View sample public health research paper on public health dimensions of disability. Browse research paper examples for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Introduction
Disability is often described by public health as a negative outcome, a failure to prevent an undesirable state. In this research paper, disability is described from a different point of view, that is, one that asserts the role of public health in promoting improved health and participation among people with disabilities. Explicit in this assertion is the assumption that people with disabilities are an integral part of the population, and therefore should be included in the public health mission, science, and programs for any nation.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
The strength of public health is that it creates a science to understand the prevalence and disparities of health conditions, and public health uses that science base to inform the development of policies and interventions to improve the public’s health. Similarly, by understanding the prevalence of disability, the circumstances of people with disabilities, and the disparities in health among people with and without disability, interventions can be developed to promote the health of people with disabilities. Moreover, improved health is likely to lead to greater social participation – work, social roles, and civic involvement – among people with disabilities across the life span.
Definition Of Disability
Disability is a remarkably complex, variable, and dimensional human experience. For that reason, an acceptable brief definition generally appears inadequate. People concerned about disability – clinicians, researchers, people with disabilities, their families, and policy makers – all seek to create a concise working definition to reflect their varied interests. Many of these efforts come up short. There is, in fact, no gold standard definition of disability.
Fujiura and Rutkowski-Kmitta note, ‘‘Disability identification is a judgment on the human condition, and its statistical summary represents more than a simple enumeration of those who are disabled and those who are not’’ (2001: 69).
One can identify at least four approaches to defining disability:
- Many equate a diagnosis with disablement; for example, one might assume that a person diagnosed with cerebral palsy experiences some level of disability. However, because of the great variability within cerebral palsy, knowing a diagnosis does not tell much about function. Even with the limited utility of equating diagnosis to disability, many groups of consumers, parents, and advocates organize themselves around conditions. In some respects, it is easier to organize around a condition than to attempt to embrace a concept as broad and perhaps vague as disability.
- Disability is often associated with eligibility for educational and rehabilitation programs, medical care, and income benefits. Organizations administering these programs establish eligibility criteria requiring people to ‘prove’ they have a disability. Proving eligibility for one program does not necessarily establish eligibility for another. A recent review of federal definitions of disability identified over 50 statutory definitions in various federal programs (Domzal, 1995). Because of the costs associated with these programs, eligibility is designed to limit the number of people deemed disabled.
- Yet another way to define disability is to characterize function. A functional approach to defining disability creates opportunities to understand human experience in a way that may be more relevant to people with disabilities as well as those who serve them through practice, policy, and research.
- Many disability advocates define disability by the degree of environmental accommodation required by an individual, thus focusing attention on the environments in which one lives rather than on a person’s ability level (Table 1).
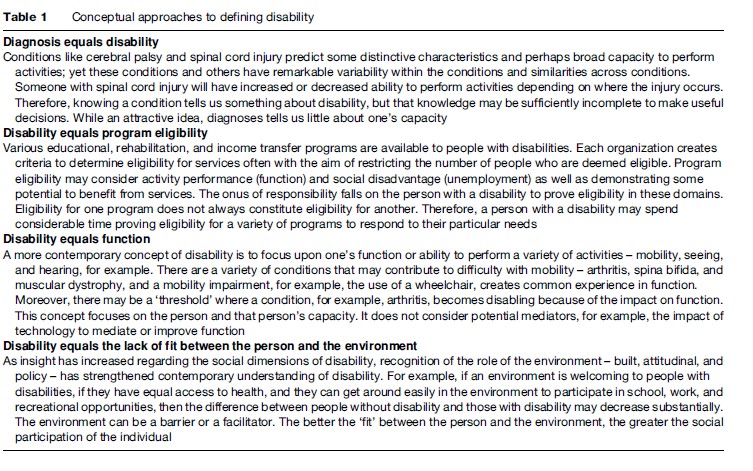
Definitions also vary on the purpose – disability defined to defend civil rights or promote health will be broader than those for monetary benefits, for example.
Additional conceptual limitations confound efforts to define disability. Disability may be culturally defined; less-developed countries often report lower rates of disability. Also, people may be reluctant to identify themselves as a having a disabling condition for any number of reasons – stigma, guilt, or punishment for past transgressions. For many, disability is treated as a threshold concept, that is, a person may report a limitation, but the severity of that limitation is not known. Disability surveys contribute to the creation of less dimensional definitions of disability by failing to capture severity or duration.
Models Of Disability
The earliest health classification focused on causes of death and was begun in the 1850s in Europe, which became the International Classification of Diseases (ICD-10). It was not until the 1950s that the World Health Organization (WHO) became conservator of classifications and morbidity was added to mortality as a part of the classifications. In disability, however, classification systems in the late nineteenth and early twentieth centuries emerged from early worker’s compensation legislation to determine reimbursement for temporary or permanent inability to return to work. Beginning in the 1930s, efforts moved from reimbursing people for loss of function to interests in rehabilitation that allowed people to reach or regain vocational capacity. The concern for vocational rehabilitation accelerated after World War II. In the 1960s, efforts to model disability turned toward measuring skills and behaviors, and thus various activities of daily living – such as eating, dressing, bathing – or ADL scales emerged (Frey, 1984). Subsequently efforts by Nagi (1965) and Wood and Badley (1980) under the auspices of the WHO focused on the multiple elements that define the lived experience of disability; thus efforts evolved to understand the relation among disease, function, and social roles, and later the effects of the environment (Pope and Tarlov, 1991; Brandt and Pope, 1997).
Efforts to construct models of disability mirror changes in social and public policies as well as changing notions about how people with disabilities are valued. Distinctions have been made between a medical model and a social model of disability. At the risk of oversimplification, the medical model implies that the problem of disability essentially resides with the person, and the role of providers is to fix the problem. A social model, on the other hand, posits that people with disabilities conduct their lives within a complex social structure characterized by barriers and opportunities created by systems, resources, and resilience. This approach suggests that the individual’s participation in society and quality of life is impacted at least as much by environment as by the person’s physical or mental status. Disability may be defined, then, as the fit between the person and the environment (for more about medical and social models, see the section ‘Medical/social models of disability’).
In 1981, the WHO published the International Classification of Impairments, Disabilities, and Handicaps (ICIDH) (WHO, 1981). The underlying concern of this model was to identify and characterize ‘planes of the experience’ of disability, recognizing that disability had dimensional characteristics that were defined by function and social roles. The foundation created by the ICIDH was followed by two decades of work resulting in the 2001 publication of the International Classification of Functioning, Disability and Health (ICF) (WHO, 2001). The ICF follows in the tradition of the ICD, addressing function in a systematic way similar to the ICD’s emphasis on etiology and morbidity. The ICF allows this scientific grounding for disability and functioning.
The ICF is one volume of the WHO family of classification systems, including the ICD-10, and it creates a conceptual framework and a classification system to portray multidimensional characteristics of the human experience; it is not limited to disability. In the model, a health condition is a disease, disorder, or injury that potentially precipitates changes in body function and structure, activities, and participation. Each of these terms – impairments, activities, and participation – is carefully defined (Figure 1).
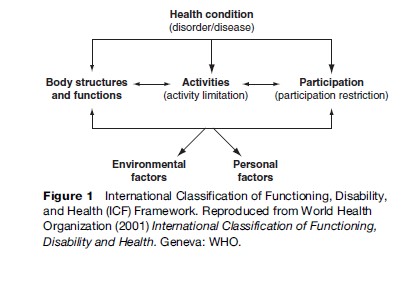
Impairments are changes in the body structure and function. Body functions include mental functions; sensory functions and pain; voice and speech functions; functions of the cardiovascular, hematological, immunological, and respiratory systems; functions of the digestive, metabolic, and endocrine systems; genitourinary and reproductive functions; neuromusculoskeletal and movement-related functions; and functions of skin and related structures. Body structure follows this same schema. Activities and participation include learning and applying knowledge; general tasks and demands; communication; mobility; self-care; domestic life; interpersonal interactions and relationships; major life areas; and community, social, and civic life.
The ICF also classifies environmental factors, including products and technology; natural environment and human-made changes to the environment; supports and relationships; attitudes; and services, systems, and policies. A major contribution of the revised model proposed by the ICF is the role of the environment – built, social, and attitudinal – to create barriers and facilitators for people with disabilities. The importance of the environment has led some people to define disability as the ‘fit’ between the person and the environment. Personal factors appear in the taxonomy and include age, gender, and social status, but these contextual factors are not yet classified in the ICF framework.
The ICF is not designed as a measurement tool, but as an organizing system to map human experience. The aim of the ICF is to create a classification system, not to replace existing clinical tools. The value of the ICF is that it captures the multidimensional experience of disability in its various domains; it creates a common language to describe complex experiences. An example may illustrate the robustness of the model. A person diagnosed with macular degeneration (a disease) may have changes in structure of macula that can diminish acuity (function); acuity can be measured. Vision loss is more than changes to the structure and function of the eye. It is problematic because it affects the ability to perform various activities – reading, driving, shopping, record keeping, and meal preparation. While these activities are important, the greater limitation of vision impairment may be the impact on social participation – getting together with friends, working, and educational and civic pursuits. The environment in the ICF model serves as a barrier or facilitator, and for people with vision loss, the environment may include signage, print size, light, transit systems, and access to technology. The environment also includes attitudes and policies. Improvements in signage, lighting, and print size as well as positive attitudes of medical personnel and the public do much to ameliorate problems posed in the environment.
The ICF components can be used to map individuals, groups, or populations, and the taxonomy also distinguishes among the roles of providers and policy makers. By and large, rehabilitation addresses efforts to improve the performance of activities – through alternative strategies (e.g., a closed circuit television) and development of new or alternative skills (e.g., Braille). Changes in public policy may affect the availability of public transportation systems that reduce the necessity of driving, and changing social values may improve community attitudes to be more inclusive (see Figure 1).
People with different diagnoses (e.g., spina bifida, spinal cord injury, and cerebral palsy) may have very similar functional difficulties (e.g., mobility or self-care). Differences in environments may allow more or less participation. Environmental changes can create more accessible businesses, homes, and transportation systems that benefit all people with mobility limitations regardless of the underlying diagnosis. Therefore, the ICF creates a language that allows one to identify characteristics common to people with disability as well as those that are distinct to individuals or particular groups.
Moreover, the ICF taxonomy can be used as a framework to direct interventions, define outcomes, and guide policy, as well as organize research efforts. For example, while the clinical interventions in rehabilitation are aimed at restoring function, the purpose of restored function is to promote full societal participation. One could use the ICF to map individual experiences or aggregate the effects of a rehabilitation program to illustrate the effectiveness of a rehabilitation intervention. Moreover, interventions for attention-deficit hyperactivity disorder (ADHD) may occur in the form of medication, addressing the impairment level. This intervention, hopefully, improves a child’s functioning as shown by improving his/ her attention. The attention helps improve the child’s ability to make and keep friends, and improve schoolwork. On the other hand, intervention could occur in the school room where a competent teacher is able to help a youngster with ADHD burn off excess energy during recess so that behavior is more settled and participation improves.
In addition, one can use this framework to describe a population by identifying dimensions of activities, participation, and the environment. The outcomes of clinical interventions and public health are increased participation. The pathways to accomplish a common goal may differ.
Medical/Social Models Of Disability
The traditional model of disability grew, reasonably, out of a medical perspective (e.g., a medical model). That perspective focused issues on the person’s problem(s), assumed medical care; thus presumed changes for the person would come in the form of adapting to their environment as best they could. Relevant policies focused on medical care issues. As Western society has developed civil rights emphasis over the past 40 years, a second model has evolved from people with disabling conditions. It is called the social model and frames issues of disability in society. In this model the emphasis is on the environmental barriers that impede or prohibit those with physical impairments from participating fully in society. Society is marginalizing people with disabling conditions and social change is needed in the form of changes in attitudes and adaptations of the physical environment; policy changes should be driven by human rights.
The ICF model integrates the two perspectives, medical and social, suggesting that both individual needs and societal responsibilities are important. This biopsychosocial model recommends that medical care and social change are needed, that personal adjustment and environmental changes are crucial for people with disabling conditions to participate fully in society (Figure 2).

Disability In Developed And Developing Nations
While the dimensional qualities of disability may be largely universal, the perception, rates, civil rights, and programs for people with disabilities vary remarkably in developing and developed nations. The United Nations (UN) Statistical Commission has developed guidelines for disability statistics to be used by any country (UN, 2001). The current state of prevalence rates around the world is chaotic – that is, prevalence varies from extremely low rates of less than 2% in lower-resource countries to as high as 20% in countries with high resources. The variation reflects differences in definitions in surveys or censuses (‘‘Is there anyone in the household who is deaf, dumb, or blind?’’ versus, ‘‘Are you limited in any way in any activities due to a disabling condition?’’), and include the stigma in some countries attached to identifying with disabilities. Developing countries often indicate that the disparities found in higher-resource countries are less apparent in their own countries because, for example, almost everyone is poor and unemployment is rampant. Disparities, however, are often shown in the number of children with disabilities receiving education services. From a policy standpoint, however, numerous countries with relatively few resources have developed strong policy statements. The white paper ‘‘On an Integrated National Disability Strategy’’ from South Africa is a prime example (Office of the Deputy President, 1997). Resources, however, restrict the opportunity to implement many policies. In addition, policy assessment is being completed in numerous countries by a project under the Center for International Rehabilitation (CIR), publishing reports that uniformly collect policy information on disability rights (CIR, 2003, 2004).
Estimated Population Of People With Disabilities
Given the debate over what constitutes disability, it is no wonder that there are similar debates about the prevalence of disability or estimated populations of people with disabilities. Several national, population-based surveys have different estimates of the population of people with disabilities. While these rates range from about 15–20% of the population, the differences arise from different case definitions of disability as well as differences in how surveys are administered. In the United States, the 2000 Census reports 49.7 million people age 5 and over (Waldrop and Stern, 2003; in 2003 the National Center for Health Statistics (NCHS) – a face-to-face survey – estimated that 34.3 million people (12%) were ‘‘limited in their usual activities due to one or more chronic conditions.’’ In addition, the NCHS survey estimated that 3.8 million (2%) required the help of others with ADLs such as eating, dressing, and bathing, and 7.7 million (4%) required help with instrumental activities of daily living (IADLs, e.g., household chores or shopping) (Schiller et al., 2005). A 2001 analysis of the 1999 Survey on Income and Program Participation (SIPP) data estimated that 44 million people aged 18 and over were disabled (Centers for Disease Control and Prevention [CDC], 2001). The Behavioral Risk Factors Surveillance System, a random digit dial telephone survey of adults age 18 and over, uses two disability questions to estimate state-level prevalence of disability. Using 2001 and 2003 survey data, states report a mean prevalence of disability of 19.1%.
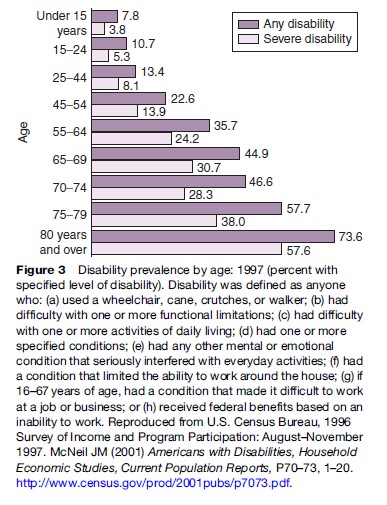
McNeil (2001), using 1997 SIPP data from the U.S. Census, estimates that 19.7% of people aged 5 and over reported disabilities, representing 52.6 million people. These estimates did not include people in institutions. McNeil estimated that 12.3% of the population (33.0 million people) had a severe disability, and 3.8% (10.1 million) needed personal assistance with one or more ADLs or IADLs. In his study, McNeil used a summary definition of disability that included nine dimensions, including limitation in performance of ADLs, IADLs, inability to work, and receipt of federal benefits based on inability to work. Figure 3 shows prevalence of disability by age group, and it shows a well-documented increase in prevalence of disability as people age.
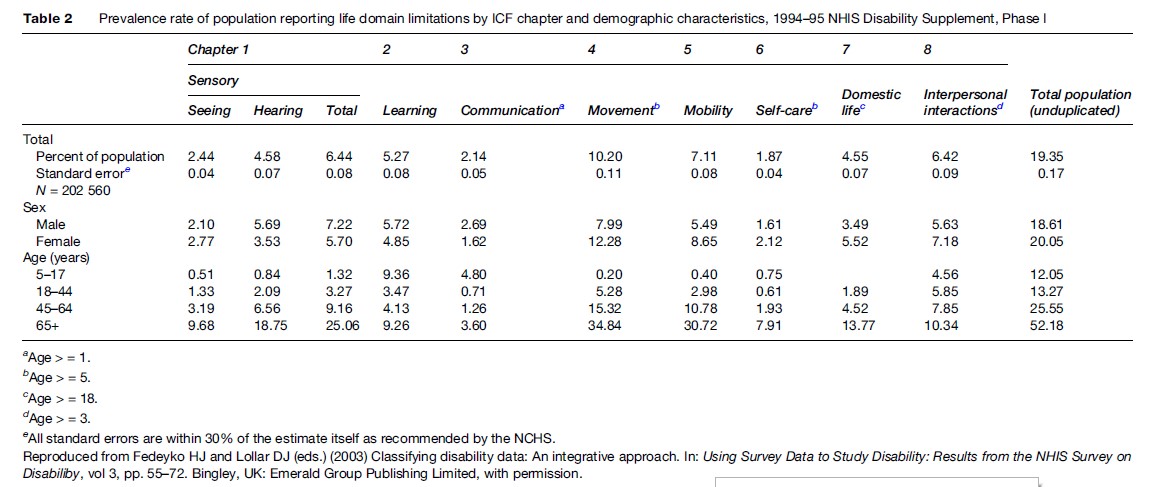
Fedeyko and Lollar (2003) employed the eight ICF domains to estimate prevalence of disability for people aged 5 and over using data from the 1994–1995 National Health Interview (NHIS) Disability Supplement. This noncategorical strategy reveals that 19.35% of the population report one or more life domain limitations, an estimate remarkably close to McNeil’s study. This analysis illustrates that people are slightly more likely to report limitations in two or more domains; 45.3% of respondents reported one limitation; 24.3% reported two, and 30.4% report three or more. Table 2 illustrates the distribution of the population employing ICF domains.
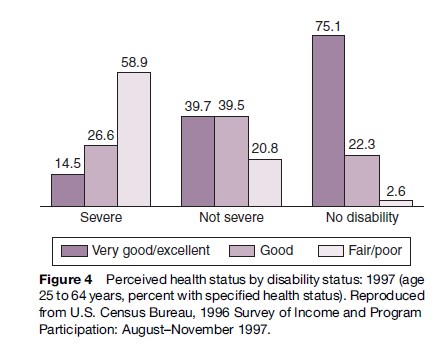
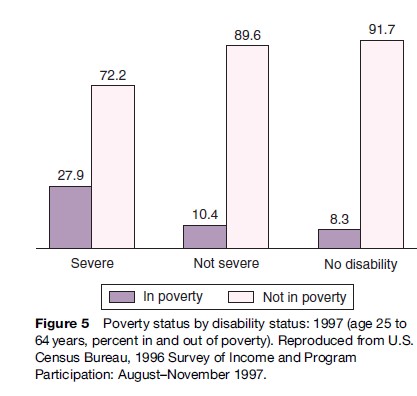
In addition to severity and domain, McNeil (2001) examined the relation between poverty and disability and poor health and severity of disability. The association between poverty and poor health as they relate to severity suggests the importance of understanding the broad social context of disability (Figures 4 and 5).
Older People With Disabilities
People who are older report higher rates of disability; higher rates of chronic conditions associated with aging contribute to functional decline. The six main conditions associated with aging – arthritis or rheumatism, back or spine, heart trouble/hardening of the arteries, lung and respiratory problems, deafness or hearing problems, mental and emotional problems – account for 23.9 million people who report functional difficulties (McNeil and Binette, 2001). Other factors – poverty, lower education levels, and race and ethnicity – predict higher rates of disability (McNeil, 2001).
Given the large number of older people who report disability, there is compelling evidence that the rate of disability is declining. A variety of studies conducted in the 1990s report that prevalence of disability declined 1.55% to 0.92% per year (Freedman et al., 2002). Hardy and her colleagues (2005) argue that for older people disability is a ‘‘dynamic process’’ in which many elders transition into and out of independence and disability. Debates regarding prevalence of disability among older people are complicated by the increasing number and longevity of older people. Fries (1980) argues that a ‘‘compression of morbidity’’ may reduce the period that chronic conditions affect function. Others have suggested that the trajectory of chronic conditions in a large population may result in prolonged periods of disablement. Other factors, including increased expectations of the baby boomer generation, increased use of technology, and better medical treatments contribute to the mixed understanding of future trends in aging and disability (Freedman, 2006).
Working-Aged People With Disabilities
While much of the research in the 1990s indicated reduced prevalence of disability among older people, research on people younger than 65 revealed opposite trends. Lakdawalla et al. (2004) examined NHIS data from 1984 to 2000 and noted that younger people reported greater rates of diseases (obesity and diabetes) that lead to disability as well as increasing economic incentives to report disability – even if function has remained unchanged. Lakdawalla and colleagues hypothesize that increased rates of obesity contribute to substantial increase in rates of disability. Obesity increases the likelihood of diabetes and musculoskeletal problems (primarily back-related), for example. In addition, improvements in technology may improve survival among people with severe chronic illnesses, and finally, the authors note that less-skilled workers may find economic advantage in seeking disability insurance, as wages have not kept pace with increases in disability insurance benefits. In another investigation, Bhattacharya et al. (2006) found that in addition to increases in diabetes among the working aged, from the early 1980s to the mid-1990s, there were increases in the prevalence of respiratory diseases such as asthma and chronic bronchitis as well as an increase in congestive heart failure.
Children With Disabilities
The UN Convention on the Rights of the Child (UN, 1989) includes specific language on the rights of children with disabilities in Article 23. It mandates that children with disabilities should enjoy a full life under conditions to ensure dignity, self-reliance, and participation in the life of the community. The right to special care and assistance for the children and their caregivers is included. In addition, assistance without cost and access to education, training, health care, rehabilitation, and services to achieve social integration and individual development is explicitly recommended.
Health Disparities/Disparities In Health Behaviors
The public health field often equates disability with sickness. The notions of illness and disability, however, are not points on the same spectrum. They are different concepts. People with disabilities can be sick, and overall they report poorer health than people without disabilities. That said, the aim of public health should be to improve the health of people with disabilities.
A recent examination of the 2001 and 2003 Behavioral Risk Factors System (CDC, 2006) provides insight into differences in prevalence of disability as well as self-reported health, health disparities, and disparities in health behaviors among people with and without disabilities.
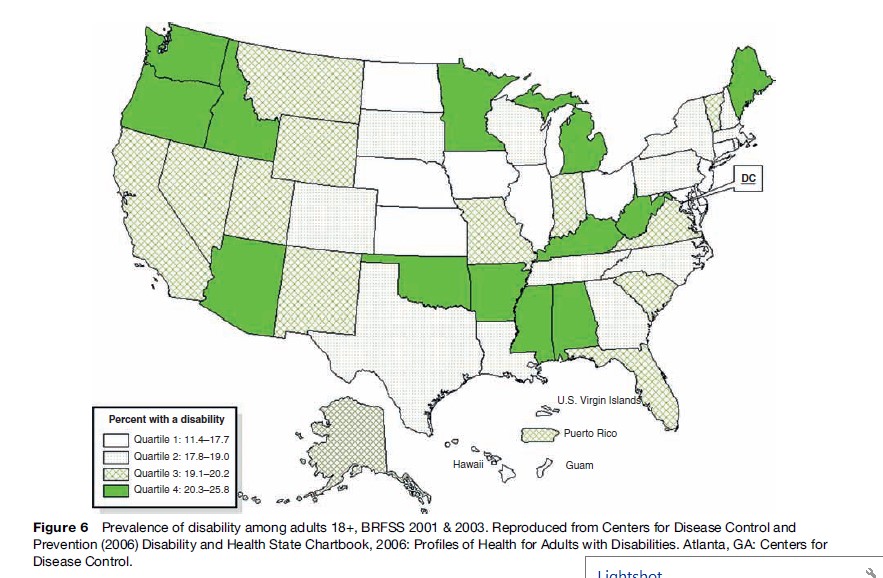
In the United States, rates of disability have considerable regional and state-to-state variability. The rate of disability for those aged 18 and over ranges from 11.4% in Hawaii to 25.8% in West Virginia. The median rate of the states is 19.1%. Figure 6 shows prevalence of disability in the states divided by quartiles. The prevalence of disability in these states, in all probability, differs because of differing health behaviors, access to health care, insurance, poverty, and education levels.
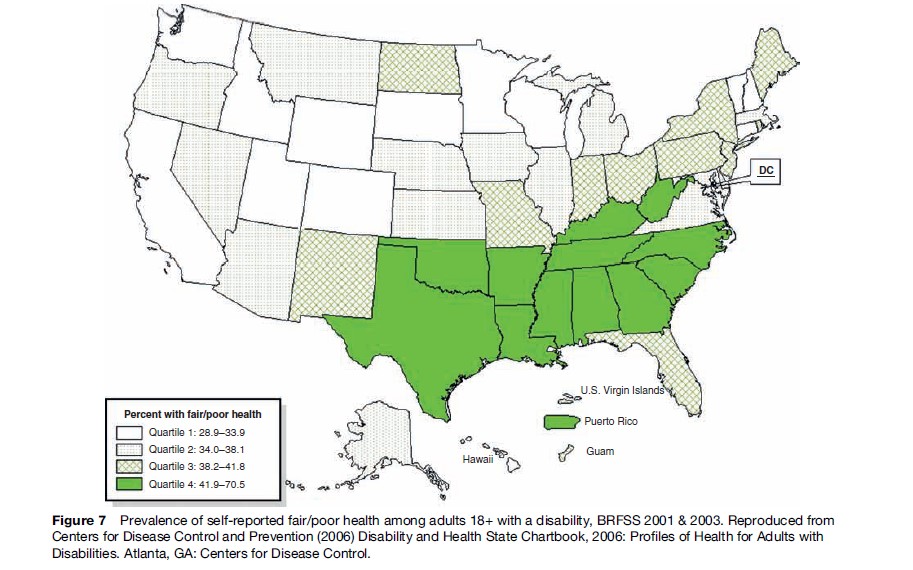
However, if one examines self-reported health among those with disability, a striking pattern occurs. Among those with disability, the highest percentage of those reporting fair/poor health occurs in the southeastern states of the United States. Figure 7 shows prevalence of fair/poor health among people with disabilities divided into quartiles. While states in the Ohio and Mississippi valleys (West Virginia, Kentucky, Mississippi) and the far northwest (Washington, Oregon, and Idaho) tend to report higher rates of disability, poorer health occurs in the southeast. Poorer health predicts higher health-care costs, greater demands upon caregivers – both paid and family – and diminished social participation.
The problem of poor health may not reside with access to health care but rather in health behaviors – smoking, obesity, and lack of exercise. In the CDC study, the mean rate of smoking among people with disabilities is 30.5% compared to 21.7% for those without disabilities. Similarly, people with disabilities are more likely to be obese(31.2%) compared to people without disabilities (19.6%), and people with disabilities are more likely to be physically inactive (22.4%) compared to those without disabilities (11.9%). These health behaviors may be contributing to overall poorer health. There are substantial differences in the rates of smoking, exercise, and obesity between people with and without disabilities. If health behaviors can be modified, then there may be greater opportunities to achieve national health goals.
These patterns of health disparities suggest that people with disabilities need to be included as a targeted population for broad public health interventions in smoking, obesity, and exercise. However, given the particular considerations of people with disabilities in terms of mobility, sensory, and cognitive function, interventions may need to be adapted to respond to those differences.
Health Promotion Interventions For People With Disabilities
The Rural Institute on Disability at the University of Montana in the U.S. has been particularly successful in designing, implementing, and evaluating health interventions of people with mobility and cognitive limitations.
One well-established program, Living Well with a Disability, is an 8-week curriculum that can be delivered in the community by a trained facilitator. Living Well has been replicated in 27 U.S. states; it is based on the independent living philosophy that fosters control and decision making of the consumer. The program emphasizes goal-setting and goal clarification process and teaches skills for generating, implementing, and monitoring solutions to problems. Living Well also provides tools for managing one’s health and making healthy lifestyle changes, increasing physical activity, developing and maintaining healthy relationships, improving nutrition, avoiding depression and frustration, and advocating for community health to maintain gains (University of Montana Rural Institute, 2004).
Several evaluations of this program have examined improved health and reduced utilization of health care including physician visits, emergency room care, and hospitalizations. This kind of program is especially well suited to be delivered through independent living programs, community-based programs operated for and by people with disabilities.
For people with intellectual disabilities, the University of Montana has developed a nutrition program and the University of South Carolina College of Medicine has developed a fitness and nutrition program (Ewing, 1999). Ewing’s Steps to Your Health addresses nutrition, exercise, stress management, and obesity, as well as communication style. This intervention relies upon a facilitator to work with groups of consumers in the community.
While some health promotion activities are designed as community-based interventions, others are web-based and serve a broader national audience. One example is the National Center on Physical Activity and Disability (NCPAD). This website provides information on health promotion, including strategies, resources, and regimens to promote exercise and fitness. The website is becoming increasingly interactive with the idea of having consumers provide details about function and desired outcomes; the electronic system then generates suggestions based upon the individual’s profile (see the section ‘Relevant websites’).
Training
Public health curricula have traditionally dealt with disability as one of the negative health outcomes to be prevented. While primary prevention of disabling conditions is an important public health mandate – whether from injury, chronic illness, developmental disabilities, birth defects or environmental toxins – primary prevention efforts will never be completely successful. Individuals will continue to be born with or acquire conditions that are disabling. Public health as a field, and therefore, public health education, should acknowledge and train professionals to address this large segment of the population.
Public health training is currently increasing coverage of disability with courses specifically addressing epidemiology of disability, health-care access and disparities, ethics, emergency responses, and maternal and child health. Curricular materials are also available and are growing in their use (OHSU, 2005; BU, 2006). An additional support to the growing field of disability in public health in the United States is found in the Disability Forum of the American Public Health Association (APHA). This group within APHA provides an on-going presence for professionals working in disability, and also is the consultant to APHA disability-related policies of the organization as well as matters related to members with disabilities and appropriate accommodations.
Conclusion
In summary, disability is developing as an emphasis in public health science, policy, programs, and training. The field of public health has evolved from a primary emphasis on mortality through morbidity to the next emerging area to be addressed.
Bibliography:
- Allen D and Garberson W (eds.) (2007) One in Five: Disability in the Public Health Curriculum. Unpublished manuscript.
- Bhattacharya J, Choudhry K, and Lakdawall DN (2006) Chronic disease and rends in severe disability in working-age population. In: Field MJ, Jette AM, and Martin L (eds.) Workshop on Disability in America: A New Look, pp. 113–142. Washington, DC: National Academies Press.
- Brandt EN and Pope AM (1997) Enabling America: Assessing the Role of Rehabilitation Science and Engineering. Washington, DC: National Academy Press.
- Centers for Disease Control and Prevention (2001) Prevalence of disabilities and associated health conditions among adults – United States, 1999. Morbidity and Mortality Weekly Report 50(7): 120–125.
- Center for International Rehabilitation (2003) International Disability Rights Compendium. Washington, DC: CIR.
- Center for International Rehabilitation (2004) International Disability Rights Monitor: Regional Report of the Americas 2004. Chicago, IL: International Disability Network.
- Centers for Disease Control and Prevention (2006) Disability and Health State Chartbook, 2006: Profiles of Health for Adults with Disabilities. Atlanta, GA: Centers for Disease Control.
- Domzal C (1995) Federal Statutory Definitions of Disability. Washington, DC: U.S. Department of Education, National Institute on Disability and Rehabilitation Research.
- Drum CE, Krahn GL, Ritacco BA, and Drake AE (eds.) (2004) Disability and Public Health Curriculum Outline. Portland, Oregon: Oregon Office on Disability and Health.
- Ewing GB (1999) Steps to Your Health. Columbia, SC: South Carolina Department of Disabilities and Special Needs and the University of South Carolina School of Medicine.
- Fedeyko HJ and Lollar DJ (eds.) (2003) Classifying disability data: An integrative approach. In: Using Survey Data to Study Disability: Results from the NHIS Survey on Disabiliby, vol 3, pp. 55–72. Bingley, UK: Emerald Group Publishing Limited.
- Fujiura GT and Rutkowski-Kmitta V (2001) Counting disability. In: Albrecht GL, Seelman KD, and Bury M (eds.) Handbook of Disability Studies, pp. 69–76. Thousand Oaks, CA: Sage.
- Freedman VA, Martin LG, and Schoeni RF (2002) Recent trends in disability and function among older adults in the United States: A systematic review. Journal of the American Medical Association 299(24): 3137–3146.
- Freedman VA (2006) Late-life disability trends: An overview of the evidence. In: Field MJ, Jette AM, and Martin L (eds.) Workshop of Disability in America: A New Look, Summary and Background Papers. Washington, DC: National Academies Press.
- Frey WD (1984) Functional assessment of the ’80s: A conceptual enigma, a technical challenge. In: Halpern AS and Fuhrer MJ (eds.) Functional Assessment in Rehabilitation. Baltimore, MD: Brooks.
- Fries J (1980) Aging, natural death, and the compression of morbidity. New England Journal of Medicine 303(3): 130–135.
- Hardy SE, Dubin JA, Holford TR, and Gill TM (2005) Transitions between states of disability and independence among older persons. American Journal of Epidemiology 161: 575–584.
- Lakdawall DN, Bhattacharya J, and Goldman DP (2004) Are the young becoming more disabled? Health Affairs 23(1): 168–176.
- McNeil JM and Binnette J (2001) Prevalence of disabilities and associated health conditions among adults—United States, 1999 MMWR. Morbidity and Mortality Weekly Report 50(07): 120–125.
- Nagi SZ (1965) Some conceptual issues in disability and rehabilitation. In: Sussman MB (ed.) Sociology and Rehabilitation. Washington, DC: American Sociological Association.
- Office of the Deputy President (1997) Integrated National Disability Strategy: A white Paper. Ndabeni, South Africa: Office of the Deputy President.
- Pope AM and Tarlov AR (1991) Disability in America: Toward a National Agenda for Prevention. Washington, DC: National Academy Press.
- Schiller JS, Adams PF, and Coriarty Nelson Z (2005) Summary of health statistics for the U.S. population: National Health Interview Survey, 2003. Washington, DC: National Center for Health Statistics. Vital Health Statistics 10(224) 1–104.
- The University of Montana Rural Institute (2004) Living well with a disability: An update. Rural Disabilities and Rehabilitation Research Progress Report #19. http://mtdh.ruralinstitute.umt.edu/blog/?page_id=1574
- United Nations (2001) Guidelines and Principles for the Development of Disability Statistics. New York: UNseries 4, No. 10.
- United Nations General Assembly (1989) Convention on the Rights of the Child, Document A/RES/44/25 (12 December). https://www.un.org/en/development/desa/population/migration/generalassembly/docs/globalcompact/A_RES_44_25.pdf
- Waldrop J and Stern S (2003) Disability status: 2000. Census 2000 Brief, Issued March 2003. http://www.census.gov/prod/2003pubs/c2kbr-17.pdf
- Wood PHN and Badley EM (1980) People with Disabilities–Toward Acquiring Information which Reflects More Sensitively their Problems and Needs. New York: World Rehabilitation Fund.
- World Health Organization (1981) International Classification of Impairments, Disabilities, and Handicaps. Geneva, Switzerland: WHO.
- World Health Organization (2001) International Classification of Functioning, Disability and Health. Geneva, Switzerland: WHO.
- Albrecht GL, Seelman KD, and Bury M (2001) Handbook of Disability Studies. Thousands Oaks, CA: Sage.
- Disabled Peoples’ International. http://www.dpi.org/
- Field MJ, Jette AM, and Martin L (2006) Workshop on Disability in America: A New Look. Washington, DC: National Academies.
- Field MJ and Jette AM (2007) The Future of Disability in America. Washington, DC: National Academies.
- Kinne S, Patrick DL, and Doyle DL (2004) Prevalence of secondary conditions among people with disabilities. American Journal of Public Health 94: 443–445.
- Lollar DJ and Crews JE (2003) Redefining the role of public health in disability. Annual Review of Public Health 24: 195–208.




