ‘at-risk’ members because of a variety of age-related changes that cause older people to have increased needs and decreased resources to meet those needs. Increased risk for this age group is related to health change, increasing need for care, and changing social circumstances. It is the interrelationship among these factors that particularly increases the risk for the elderly population.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
Health Change With Age: Increasing Risk
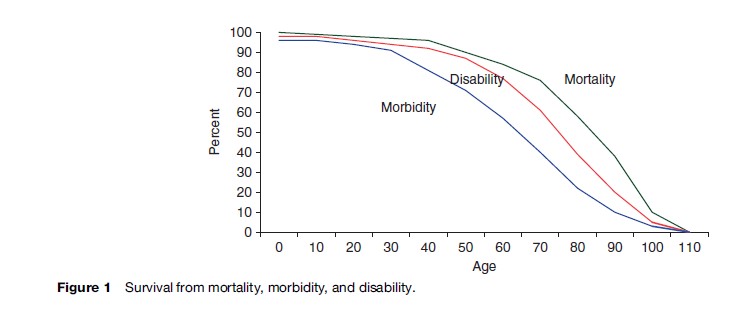
It is well known that mortality increases with age, with very high rates at the oldest ages. This age pattern of mortality reflects the underlying increase in health problems that occurs with advancing age that makes the elderly a particularly at-risk group. It is not the likelihood that death will occur, but the health deterioration that often precedes death that puts the elderly at risk. Most elderly persons die of chronic conditions such as cardiovascular disease and cancer that may evolve over many years or decades but become manifest in old age. As one ages, the likelihood increases that one will become disabled or lose physical or mental functioning abilities because of the increase in chronic diseases and conditions. Conditions particularly linked to aging include Alzheimer’s and Parkinson’s diseases and the loss of vision and hearing. Changes in cognitive ability and sensory losses that occur in older age are particular sources of disability. It is this increasing disease and disability that puts the elderly at risk. The process of health change for the older population proceeds from the onset of disease to disability to death. Figure 1 indicates the proportions of persons surviving to given ages without disease, disability, or mortality. As age increases, the proportion gets smaller. It is rare to find very old people without disease or disability, and this puts the older population at risk.
Geriatricians have characterized a syndrome common among the oldest-old as ‘frailty,’ which is the deterioration in health that results from the accumulation of diseases and the accompanying physiological dysregulation that often occurs in old age. It is recognized as a downward trajectory in health and ability to perform daily tasks and take care of oneself. Persons who have multiple health problems and increasing frailty are particularly at risk for a variety of poor outcomes, both because of their reduced physical capacity and their increased need for care. The elderly who are unable to provide their own care are the group most at risk.
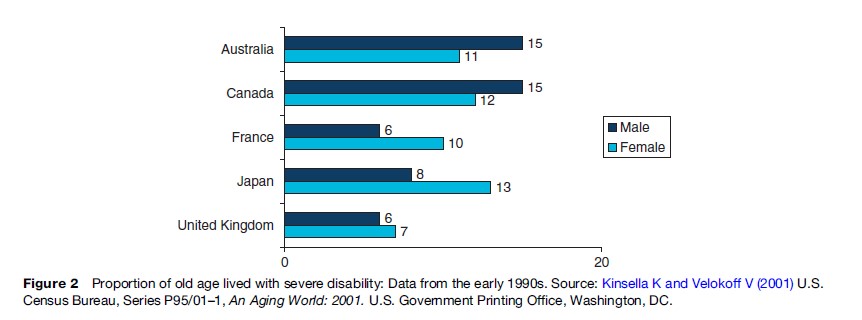
Because the elderly suffer not only from diseases but also from disabilities, the health care and services they need differ from those required at other ages. National policies for provision of care vary widely as to whether services for home care and independent living are included as well as for purely medical conditions. This interaction between health needs and health-care service provision is another source of risk for the elderly. Researchers have combined mortality and morbidity to provide estimates of how long older persons live with severe disability. The proportion of life lived in old age with severe disability is an indicator of how long older persons need care for disabilities (Figure 2). This varies by country and gender and with the age of the older population.
Appropriate Health Services: Demand And Availability
Health-Care Utilization
Health-care utilization is primarily determined by the need for service (i.e., levels of illness and disability), the availability of services, and the resources available for providing and paying for service. In countries with fewer freely available services, economic status plays a larger role in determining health-care utilization. Among older adults, the need for health services is greater and often the resources available are fewer. Many nations have programs in place to provide health services to elderly persons, although these vary dramatically in the generosity of coverage. Nations such as Thailand, Taiwan, and several European countries offer free medical care to older persons. Some countries offer restricted health services. For example, Singapore provides means-tested subsidies. Many developing nations do not offer health services to the elderly at all. One of the key differences between older and younger people is that older people may need custodial care because of high levels of disability. This type of care is often not included within the formal health-care system. The growing importance of severe disability with age and the lack of services for the disabled put older persons at risk.
Older people have higher per capita health-care needs for most types of health care than younger people. Increasing older populations worldwide mean that a growing population of elderly will require more acute and long-term care services. For many elderly people worldwide, health needs go unmet because either services are unavailable or unaffordable. For some older people, lack of transportation or accompanying persons are additional barriers to obtaining health services. Health infrastructures in most developing nations have been focused on maternal and child health and infectious disease. The rapid aging of the population and reductions in the role of infectious conditions suggest a need for a shift in this focus. Preventive care is an increasingly high priority in many countries because it is often very cost effective and offers better long-term health to citizens.
Overuse Or Inappropriate Use Of Medications
Research has documented the inappropriate use of medication in elderly persons in many settings, including hospitals, nursing facilities, and the home. Inappropriate use of medication is an additional source of risk for older people. Older adults differ physiologically from younger adults in several ways that impact the effects of drugs in the system, and these differences, coupled with older adults’ higher usage of medication, can put them at risk. Some medications can never safely be used in older adults, whereas others are recommended for use at lower doses, for a different duration, or with different frequency. Common examples of problematic medications are antihypertensive agents, psychoactive medications (including anxiolytics and benzodiazepines), hypoglycemic medications, anticholinergic drugs, and nonsteroidal anti-inflammatory drugs (NSAIDs). Poorer health status and the total number of medications prescribed most strongly increase the likelihood of receiving inappropriate prescriptions.
In many cases, problems occur as a result of interactions between multiple medications or because of redundant prescription of similar drugs by different physicians intended to treat the same problem. In health-care systems that offer fragmented treatment, specialists may be unaware of other medications a patient is taking or may be unaware of the contraindications of drugs used for conditions outside the doctor’s area of specialty. Whether resulting from a failure of patients to fully report their daily medication use or a failure of medical staff to fully record the information, the inappropriate use of medications can result in major safety concerns and is often preventable. Adverse drug interactions are a considerable cause of hospitalization and associated financial expenditures. Some researchers note the underutilization of pharmacists as drug therapy consultants to prevent this type of drug interaction from occurring.
Even when medication is appropriately prescribed, it is common to encounter problems with discrepancies between labeled dosage and dosage actually used, in the form of underuse or overuse. Research has also demonstrated that elderly persons more commonly retain expired medications in their homes and lack knowledge about identification and management of adverse drug reactions.
Institutionalization And Age-Related Services
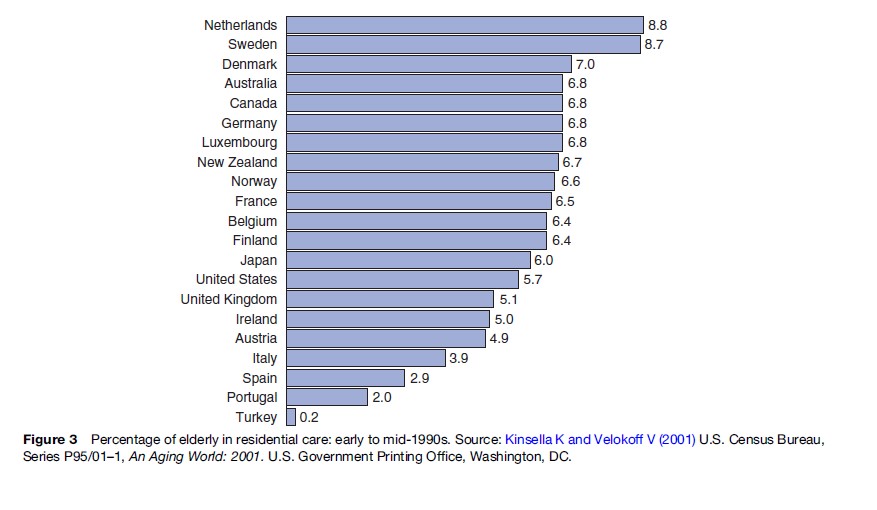
Though relatively rare in some countries, the risk of institutionalization and use of residential care is a significant concern for many elderly. Several factors influence the eventual use of residential care facilities, and this varies tremendously by country (Figure 3). Elderly people who have adult children are less likely to become institutionalized probably because of the alternative of co-residence. Although marriage often provides built-in support, married older adults are more likely to be institutionalized when an elderly spouse is no longer able to provide mutual care and support. Declines in functional and cognitive capacity are especially likely to predict institutionalization, although some losses in function can be improved by adaptive changes in living conditions. Increasingly, patients who are admitted to institutions which provide nursing care are more dependent because medical advances in developed nations allow individuals to remain in their homes longer before institutionalization becomes necessary. This has contributed to rising costs of nursing home care.
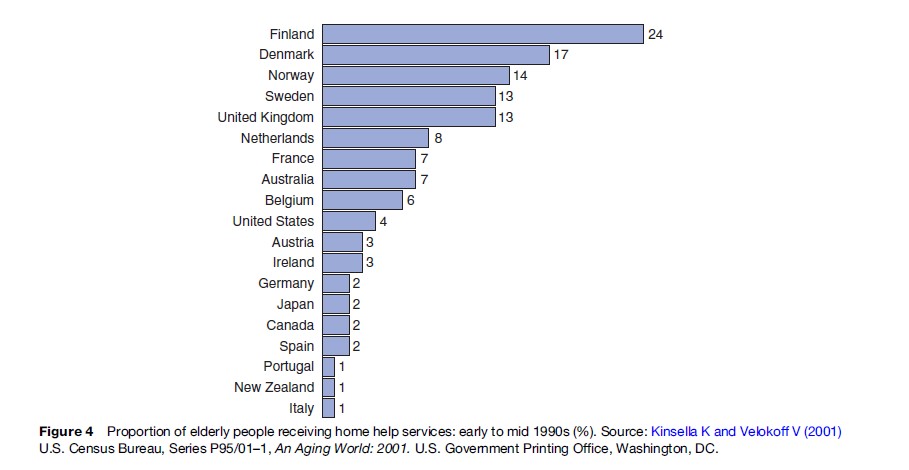
Many governments throughout the world have attempted to delay or reduce the rates of institutionalization by providing home help services. Scandinavian countries and the United Kingdom have generous public welfare systems and consequently have the highest prevalence of home help services (Figure 4). Unfortunately, many European countries, including Denmark and the Netherlands, have had to decrease spending on social services because of the increasing numbers of older adults in the population and the rising costs associated with providing public services.
Elderly: At Risk Due To Social Circumstances
Social Support
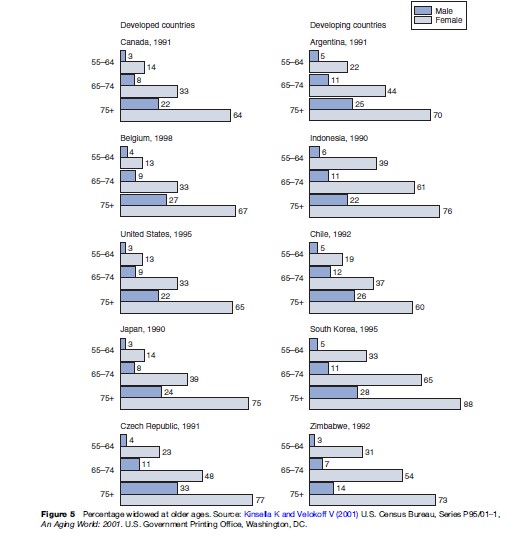
Elderly persons are also at risk due to social circumstances. Social networks may serve as a buffer against decline in health and well-being in old age. It is not only the health of an individual aging person that changes with age. There is also an increasing likelihood of sickness and mortality of family members and friends. This is another source of vulnerability among the elderly. Most women over age 74 in most countries of the world are widows, but most men of this age are married (Figure 5). The loss of a spouse and a dwindling social network of family and friends deplete this social buffer. The loss of social relationships also has an effect on physical and mental health, as well as mortality. Social support is a critical component of healthy aging. Social support includes resources, whether instrumental or emotional, provided by others. Emotional support is defined as interaction leading an individual to believe that he or she is cared for and loved, esteemed, and a member of a network of mutual obligations. Emotional support includes expressions of affection and trust. Instrumental support consists of tangible assistance such as help with household chores, financial assistance, transportation, and daily activities. Level of perceived support has been shown to be an important predictor of health and well-being, surpassing measures of actual support received. Individuals who feel supported recover more quickly from illness or surgery, follow medical regimens more closely, and are at lower risk of depression. Social support is defined not only by the number of relationships or the frequency of contact, but also by the quality of relationships.
As already discussed, elderly individuals who lack social ties are at greater risk for poor health. Social support promotes health in many ways; for example, by encouraging prompt attention to medical needs, by urging avoidance of unhealthy behaviors such as smoking, and by improving resistance to disease through reduction of stress response. The stress process is important in understanding how lack of social support affects health and well-being. Individuals who do not anticipate receiving help from a social network are more likely to experience prolonged neuroendocrine response to challenges, which may have harmful effects on health and immunity.
The type of social support that is effective in promoting health and well-being varies according to individual needs and situations. The degree to which older adults experience decreases in social support may vary across cultures, especially considering differing norms for family structure and co-residency that affect the number and quality of relationships, as well as the frequency of contact. The amount of social support needed may also depend on the degree to which resources are publicly provided. For example, in northern European nations, family may more commonly provide emotional support than instrumental support because of the very generous assistance the government provides for instrumental services. Cultures may also differ in the attitudes and beliefs that pertain to intergenerational support. In some cultures older adults may be reluctant to receive help from adult children, whereas in others it is expected. In many developing African countries the increasing proportion of persons with AIDS has led to a disruption in the social welfare for the elderly via the extended family. Urbanization and modernization of economies place strains on the traditional extended family system, especially when migration for work is necessary for economic security.
Economic Status
Economic resources can also serve as a buffer against some of the risks in old age. Those with few economic resources are at greater risk for most of the problems of old age because it is more difficult for them to secure their health and care needs. The degree of difficulty depends on the policies in each nation and the likelihood of elderly depending on familial support. Economic resources include assets and income, and in some countries children are major sources of economic support. In highly industrialized nations, economic support is usually supplied through retirement pensions, government programs, savings, investments, and assets. More agricultural nations rely more heavily on continued work and receipt of financial assistance from family members. For example, in Taiwan, Thailand, and the Philippines, earnings of adult children are the most important source of income for the elderly.
The adequacy of income and assets is relative. Less absolute income is required to survive where multigenerational living arrangements are common. In such cases the burden of home ownership is decreased and economies of scale reduce the cost of living for any one person. By contrast, in societies that increasingly value autonomy and privacy, elderly individuals must bear greater individual financial responsibility. Often governments define a poverty threshold below which persons cannot ‘reasonably’ survive. Poverty thresholds can be problematic as they are often arbitrary. In the United States, many elderly are often ‘near poor’ even though they may not meet the standards for poverty assistance because they do receive a government pension. Marital status, gender, education, health, and rural versus urban residence are important determinants of economic security in old age, as well as earlier in life. Those who are poor when they are young are often poor when they are old.
Living Arrangements
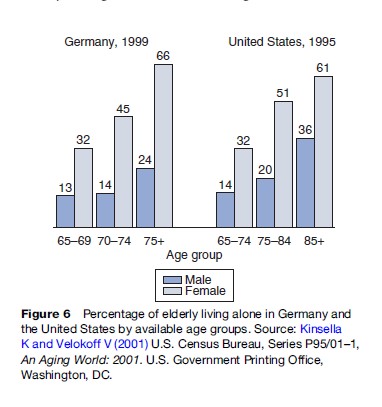
In developing countries around the world, it is the norm for the elderly to live with adult children. However, economic changes and Western values have pervaded many societies, resulting in the gradual replacement of extended family household structures by increasing expectations of independence and self-reliance by elders. In much of the world there is an increasing trend for older persons to live separately from their children. Changes in social and economic conditions are implicated as the cause of the trend. This can be a source of risk for older persons, especially those who are sick or disabled, widowed or poor. In countries such as Germany and the United States, most women over age 74 live alone (Figure 6).
There is wide variety in the global use of nonfamily institutions for care of the elderly. Although many societies offer some form of free or reduced-cost public housing for older adults, there has been rapid growth worldwide in the development of for-profit assisted living residences, retirement communities, nursing homes, and other old-age homes. Institutionalization is still relatively rare in most countries, but the number of institutionalized elderly throughout the world is rising.
Recent U.S. trends, however, show a declining prevalence of nursing home residence and increased return from nursing homes to community settings. Instead, more elders are adapting by recruiting paid and unpaid caregivers. Attempts to improve support and safety in one’s current home environment are generally preferred over transfer to institutional settings. Moves into assisted living or other independent residential facilities are also an increasingly prevalent alternative.
Lifelong Characteristics Of At-Risk Populations
Many of the characteristics that predict risk in old age are the same as for younger groups. The lifelong challenges of poverty, minority status, and gender continue to predict poor outcomes for older adults. Socioeconomic status (SES) is one of the most important determinants of health. The life trajectory is linked to one’s education and occupational status. Being of low SES predicts earlier onset and greater incidence of illness and earlier death. One mechanism is differential exposure to the risk factors for poor health. These include smoking and drinking, obesity, poor self-esteem, and financial stress. It has also been hypothesized that low social status and increased psychological pressures attached to low status may lead to changes in neuroendocrine pathways that later result in disease. Social inequalities are persistent, and increasing in some societies, and perpetuated by the global spread of market centered economic structures. The theory of cumulative advantage and disadvantage has often been applied to describe how one’s capacity, status, and access to resources accumulate to provide greater advantages or disadvantages over time, resulting in greater divergence among aging individuals.
Individuals with low socioeconomic status have earlier onset of health problems, greater morbidity, and earlier death. Lack of social support may partially explain the poorer health outcomes experienced by groups with lower SES. There may be differences in the amount of social support received by low SES groups and the importance of social support for determining health outcomes for these groups. Members of higher SES groups report more frequent contact with family and friends and greater satisfaction with the help they receive. Members of support networks tend to share similar socioeconomic status. In a low SES group, members of the network may lack the resources to provide assistance to their fellow network members. Furthermore, the types of problems experienced by low SES elders tend to be chronic and may result in burdens on support providers. In some countries, health disparities by race and ethnicity are intertwined with disparities due to SES, although SES differences in health are greater than race differences. High-income black males have a life expectancy that is 2.5 years longer than their low-income counterparts and have a life expectancy that is nearly 3 years longer than white males in the lowest income category. African-Americans experience earlier onset of chronic disease and live more years of life with disabling health problems.
Some research shows that the repeated experiences of discrimination and perceptions of discrimination result in physiological stress responses that lead to poor physical and mental health. Differential access to medical care and differential quality of care available may play a role in health disparities among members of different groups. Systematic differences in the kind and quality of medical care received have also been observed. Delayed diagnosis and poor management of chronic disease is common among minority groups. Although poor and minority elderly may have many disadvantages, membership of minority groups may also provide culturally reinforced social resources.
Gender and marital status are important predictors of late life health and well-being. These characteristics are highly related to being an at-risk elder. Women live longer than men and are therefore more likely to be widowed, develop chronic illness and cognitive impairment, and spend the last years of their lives in need of help for chronic health problems. Women are at greater risk of poverty in old age, especially in cultures in which women’s primary work is unpaid domestic labor or in which labor market norms prevent women from earning high wages. Because men more often die before their spouse, women are more likely to take up care-giving duties for their husbands, and for other family members, that take a toll on physical and psychological well-being.
Men are also adversely impacted by widowhood, as they are more likely to be dependent on domestic support provided by their wives and thus may be at a greater disadvantage when they have to live alone. This, however, may change as new generations of men and women divide domestic duties differently. Social isolation may also be more stressful for men, and they are typically less embedded into social networks over the life course.
Conclusion
Old age can put anyone at risk; almost everyone experiences changes in health and social networks that underlie much of this risk. People at greater risk include those without family and those without resources, as well as those who live in countries without social policies designed to address the special needs of aging populations.
Bibliography:
- Calasanti T (2004) Feminist gerontology and old men. Journal of Gerontology: Social Sciences 59B: S305–S314.
- Cohen B and Menken J (eds.) (2006) Aging in Sub-Saharan Africa: Recommendations for Further Research. Washington, D.C: National Academies Press.
- Crimmins EM and Seeman TE (2004) Integrating biology into the study of health disparities. Population Development Review 30: 89–107.
- Crown W (2001) Economic status of the elderly. In: Binstock RH and George LK (eds.) Handbook of Aging and the Social Sciences,, 5th edn., pp. 352–368. San Diego, CA: Academic Press.
- Dannefer D (2003) Cumulative advantage/disadvantage and the life course: Cross-fertilizing age and social science theory. Journals of Gerontology: Social Sciences 58: S327–S337.
- Golden AG, Preston RA, Barnett SD, Llorente M, Hamdan K, and Silverman MA (1999) Inappropriate medication prescribing in homebound older adults. Journal of the American Geriatrics Society 47: 948–953.
- Hays JC, Pieper CF, and Purser JL (2003) Competing risk of household expansion or institutionalization in late life. Journals of Gerontology 58B: S11–S20.
- Hermalin AI (ed.) The Well-Being of the Elderly in Asia: A Four-Country Comparative Study. Ann Arbor, MI: The University of Michigan Press.
- Johnson ML (2005) The Cambridge Handbook of Aging. Cambridge, UK: Cambridge University Press.
- Kinsella K and Velokoff V (2001) U.S. Census Bureau, Series P95/01–1, An Aging World: 2001. Washington, DC: U.S. Government Printing Office.
- Krause N (2001) Social support. In: Binstock RH and George LK (eds.) Handbook of Aging and the Social Sciences, 5th edn., pp. 273–294. San Diego, CA: Academic Press.
- Liebig PS (2003) In: Liebig PS and Rajan SI (eds.) An Aging India: Perspectives, Prospects, and Policies. New York: Haworth Press.
- Moen P (2001) The gendered life course. In: Binstock RH and George LK (eds.) Handbook of Aging and the Social Sciences,, 5th edn., pp. 179–196. San Diego, CA: Academic Press.
- National Center for Health Statistics (2001) Health, United States, 2001, Special Excerpt: Trend Tables on 65 and Older Population. Hyattsville, MD: Centers for Disease Control and Prevention.
- O’Rand AM (2001) Stratification and the life course: The forms of life-course capital and their interrelationships. In: Binstock RH and George LK (eds.) Handbook of Aging and the Social Sciences,, 5th edn., pp. 197–213. San Diego, CA: Academic Press.
- Robine JM, Jagger CJ, Mathers CD, Crimmins EM, and Suzman RM (2003) Determining Health Expectancies. Chichester, UK: John Wiley and Sons.
- Robine JM, Crimmins EM, Horiuchi S, and Zeng L (eds.) (2006) Human Longevity, Individual Life Duration, and the Growth of the Oldest-old Population. Dordrecht, Netherlands: Springer.
- Rowe J and Kahn R (1999) Successful Aging. New York: Random House.
- Waite LJ (ed.) (2004) Aging, Health and Public Policy: Demographic and Economic Perspectives. A supplement to Vol. 30 of Population and Development Review. New York: Population Council.
- Williams DR and Wilson CM (2001) Race, ethnicity, and aging. In: Binstock RH and George LK (eds.) Handbook of Aging and the Social Sciences,, 5th edn., pp. 160–178. San Diego, CA: Academic Press.
- Zeng Y, Crimmins E, Carriere Y, and Robine JM (eds.) (2006) Longer Life and Healthy Aging. Dordrecht, the Netherlands: Springer.
- Zhan C, Sangl J, Bierman AS, et al. (2001) Potentially inappropriate medication use in the community-dwelling elderly: Findings from the 1996 medical expenditure panel survey. Journal of the American Medical Association 286: 2823–2829.




