Sample Doctor-Patient Interaction Research Paper. Browse other research paper examples and check the list of research paper topics for more inspiration. iResearchNet offers academic assignment help for students all over the world: writing from scratch, editing, proofreading, problem solving, from essays to dissertations, from humanities to STEM. We offer full confidentiality, safe payment, originality, and money-back guarantee. Secure your academic success with our risk-free services.
1. Introduction
The quality of the interaction between doctor and patient in the consultation is central to effective healthcare delivery. Studies of doctor–patient interaction have focused on examining how doctors and patients communicate in a range of clinical settings. In addition to describing the nature of and variation in the communication process, many studies have also sought to examine how this interaction influences other healthcare outcomes, such as patient satisfaction and treatment adherence.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
The development of audio and video-recording techniques has provided social and behavioral science researchers with a window into the private world of the medical consultation, allowing detailed investigations of the consultation process. From the early research it quickly became evident that there were considerable problems in the process and outcome of many consultations. Many patients reported that they had not been given sufficient information or had difficulty in understanding information which was presented in the consultation. Very often this was also found to be associated with a subsequent reluctance or inability to follow the doctor’s recommended treatment or advice. For example, in the landmark study of Korsch and Negrete (1972), which involved mothers taking their children to a paediatric outpatient clinic, about 20 percent of mothers were not informed clearly about the diagnosis and nearly 50 percent were uncertain afterwards as to the course of their child’s illness. This and other studies have also shown that patients often report feeling that they have not been sufficiently involved in the decision-making which may have occurred in the consultation (Guadagnoli and Ward 1998).
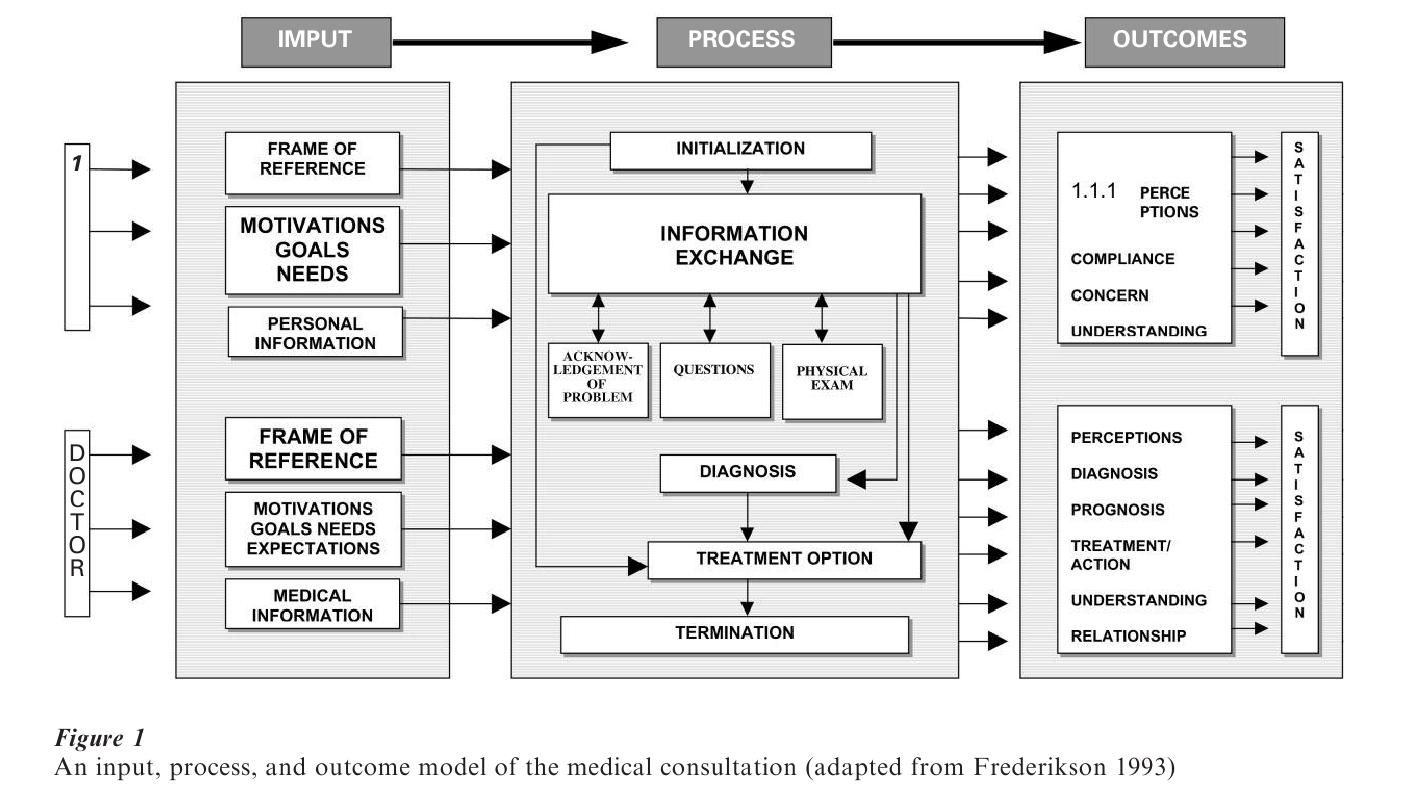
Many studies which have analyzed the process and outcome of the medical consultation have revealed that there is considerable variation in the pattern of doctor–patient interaction and that this is influenced by factors which the doctor and patient bring to the encounter. As a result, current theoretical frameworks for understanding doctor–patient communication tend to focus on the relations between inputs (i.e., the attitudes, beliefs, expectations, etc. which patient and doctor bring to the consultation), process (the nature of the encounter), and outcome (the short and longer term effects on the patient). An example of one such framework is provided by Frederikson (1993) and is shown in Fig. 1, which provides an indication of the range of variables which have been studied. This research paper will, therefore, follow this structure and focus initially on these three broad areas. One of the practical benefits of this research has been the development of interventions to improve doctor–patient communication, and this work will be summarized in the final section.
2. Input Factors In Doctor–Patient Communication
The main input factors in doctor–patient communication reflect variations between and within both doctors and patients. Studies have shown that patients can differ along many dimensions (e.g., age, personality, coping style, expectations, etc.) which can influence the process and outcome of a medical consultation. Similarly, there is growing evidence that, despite having had a common medical training, doctors differ in their attitudes and role perceptions in ways which can have a significant influence on what happens in the consultation. This section will, therefore, review a selection of the evidence on the nature and effects of the two input factors.
2.1 Patient Input Factors
A number of studies have shown that patients not only cope with health threats in diverse ways but also show consistent differences in how they want to be involved in the healthcare process. These studies also show that patients differ in the amount of information which they would like to receive about their health problem. For example, Miller et al. (1987) distinguish between two broad groups of patients whom they have labeled as ‘monitors’ and ‘blunters,’ with the former being more inclined to need and seek out information about their problem and treatment whereas the latter group prefer consultations in which relatively limited information is provided.
Patients come into the healthcare setting with different levels of biomedical knowledge, based on their past experience. There is also consistent evidence that patients have differing expectations for specific consultations and, for doctors, an awareness of these can be helpful in understanding not only why they are seeking help at that time but also in being able to respond effectively to their needs. Williams et al. (1995) have shown that the most common preconsultation expectation in primary care patients is for explanation and understanding of their problem, with much smaller numbers wanting tests, diagnoses, or support. These prior expectations can be important in determining outcomes since consultations in which patient expectations are met, have been shown to result in greater satisfaction and an increased willingness to follow advice or treatment.
These differences in patients’ expectations are also related to their perceptions of the role of the doctor. A number of studies have shown that patients differ in their perceptions of the role of the doctor and the extent to which it is appropriate to discuss different types of problems, particularly those of a more psychosocial type (e.g., Bower et al. 1999). However, even when patients feel that it is appropriate to discuss psychosocial problems with their doctor, this does not necessarily happen since the doctor’s own approach to the consultation may preclude this.
2.2 Differences Between Doctors
Doctors have been categorized in various ways according to their role perceptions and the extent to which they concentrate on the technical or more psychosocial aspects of patient care, as well as their beliefs about whether patients should be actively involved in the consultation and in decision-making about the management of the clinical problem (e.g., Grol et al. 1990). Inevitably these broad attitudinal differences are reflected in the way in which the consultation is conducted and in other aspects of professional behavior including decision-making, prescribing and management of clinical problems.
Although doctors undergo a common training and share a common body of knowledge and skills, wide variations in their consulting behavior have been noted. Part of this variation is a by-product of personality differences and can be seen in differences in interpersonal aspects of clinical practice but part is a reflection of differences in the approach to clinical problems. Some of these are between-individual differences whereas others reflect factors which can vary within the same individual, such as changing mood, time pressure, and various other contextual influences. In their overview of clinical decision-making, Schwartz and Griffin (1986) point out that there are often substantial disagreements between doctors when interpreting the same clinical information (e.g., x-rays). They also note that doctors may be inconsistent and disagree with their own previous judgments.
During clinical decision-making, the doctor is often faced with having to process a large amount of information about the patient and the possible diagnoses and treatment options. Since there are limits in what can be attended to and how much information can be held in working memory, doctors develop heuristics, or general strategies, for processing diagnostic and treatment information and these are subject to a range of influences. Kahnemann et al. (1982) have described a number of the heuristics which are used during clinical decision-making. Similarly, the doctor’s attitudes and beliefs about the doctor’s and the patient’s role can influence the weighting given to information from patients (e.g., the relative attention given to physical and psychosocial information). In addition, the doctors’ mood can affect information-processing in a number of ways by directly influencing the speed and accuracy of clinical problem-solving (Isen et al. 1991) or possibly by constraining access to mood congruent semantic information, as has been demonstrated in more general studies of the effect of mood on cognition.
3. The Consultation Process
There are a range of methods and frameworks for analyzing and describing the process of the consultation. One of the broadest distinctions made has been between consultations which are described as patient-centered and those which are doctor-centered, reflecting the extent to which the doctor or patient determines what is discussed (Grol et al. 1990). Doctor-centered consultations are ones in which closed-questions are used more often and the direction is determined by the doctor, typically with a primary focus on medical problems. In contrast, patient-centered encounters involve more open-ended questions with greater scope for patients to raise their own concerns and agendas.
A number of specific methods have been developed for carrying out detailed analyses of the social interaction between doctor and patient based on audio or videotapes or transcripts of the consultations (see Roter and Hall 1989). Early methods classified the verbal statements of the doctor and patient into those which were task or emotion-focused and then into more specific categories (e.g., asking questions, giving interpretations, etc.). Attempts have also been made to define a number of more general ways of classifying doctor–patient interactions. For example, one can distinguish between verbal and nonverbal information and, within the verbal domain, six broad categories can be defined (information-giving; information-seeking; social conversation; positive talk; negative talk; partnership building). From a meta-analysis of these broad categories (Roter 1989) it has been found that for the doctor, information-giving occurs most frequently (approximately 35 percent of the doctor’s communication) followed by information-seeking (approximately 22 percent), positive talk (15 percent), partnership building (10 percent), social conversation (6 percent), and negative talk (1 percent). In contrast the main type of patient communication consists of information giving (approximately 50 percent) with less than 10 percent involving information seeking.
A fairly recent and quite widely used method for analyzing the consultation process has been developed by Roter et al. (1997). This method classifies the doctor’s communication patterns into five distinct groups: (a) ‘narrowly biomedical’ characterized by closed-ended medical questions and biomedical talk; (b) ‘expanded biomedical’ similar to the narrowly biomedical but with moderate levels of psychosocial discussion; (c) ‘biopsychosocial’ reflecting a balance of psychosocial and biomedical topics; (d) ‘psychosocial’ characterized by psychosocial exchange; (e) ‘consumerist’ characterized by patient questions and doctor information giving. They found that ‘biomedical’ approaches were used more often with more sick, older, and lower income patients by younger, male doctors.
4. Outcomes Of Doctor–Patient Communication
Many studies of doctor–patient communication have attempted to evaluate the effects on a range of outcomes. Three broad groups of outcome have been studied, namely understanding and recall, satisfaction, and adherence, and each of these are now briefly discussed.
4.1 Patient Understanding And Recall
Changes in patients’ knowledge, understanding, and recall of the relevant information provided in the consultation have been assessed in a number of studies. Ley and co-workers have shown that about half the information provided in the consultation is forgotten by patients a short time afterwards but there is considerable range in what is recalled (see Ley 1997). This variation partly reflects the type of setting and sample used and partly the method which is used to test for recall. There are a number of other factors involved including the content of the information, the patients’ prior knowledge, and their level of anxiety. Generally information which is presented early in the consultation is recalled better (the primacy effect) as are statements which are perceived as being important or relevant. Moreover, recall is better for information which has been presented in an organised way based around specific themes (e.g., the nature of the problem, the details of the treatment, etc.).
4.2 Patient Satisfaction
Patient satisfaction is concerned with how patients evaluate the quality of their healthcare experience. It is increasingly being assessed in surveys of healthcare settings, as a marker of quality of care, along with other dimensions of quality such as access, relevance to need, effectiveness, and efficiency. Current research (e.g., Fitzpatrick 1997) views patient satisfaction as a multidimensional concept since patients differ in their views about specific aspects of their healthcare, such as the doctor’s behavior towards them, the information provided, the technical skills of the doctor, and the access to and quality of the healthcare setting. Generally the most important factor is the behavior of the doctor since this can influence significantly ratings of all the other aspects of healthcare.
There are a number of difficulties in assessing patient satisfaction. Results from most satisfaction surveys reveal very skewed data, apparently indicating very high levels of satisfaction across patient samples, particularly amongst older patients. Part of this problem seems to lie in the reluctance of patients to criticise healthcare services and part of it is due to the structure of the questionnaires which have been used to assess patient satisfaction (Ware and Hays 1988). In addition, the use of more in-depth methods which require patients to describe their experiences of health from their own perspective, typically give rise to a more critical view.
A number of studies have attempted to examine the relation between indices of the consultation process and measures of patient and doctor satisfaction. For example, in a study based on their five distinct patterns of consulting style (see above), Roter et al. (1997) showed that the highest levels of doctor satisfaction were found in those using the consumerist approach and the lowest levels were found in those using the narrowly biomedical approach. In contrast, the highest levels of patient satisfaction were found with those who had seen doctors using the psychosocial communication pattern whereas the lowest satisfaction scores were recorded in those who had experienced either of the two biomedical patterns.
4.3 Adherence To Advice Or Treatment
The most widely studied behavioral outcome from healthcare consultations is reflected in the extent to which the patient adheres to the advice or treatment offered by the doctor, and this topic is described in much more detail in another article (Patient Adherence to Health Care Regimens). Many consultations result in the prescription of treatment or advice by the doctor and the appropriate adoption of self-care behaviors, including use of medicines, is a key aspect to the self-management of most chronic illnesses. The incidence of reported medication nonadherence varies from 4–92 percent across studies, converging at 30–50 percent in chronic illness (Meichenbaum and Turk 1987). Even patients who have experienced major health problems, such as heart attacks, may show low levels of uptake of rehabilitation programs as well as considerable variation in the adoption of recommended lifestyle changes (Petrie et al. 1996).
In the context of doctor–patient communication, one cause of nonadherence arises from the poor cognitive outcomes outlined above, particularly poor understanding and recall of information presented in the consultation. Many patients lack basic knowledge about their medication but the relationship between this and their adherence is complex. Although some studies have demonstrated a positive association between knowledge and adherence, there are more that had failed to demonstrate a link. Moreover, interventions which enhance knowledge do not necessarily improve adherence.
The quality of communication with the doctor can also influence patients’ attitudes or beliefs about their illness or treatment which, in turn, have been shown to have significant effects on levels of adherence. Patients develop their own beliefs about the nature of their illness (Petrie and Weinman 1997) and these have been linked with a range of adherence-related behaviors other than the use of medicines. These include various self-management behaviors, such as dietary control and blood glucose testing in diabetes, attending rehabilitation, and the adoption of various lifestyle changes following myocardial infarction.
In addition to influencing patients’ perceptions of their illness, communication with the doctor can affect patients’ attitudes to their treatment. Work by Horne and Weinman (1999) has shown that patients develop very specific positive and negative beliefs about their prescribed treatment, both of which can have significant effects on treatment adherence. The positive beliefs are reflected in strong beliefs about the necessity of taking their medication in order to manage the illness whereas the negative beliefs reflect patients’ concerns about treatment side-effects or long-term dependence.
5. Interventions To Improve Doctor–Patient Communication
The majority of communication training interventions have been aimed at improving the communication skills of medical students or practitioners at various stages of training but a few have been targeted at patients, to enable them to get maximum benefit from a consultation.
Communication skills training is now a core part of the curriculum for medical students. Typically, students are provided with an overview of the basic skills of ‘active’ listening, which include the importance of developing good rapport and the use of open-ended questions early in the consultation, appropriate eye-contact, and other verbal and nonverbal responses to help the patient talk, together with the ability to summarize and arrive at a shared understanding of the patient’s problem (see Kendrick 1997). There is now consistent evidence that this type of training can result in enduring improvements in basic communication skills.
In addition to acquiring basic communication skills for work with all patients, medical students need to learn how to communicate about sensitive or difficult areas of clinical practice, including dealing with distressed patients or relatives and giving ‘bad news.’ Research in this area has shown that doctors tend to give detailed information rather than find out and respond to patients’ concerns and informational needs. As Maguire (1997) notes, this avoidance of patients’ worries can have negative effects in the short and longer term. An immediate consequence is that patients may remain preoccupied with their own concerns and fail to take in information or advice. They may also selectively attend to negative phrases or messages and be unresponsive or misconstrue more positive or neutral information.
Training in this area emphasises the value of patient-centered approaches, and exploring what patients know, think, and feel. Encouragement is given to take time to provide the patient with the information which they want, letting patients proceed at their own pace, and allowing information to be assimilated. The other key skills involve developing the ability not only to recognise distress but also to allow this to be expressed (Maguire 1997).
In recent years there have been a number of interesting interventions aimed at patients. Generally these have involved interventions for patients prior to a consultation in order to increase their level of participation, particularly to ensure that their own concerns are dealt with and that information provided by the doctor is clearly understood. A successful development of this approach can be seen in the work of Greenfield et al. (1985) who used a preconsultation intervention lasting 20 minutes for hospital outpatients who were helped to identify their main questions and encouraged to ask these in the consultation. Compared with control patients, these patients participated more actively in the consultation and this was also associated with better long-term health outcomes, including lowered blood pressure in hypertensives and better glycaemic control in diabetic patients.
6. Conclusions
Research on the nature, determinants, and effects of doctor–patient communication has revealed its complexity and its importance in effective healthcare delivery. Audio and videotaped recordings of the consultation have allowed the researcher to examine the nature of the interaction between doctor and patient. Although the tasks of coding and analysing this interaction have proved difficult, many studies have demonstrated that the interaction process can have major effects on a wide range of outcomes. These findings have been used for designing training in communication skills, and it will be a major task for researchers to evaluate the efficacy of these on the quality of healthcare delivery in the future.
Bibliography:
- Bower P, West R, Tylee A, Hann M 1999 Patients’ perceptions of the role of the general practitioner in the management of emotional problems. British Journal of Health Psychology 4: 41–52
- Fitzpatrick R 1997 Patient satisfaction. In: Baum A, Newman S, Weinman J, West R, MacManus I C (eds.) Cambridge Handbook of Psychology, Health and Medicine. Cambridge University Press, Cambridge, UK
- Frederikson L G 1993 Development of an integrative model for the medical consultation. Health Communications 5: 225–37
- Greenfield S, Kaplan S, Ware J E 1985 Expanding patient involvement in care: Effects on patient outcomes. Annals of Internal Medicine 102(4): 520–8
- Grol R, de Maeseneer J, Whitfield M, Mokkink H 1990 Disease- centered versus patient-centered attitudes: Comparison of general practitioners in Belgium, Britain and The Netherlands. Family Practitioner 7: 100–4
- Guadagnoli E, Ward P 1998 Patient participation in decision-making. Social Science and Medicine 47: 329–39
- Horne R, Weinman J 1999 Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. Journal of Psychosomatic Research 47: 555–67
- Isen A, Rosenzweig A, Young M J 1991 The influence of positive affect on clinical problem solving. Medical Decision Making 11: 221–7
- Kahneman D, Slovic P, Tversky A (eds.) 1982 Judgment Under Uncertainty: Heuristics and Biases. Cambridge University Press, Cambridge, UK
- Kendrick T 1997 Teaching communication skills. In: Baum A, Newman S, Weinman J, West R, McManus I C (eds.) Cambridge Handbook of Psychology, Health and Medicine. Cambridge University Press, Cambridge, UK
- Korsch B M, Negrete V F 1972 Doctor–patient communication. Scientific American 227: 66–74
- Ley P 1997 Doctor–patient communication. In: Baum A, Newman S, Weinman J, West R, McManus I C (eds.) Cambridge Handbook of Psychology, Health and Medicine. Cambridge University Press, Cambridge, UK
- Maguire P 1997 Breaking bad news. In: Baum A, Newman S, Weinman J, West R, McManus I C (eds.) Cambridge Handbook of Psychology, Health and Medicine. Cambridge University Press, Cambridge, UK
- Meichenbaum D, Turk D C 1987 Facilitating Treatment Adherence: A Practioner’s Guidebook. Plenum, New York
- Miller S M, Brody D S, Summerton J 1988 Styles of coping with threat: Implications for health. Journal of Personality and Social Psychology 54: 142–8
- Petrie K J, Weinman J (eds.) 1997 Perceptions of Health and Illness: Current Research and Applications. Harwood Academic, London
- Petrie K J, Weinman J, Sharpe N, Buckley J 1996 Predicting return to work and functioning following myocardial infarction: The role of the patient’s view of their illness. British Medical Journal 312: 1191–4
- Roter D L 1989 Which facets of communications have strong effects on outcome: A meta-analysis. In: Stewart M, Roter D (eds.) Communicating with Medical Patients. Sage, Newbury Park, CA
- Roter D, Hall J A 1989 Studies of doctor patient interaction. Annual Review of Public Health 10: 163–80
- Roter D, Stewart M, Putnam S M, Lipkin M, Stiles W, Inui T S 1997 The patient–physician relationship: Communication patterns of primary care physicians. Journal of American Medical Association 277: 350–6
- Schwartz S, Griffin T 1986 Medical Thinking: The Psychology of Medical Judgement and Decision. Springer Verlag, New York
- Ware J, Hays R 1988 Methods for measuring patient satisfaction with specific medical encounters. Medical Care 13: 669–79
- Williams S, Weinman J, Dale J, Newman S 1995 Patient expectations: What do primary care patients want from the GP and how far does meeting patient expectations affect patient satisfaction? Family Practitioner 12: 193–201




