Sample Ethnicity, Race, And Health Research Paper. Browse other research paper examples and check the list of research paper topics for more inspiration. If you need a research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our custom research paper writing service for professional assistance. We offer high-quality assignments for reasonable rates.
This research paper provides an overview of the role of race and ethnicity in health. Racial and ethnic statuses are primarily social categories that can reflect differential exposure to health-related risks or resources. Accordingly, across a broad range of societies, disadvantaged racial and ethnic populations have elevated rates of disease and death. Racial disparities in health are persistent over time. Data suggest that racial differences in health largely reflect racial variations in socioeconomic circumstances, but individual and institutional discrimination often play an incremental role. Understanding racial and ethnic variations in health requires greater attention to data quality issues and to assessment of both the resources and vulnerabilities to which population groups are exposed.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
1. What Is Race And Ethnic Status?
Historically, race has been viewed as capturing biological variation within human populations. However, the concept of race never rested on a firm, scientific foundation. Racial taxonomies pre-dated modern scientific theories of genetics and carefully executed genetic studies. Thus, race emerged as a sociopolitical construct, useful not only to classify phenotypic variation but also to justify the exploitation of groups defined as inferior. Historically, the conceptualization of race has been influenced by cultural and political considerations, and race has served important ideological functions in society (Duster 1984). For example, medical research in the nineteenth century attempted to document that blacks were biologically inferior to whites and therefore more susceptible to a broad range of diseases (Krieger 1987). Importantly, such data provided a scientific justification for slavery and economic exploitation.
Understanding and addressing the role of race and ethnicity in health requires a clear understanding of what race is, and the identification of the specific risk factors and resources linked to racial and ethnic status that may be responsible for variations in health. A growing body of evidence indicates that the traditional conceptualization of race is flawed. Scientific data reveal that 95 percent of human genetic variation exists within racial groups (Lewontin 1982). That is, there is more genetic variation within races than between them and, although there are patterns to the distribution of genetic characteristics, our racial categories do not capture biological distinctiveness. Our current racial categories are more alike than different in terms of biological characteristics and genetics, and there are no specific, scientific criteria to classify the human population unambiguously into discrete biological categories with rigid boundaries (Lewontin 1982). Racial taxonomies are arbitrary, and race is more of a social category than a biological one.
Although ethnic groups can share a range of phenotypic characteristics due to their shared ancestry, the term ‘ethnicity’ is typically used to highlight cultural and social characteristics instead of biological ones. Ethnic groups share some combination of common geographic origins, family patterns, language, common values, cultural norms, religious traditions, literature, music, dietary preferences, and employment patterns. Thus, the current ‘racial’ categories really capture ethnic variation; that is, they reflect common ancestry, history, or culture. Some have suggested that the term ethnicity should replace ‘race’ in health research, and the term race should be abandoned (Cooper 1994). However, although not useful as a biological category, race is an important social category. It is what sociologists call a master status—a central determinant of social identity and obligations, as well as of access to societal rewards and resources. Given that racial categories have reflected racism and its consequences (oppression, exploitation, and inequality) historically, collecting the appropriate data on race can facilitate ongoing monitoring of the magnitude of differentials and enhance understanding of their causes and the development of effective interventions to address them.
Relatedly, although variations in health are evident for many ethnic groups, much of the marked variation is evident for minority racial and ethnic groups. The term minority is used, not to represent the numerical size of a population, but rather to reflect the stratification and access to power and resources of that group. The current minority groups in the United States, for example, reflect the intersection of racial and ethnic status combined with economic disadvantage. Only those population groups that experienced prejudice and discrimination historically and have been unsuccessful in assimilating are minority groups.
2. Racial And Ethnic Variations In Health
Across a broad range of societies, racial and ethnic statuses predict variation in health. The United States has routinely reported health statistics by race, and the role of race and ethnic status is readily evident in US data. National mortality data reveal that African Americans (or blacks) have death rates that are higher than whites for 13 of the 15 leading causes of death in the United States (NCHS 1991). The differences in death rates are small for some conditions, such as atherosclerosis, but at least twice as high for deaths from diabetes, kidney disease, homicide, septicemia, prenatal conditions, and HIV/AIDS. These pervasive disparities across such a broad range of health conditions are striking. In US data, Hispanics and American Indians have lower mortality rates than whites for cardiovascular disease and cancer, but higher rates for some causes of death, such as diabetes and cirrhosis of the liver. In contrast, the Asian American population has mortality rates that are lower than those of whites.
Until recently, the United Kingdom did not focus on racial/ethnic variations in health. However, analyses of death rates by country of birth suggest that there may be important racial/ethnic variations in health status in England (Balarajan and Raleigh 1995). These patterns are complex and vary by both the specific ethnic group and health outcome under consideration. For example, death rates from coronary heart disease and stroke are higher than the national average for persons from the Indian subcontinent and the African commonwealth. In contrast, Caribbean immigrants have mortality rates lower than the national average for coronary heart disease but higher for hypertension and stroke. Similarly, persons from the Indian subcontinent and the Caribbean have higher-than-average mortality for cancers of the liver, gall bladder, and cervix. Death rates from breast and lung cancer are lower in these three major immigrant groups, but Asians have high rates for oral cancer, and Caribbeans have high mortality rates from prostate cancer.
The experience of the United States and England is not unique. In a comprehensive review of racial and ethnic differences in disease internationally, Polednak (1989) reveals that racial and ethnic status predicts variations in health across a broad range of societies. Disadvantaged racial ethnic groups, such as the Maori in New Zealand, blacks in South Africa, and Aboriginal populations in Australia, have higher rates of disease than the more advantaged groups within their societies. For example, for the 1991–6 period in South Africa, compared to the survival experience of white infants, the infant mortality rate was 5.2 times higher for blacks, 4.2 times higher for Coloureds and 1.3 times higher for Asians (Sidiropoulos et al. 1997). Recent Australian data reveal that the rate of low birth weight infants for indigenous mothers is twice that of their nonindigenous peers, and the neonatal mortality rate (deaths of liveborn infants within 28 days of birth) is 2.6 times higher for babies born to Aboriginal mothers compared to the rest of the population (McLennan and Madden 1999). These elevated mortality rates persist throughout the life course, with Aboriginal males and females having a mortality rate between ages 35 and 44 that is at least seven times higher than that of the nonindigenous population. Moreover, there is considerable variation by ethnic status in multiple societies, with some ethnic groups having higher frequencies of some disease conditions but lower frequencies of others (Polednak 1989). For example, among European groups, the French tend to have low rates of heart disease, the Poles low rates of stroke, and the Finns low rates of breast and colorectal cancer.
2.1 Persisting Racial Disparities In Health
One important feature of racial differences in health is the persistence of the racial gap in health status over time. For example, despite declining death rates from stroke in England between 1970 and 1983, there was the persistence of elevated rates of stroke deaths for persons from the Caribbean and Africa (Balarajan and Raleigh 1995). Table 1 shows that, in 1950, blacks in the United States had an overall death rate that was 1.6 times higher than that of whites. Mortality rates have declined for both racial groups over time, but in the late 1990s, blacks had a death rate that was still 1.6 times that of whites (NCHS 1999). For several causes of death (heart disease, cancer, cirrhosis of the liver, and diabetes), the black white ratio was wider in the late 1990s than in 1950. There were multiple paths to this pattern of persistent racial differentials (Williams 1999). For some outcomes, such as heart disease, declining rates are evident for both racial groups, but the black white difference widened due to more rapid improvements in the health of the white population than of the black population. For cancer and diabetes, there were stable or declining rates for whites, but increasing rates for blacks. For other outcomes, such as stroke and unintentional injury, the black white gap was virtually identical in the late 1990s to what it was in 1950. However, influenza and pneumonia stand out as the only causes of death where the black /white difference in mortality has narrowed over time due to more rapid improvements in the health of the black compared to the white population. We need an enhanced understanding of the reasons for this success so that we could develop interventions to replicate it.
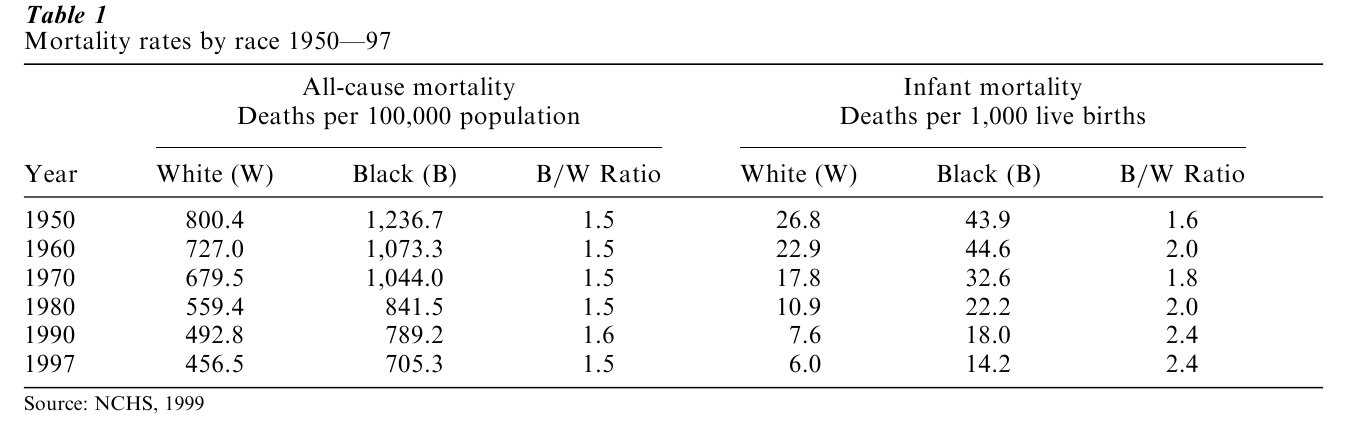
Infant mortality data tell a similar story. The right panel of Table 1 indicates that, compared to the 1950 infant death rate, the 1997 infant mortality rate was three times lower for blacks and more than four times lower for whites (NCHS 1999). However, the relative difference in rates between the two racial groups was larger in 1997 than in 1950. A black infant was 1.6 times more likely than a white infant to die before his or her first birthday in 1950. This ratio increased to 2.4 in 1997.
3. Economic Status: A Central Determinant Of Health
Although racial and ethnic status do not tell us much about underlying biological risks for disease, they do reflect an important part of the economic inequality and historic injustice that has existed in particular societies. Racial differences in economic circumstances are central to understanding health status variations.
3.1 Racial Differences In Socioeconomic Status
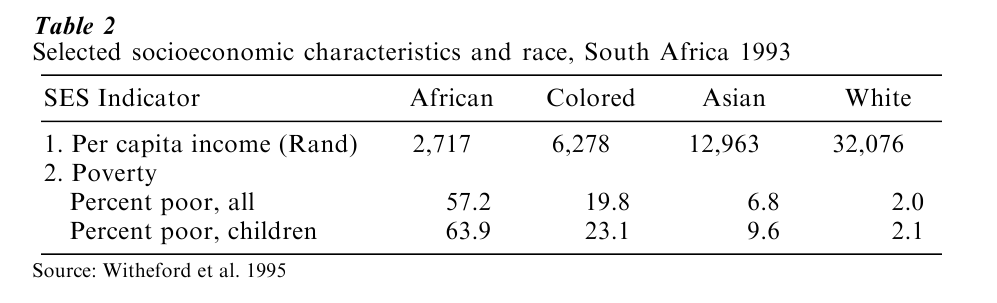
There are important differences in power and socioeconomic status (SES) across major racial and ethnic groups. Table 2 presents levels of per capita income and poverty rates by race in South Africa from a World Bank-funded national survey on Living Standards and Development conducted in 1993. Racial disparities in economic circumstances are striking. Whites in South Africa have a per capita income (R 32,076) that is almost 12 times that of blacks, five times that of Coloureds, and two and a half times that of Asians (Whiteford et al. 1995). In a similar vein, compared to the poverty rate of whites of 2 percent, the rate of poverty is 29 times higher for blacks, 10 times higher for Coloureds, and more than three times higher for Asians. For all racial groups, the poverty rate is higher for children than for the total population.
In the United States, blacks, Hispanics, and American Indians have lower rates of income, education, and occupational status than whites. The Asian population in the United States is overrepresented at both ends of the SES distribution. Compared to whites, Asians have higher levels of median income, but some subgroups of the Asian population, such as the Hmong, Laotians, and Cambodians, have lower levels of income and higher rates of poverty than the black or the American Indian population. This highlights the heterogeneity that exists within many of the major racial and ethnic categories, and the importance of attending to the variation within these subgroups. For multiple health outcomes and multiple racial ethnic groups, an overall statistic masks the variation that exists for subgroups within that population.
Data for the US also reveal that racial differences in income understate the true magnitude of racial differences in economic circumstances. Income captures the flow of economic resources into the household. Wealth reflects the accumulated economic reserves that can cushion a decline in income and facilitate long-term planning. Racial differences in wealth are considerably larger than those for income. For example, in the United States, the median net worth of whites ($44, 408) is almost ten times larger than that of blacks, and eight times larger than that of Hispanics. Moreover, measures of wealth make an incremental contribution in predicting variations in health over and above measures of education and income (Williams and Collins 1995).
3.2 Race, SES, And Health
Research reveals that SES differences between the races account for much of the racial/ethnic differences in health. For example, adjusting black/white disparities in health in the USA for SES sometimes eliminates, but always substantially reduces, these differences. Table 3 illustrates these patterns. It presents US life expectancy at age 45 by family income for black and white males and females. At age 45, white males have a life expectancy that is almost five years longer than their black counterparts; and white females outlive their black counterparts by 3.7 years. Several important trends are noteworthy. First, for both racial groups, income is strongly linked to life expectancy. Consistently, persons of lower levels of income have lower life expectancy than their more economically favored peers. Second, the effect of SES on health is not confined to the low end of the income distribution. Persons of each higher level of income experience better health than those at the level immediately preceding theirs, at least up to the highest category used here (which is about the median).
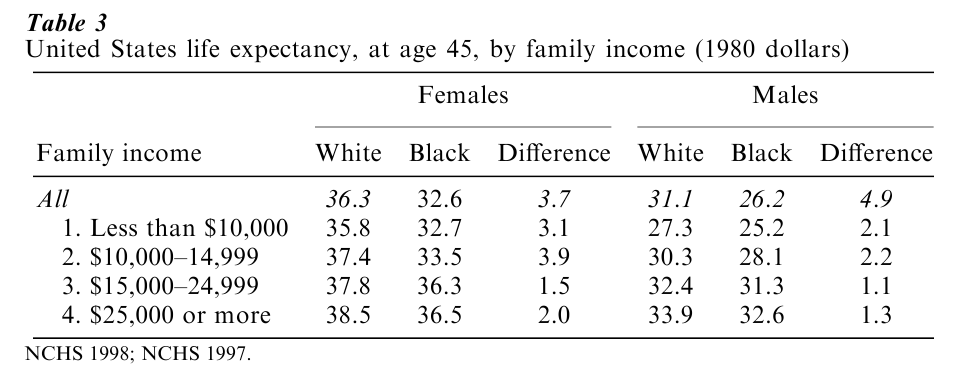
Third, the difference in health status by SES for both black and white men is larger than the overall racial difference. African American men in the highest income group live 7.4 years longer than those in the lowest income group; the comparable number for whites is 6.6 years. The overall racial difference for men was 4.9 years. Although SES predicts variation in health for both black and white women, for women, the overall racial difference is somewhat larger than the differences between SES groups. The life expectancy data also reveal an independent effect of race, even when blacks and whites are comparable in income. At every level of income for both men and women, African Americans have lower levels of life expectancy than their white peers. This pattern has been observed across multiple health outcomes, and for some indicators of health, such as infant mortality, the racial gap becomes larger as SES increases.
3.3 Racism: An Added Burden For Non-Dominant Populations
There are several factors linked to historical or contemporary racism that can account for these differences. Racism refers to organized institutional structures and policies, built on an ideology of superiority that allocates systematically fewer societal resources to groups regarded as inferior. Racial residential segregation in the United States and South Africa has been a prime example of a societal structure that importantly restricted socioeconomic opportunity and mobility for groups regarded as inferior (Cell 1982, Jaynes and Williams 1989). Residential segregation determined housing conditions, education and employment opportunities, and thus truncated economic mobility. Because of conditions created by residential segregation, SES indicators are not equivalent across race. There are racial differences in educational quality in elementary and high schools. Similarly, the income return for a given level of education varies by race. For example, data from the United States reveal that, at every level of education, blacks and Hispanics, working full time in the labor force, have lower levels of income than whites (Williams and Collins 1995).
We noted earlier that there were large racial differences in wealth. These racial differences in wealth are evident at all levels of income, and are largest at the lowest income level (Williams and Collins 1995). For example, persons in the lowest quintile of income in the United States, the net worth of whites is $10,257 compared to $1 for blacks and $645 for Hispanics. For most US households, housing equity is a major source of wealth. Thus, contemporary racial differences in wealth reflect the institutional discrimination that was embodied in government housing policy and the practices of banks and the real estate industry a generation ago (Jaynes and Williams 1989). There are also large differences in purchasing power across race. For example, on average, African Americans pay higher prices for a broad range of goods and services (such as groceries, housing, and insurance) because of the higher costs in the residential contexts in which they reside. Residential segregation has also led to the concentration of poverty and the non-equivalence of neighborhood environments across race. Compared to whites of equivalent income, blacks in the USA live in communities lower in SES and resources, such that, in the 171 largest cities in the USA, the worst urban residential context for whites is better than the average context of black communities (Sampson and Wilson 1995).
Second, the health status of adults is influenced not only by current SES but also by exposure to adverse economic conditions over the life course. Non-dominant racial groups are more likely than their economically favored counterparts to have experienced economic deprivation, elevated rates of illness, and deficits in medical care during infancy and childhood. Some research suggests that the health status of adults may be affected adversely due to childhood diseases and living conditions, as well as to nutritional deprivation in the intrauterine environment or during infancy and childhood (Elo and Preston 1992). Thus, the persistence of racial differences in adult health, even in the face of adjustment for SES, could reflect, at least in part, racial differences in early-life economic and health adversity.
Third, racial discrimination and prejudice may constitute added risk factors that adversely affect health. There is evidence of systematic discrimination in the quantity and quality of services across racial groups, including medical care (Williams 1999). Studies in the United States reveal that, even after adjustment for SES, health insurance, and clinical status, whites are more likely than blacks to receive a broad range of specific medical procedures. These disparities exist even in contexts where differences in economic status and insurance coverage are minimized, such as the Veteran’s Administration Health System and the Medicare program.
Research also suggests that subjective experiences of unfair treatment may be an important type of stress that can affect health adversely. Several studies reveal that experiences of discrimination are related adversely to physical and mental health (Krieger 1999, Williams and Williams-Morris 2000). Some recent data suggest that exposure to experiences of discrimination makes an incremental contribution to explain racial differences in self-reported measures of health over and above SES (Williams 1999). Other data indicate that a widely held societal stigma of inferiority can create specific anxieties, expectations, and reactions that can adversely impact socioeconomic performance as well as mental health status (Williams and Williams-Morris 2000, Steele 1997). First, across multiple societies, groups viewed as inferior have lower educational performance. Second, members of negatively stereotyped groups may internalize societal stereotypes such that the stereotype becomes a self-fulfilling prophecy leading to poor performance. Alternatively, the threat of poor performance can lead to anxieties that affect academic performance adversely. Third, some limited research suggests that African Americans who endorse negative cultural images of their group tend to have higher levels of depressive symptoms and substance use.
3.4 Changes In Racial Inequalities In Health
Data from the United States suggest that patterns of racial inequality change over time in response to larger socioeconomic changes. For example, although it was noted earlier that the black white gap in overall mortality was identical in the late 1990s to what it was in 1950, over this time period there were times of both widening and reduced racial differentials in health. For example, the Civil Rights Movement improved the economic circumstances of blacks and narrowed the black white gap in income during the 1960s and early 1970s. Correspondingly, mortality rates for blacks declined, both on a percentage and an absolute basis, more rapidly than those of whites between 1968 and 1978 (Williams and Collins 1995). Similarly, during this time period, the life expectancy increases for black males and females were larger on both a relative and an absolute basis than those for whites. However, the economic status of blacks relative to whites stagnated in the mid-1970s and worsened during the 1980s. Similarly, the black white gap in health worsened for multiple indicators of health status during this decade. The black white gap in life expectancy, infant mortality, and excess deaths in-creased between 1980 and 1991 (Williams and Collins 1995). For example, for five consecutive years after 1984, the life expectancy at birth for blacks progressively declined from 1984 levels, while that of whites continued to increase progressively. These data are consistent with research, which shows that the health of populations is affected by a broad range of economic factors, including growth, stability, and inequality (Brenner 1995). For example, mortality from all causes tends to increase about two to three years after the low point of a recession. These data highlight that both race and SES have powerful influences on health because, as master statuses, they shape the experience of and exposure to almost all psychosocial and environmental risk factors for health.
4. Data Quality
Race is routinely used in both the health policy and the research literature in a routine, atheoretical, and uncritical manner, with little attention given to the measurement difficulties that are attendant on the assessment of racial categories. However, there is growing attention to reliability and validity problems linked to the assessment of race that have implications for the quality of available data on racial differences in health (Hahn 1992, Williams and Collins 1995).
4.1 Problems With The Numerator
In the United States, it is well documented that the numerators for officially reported death rates and some other health events are underreported due to the discrepancy between interviewer-observed race and respondent-reported race. This problem is minimal for data on blacks and whites, but substantial for American Indians, Asians, and Hispanics. Persons who self-identify with these groups are often misreported as white on death certificates and in other health statistics contexts. This numerator problem leads to an underestimation of health events for these racial ethnic groups.
4.2 Problems With The Denominator
Another problem affecting the quality of racial data is the accuracy of the denominators used in calculating rates of health events. In many countries, data collected by the official census are used as the basis for denominators. In the United States, Census Bureau evaluations of the extent of the undercount based on administrative data and demographic trends reveal that, while the overall undercount for the United States population is small, it is considerably larger for blacks than for whites, and is especially large for middle-aged black males. Importantly, the use of a denominator that is undercounted inflates the obtained rate in exact proportion to the undercount in the denominator. Thus, most officially reported mortality and morbidity rates for middle-aged black males are about 15 percent too high. Currently, demographic analysis estimates of Census undercount are available only at the national level, and it is likely that the omission of black males from households (the major cause of the undercount of blacks) varies by geographic area and could thus be considerably larger for some states or municipalities.
4.3 The Challenge Of Defining Race And Ethnicity
Data from the US also suggest that there is considerable inconsistency in reporting racial, and especially ethnic, status over time. Given that many persons are multiracial or multiethnic in ancestry, self-identity appears to be importantly linked to the particular context of measurement. Relatedly, there is considerable debate over the optimal terminology to be used for particular racial groups, the number of racial groups for which data should be collected, the boundaries between racial and ethnic status, and whether new categories should be developed for persons who are of mixed ancestry. For a growing number of persons in society, racial and ethnic status is not singular and static, but multiple and dynamic (Evinger 1995).
Complicating the definitional problems linked to race is the fact that categories of race and ethnicity are often assessed differently across societies, over time within particular societies, and by different agencies and institutions even within the same society. In the USA, for example, the standard birth and death certificates were revised in 1989 to include identifiers for Hispanic status. But the wording of the question assessing Hispanic status varies from state to state, and the data on Hispanic ethnicity is not completely reported in all states. Similarly, many health surveys and federal data-collection systems in the USA use one question to assess race and a separate one to assess Hispanic origin, while other agencies use one combined question to assess both racial and ethnic status. Importantly, differing wording of racial and ethnic questions will provide varying estimates of the size of racial ethnic populations.
5. Resources And Acculturation
Health-enhancing resources exist even in the most disadvantaged racial and ethnic populations. Much research on the health of the disadvantaged has focused historically on pathology and vulnerability. However, the available health data clearly suggest that health-enhancing factors are also resident within contexts of economic deprivation. For example, despite high rates of poverty and low rates of health insurance coverage, Mexican immigrants still have a relatively good health profile. Similarly, although African Americans are disadvantaged on almost every indicator of physical health status compared to whites, they have surprisingly good levels of mental health (Williams and Williams-Morris 2000). Rates of suicide are markedly lower for blacks than whites, and blacks tend to have equivalent or lower rates of psychiatric illness compared to whites. These data suggest the need to identify cultural strengths and health enhancing resources that exist within disadvantaged communities, and that may shield these populations from at least some of the negative exposures in their social context. Research has nominated the quality of family and extended kin relationships, as well as the role of religious institutions and participation, as key health-enhancing resources that may reduce some of the negative effects of stress on the health of disadvantaged populations. More research is needed on the mechanisms and processes by which these factors operate, and the ways in which they combine with existing risk factors to affect health.
In many societies, many minority racial and ethnic groups are immigrant populations. The health profiles of these groups may reflect their immigrant status importantly and may change with increasing length of stay in the host society. In the United States, immigrants of all the major racial ethnic groups have lower rates of infant and adult mortality than their native-born counterparts (Williams 1999). Importantly, these patterns persist even when immigrant groups, such as Mexicans in the United States, are lower in SES and have limited access to medical care. At the same time, other data suggest that, across a broad range of health status indicators such as infant mortality, low birth rate, cancer, high blood pressure, adolescent pregnancy, and psychiatric disorders, the health status of immigrants worsen with length of stay in the USA (Williams and Collins 1995). The mechanisms and processes responsible for these negative effects of acculturation are not fully understood. Several behaviors that adversely affect health status appear to increase with length of stay. It has also been suggested that there may be health-protective aspects of indigenous cultures and belief systems that are lost with increasing time in a new society.
Culture is a construct that is widely invoked in discussions of racial and ethnic variations in health. However, it is often treated as a residual explanation for unexplained differences in health. There is a critical need for the theoretical identification and the empirical assessment of the specific cultural beliefs and behaviors that are presumed to affect health. Moreover, researchers must avoid labeling as cultural what are more structural differences in the social position of different groups. Culture is dynamic and its development and persistence must be understood within the context of powerful reciprocal influences that are operative as social groups interact with the constraints and opportunities of their specific environment.
6. Concluding Recommendations
Future research on racial ethnic variations in health must assess comprehensively racial and ethnic status. This should include the assessment of the considerable ethnic heterogeneity that exists within all of the widely used racial categories. Second, researchers must recognize that there is no generic health model that applies equally to all racial or ethnic minority populations. Research and health policy regarding race should be attentive to the distinctiveness of each racial group, including using the terms that are broadly recognized and preferred by a substantial proportion of respondents of particular racial groups. The fluidity of racial and ethnic categories requires periodic monitoring and updating measures of racial and ethnic status. Importantly, whenever racial and ethnic data are reported, more attention must be given to the interpretation of these data. For example, it is always necessary to indicate why race or ethnicity is being utilized, the limitations of racial and ethnic data, and how the findings should be interpreted. Given the strong association between racial ethnic status and SES, the presentation of data on racial differences should routinely stratify them for SES within racial groups. Failure to attend to these issues of presentation and interpretation may misspecify complex health risks and even perpetuate negative racial stereotypes. Finally, future research must conceptualize and operationalize increasingly the specific factors linked to race that might affect health.
Bibliography:
- Balarajan R, Raleigh V S 1995 Ethnicity and Health in England. Department of Health, London
- Brenner M H 1995 Political economy and health. In: Amick B C III, Levine S, Tarlov A R, Walsh D (eds.) Society and Health. Oxford University Press, New York, pp. 211–46
- Cell J 1982 The Highest Stage of White Supremacy: The Origin of Segregation in South Africa and the American South. Cambridge University Press, New York
- Cooper R S 1994 A case study in the use of race and ethnicity in public health surveillance. Public Health Reports 109(1): 46–52
- Duster T 1984 A social frame for biological knowledge. In: Duster T, Garret K (eds.) Cultural Perspectives on Biological Knowledge. Ablex Publishing, Norwood, NJ, pp. 1–40
- Elo I T, Preston S H 1992 Effects of early-life conditions on adult mortality: A review. Population Index 58: 186–212
- Evinger S 1995 How shall we measure our nation’s diversity? Chance 8(1): 7–14
- Hahn R A 1992 The state of federal health statistics on racial and ethnic groups. Journal of the American Medical Association 267(2): 268–71
- Jaynes G D, Williams R M 1989 A Common Destiny: Blacks and American Society. National Academy Press, Washington, DC
- Krieger N 1987 Shades of difference: Theoretical underpinnings of the medical controversy on black white differences in the United States, 1830–1870. International Journal of Health Services 17: 259–78
- Krieger N 1999 Embodying inequality: A review of concepts, measures, and methods for studying health consequences of discrimination. International Journal of Health Services 29(2): 295–352
- Lewontin R C 1982 Human Diversity. Scientific American Books, New York
- McLennan W, Madden R 1999 The Health and Welfare of Australia’s Aboriginal and Torres Strait Islander Peoples. Australian Bureau of Statistics, Commonwealth of Australia NCHS (National Center for Health Statistics) 1991 Vital Statistics of the United States, 1988. Vol 2. Mortality, Part A. Public Health Services, Washington, DC
- NCHS (National Center for Health Statistics) 1997 US Decennial life tables for 1989–91. United States Life Tables 1(1): 12–29
- NCHS (National Center for Health Statistics) 1998 Health, United States, 1998 With Socioeconomic Status and Health Chartbook. US Department of Health and Human Services Hyattsville, MD
- NCHS (National Center for Health Statistics) 1999 Health, United States, 1999 With Health and Aging Chartbook. US Government Printing Office, Hyattsville, MD
- Polednak A P 1989 Racial and Ethnic Differences in Disease. Oxford University Press, New York
- Sampson R J, Wilson W J 1995 Toward a theory of race, crime, and urban inequality. In: Hagan J, Peterson R D (eds.) Crime and Inequality. Stanford University Press, Stanford, CA, pp. 37–54
- Sidiropoulos E, Jeffery A, Mackay S, Forgey H, Chipps C, Corrigan T 1997 South Africa Survey 1996 97. South African Institute of Race Relations, Johannesburg, South Africa
- Steele C M 1997 A threat in the air: How stereotypes shape intellectual identity and performance. American Psychologist 52(6): 613–29
- Whiteford A, Posel D, Kelatwang T 1995 A Profile of Poverty, Inequality and Human Development. Human Sciences Research Council, Pretoria, South Africa
- Williams D R 1999 Race, SES, and health: The added effects of racism and discrimination. Annals of the New York Academy of Sciences 896: 173–88
- Williams D R, Collins C 1995 US socioeconomic and racial differences in health. Annual Review of Sociology 21: 349–86
- Williams D R, Williams-Morris R 2000 Racism and mental health: The African American experience. Ethnicity and Health 5: 243–68




