View sample public health research paper on literacy and public health. Browse research paper examples for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Efforts to promote self-efficacy and empowerment in health care are changing how the role of the patient is viewed, from passive participant to informed and activated consumer. Health information has become increasingly accessible to consumers of health-care services as a result of the Internet and mass media. In this new era, greater attention on how information is accessed, understood, and used is warranted.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
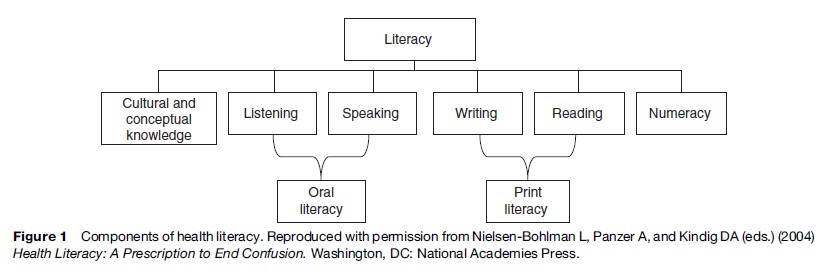
The definition of health literacy accepted by the Institute of Medicine (IOM) and National Library of Medicine (NLM) in the United States is the ‘‘degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.’’ It is a multifaceted concept, of which reading ability is a fundamental component. An individual’s ability to read, comprehend, and take action based on health-related material may be closely related to the ability to read, comprehend, and take action based on other types of materials (general literacy). The prerequisite health literacy skill set ultimately is determined by the level of complexity of tasks imparted to individuals by a particular health-care system, and include more than one’s ability to read text in print materials. Rather, health literacy skills encompass a broad range of cognitive and social processes that are involved in the act of comprehending and responding to both oral and print communication. Individuals therefore need to have adequate listening and speaking skills, numeracy ability, and conceptual knowledge to engage in routine self-care activities and to navigate complex health-care systems (see Figure 1).
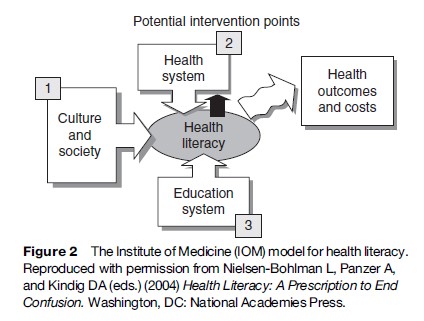
Within the IOM model, determinants of individual health literacy skills include culture and society and the educational system, as well as the health-care system (see Figure 2). This, perhaps, was the most groundbreaking achievement of the IOM report: the acknowledgment of limited health literacy as a problem mostly situated in the way essential health information is communicated to consumers of health care. As such, the IOM report recommends that the responsibility for improvement must be shared by these various sectors and that the health-care system carries significant, but not complete, responsibility for improvement.
Beyond The U.S. IOM Model
While the accepted definition of health literacy is the same in the United States and the United Kingdom, the definition of health literacy in continental Europe has been expanded to not only include basic health, patient, and consumer competencies (e.g., self-care, navigation, making healthy decisions in the selection and use of goods and services) but citizen competencies as well. This means individuals must share in the responsibility of promoting and protecting health in a society by being informed on health matters, advocating on behalf of health issues, and being proactive instead of only responding to health problems at the time when decisions need to be made. Thus, health literacy in this definition refers to being an empowered consumer of health care.
Both the U.S. and European definitions reflect a broad conceptual understanding of health literacy, although it should be noted that the related body of research literature that has led to the eventual creation of this field of study has operationalized the term in a very limited manner. This is explained in part due to the difficulty in measuring certain aspects of the conceptual definitions, and by the early beginnings of research in this area that focused on health associations with patients’ reading ability.
Background
The term ‘health literacy’ formally arrived and became part of the U.S. public health lexicon during the 1990s, although investigations of whether patients possess the necessary skills to read, understand, and act on available health information had been conducted for some time before then. What began as a handful of studies evaluating associations between poor reading ability and health knowledge and behaviors since has expanded to an independent field of study. Currently, there are approximately 1000 health literacy-related publications; a large proportion of these address the readability of health materials. Texts, annual conferences, and numerous available funding opportunities are further indication of the rapidly growing awareness of the health literacy agenda. In the United States, where the term was conceived and the clear majority of research performed, the federal government has identified improving the health literacy of Americans as a priority for national public health efforts. As a result of the increased recognition of the importance of literacy skills in health care, the U.S. Department of Education conducted the first national assessment of adult health literacy in 2003, and is expecting to track the progress of Americans at five-year intervals.
From a global perspective, other countries have also begun to individually address the problem of limited health literacy. Both Switzerland and the United Kingdom have recently completed national health literacy surveys, the first of their kind in Europe. Likewise, formative responses to health literacy have been implemented and are now underway within many different national health-care systems, including Canada, Ireland, and the United Kingdom. Awareness of the issue and its potential impact on health care and costs has made health literacy a priority for an increasing number of governments around the world.
Epidemiology
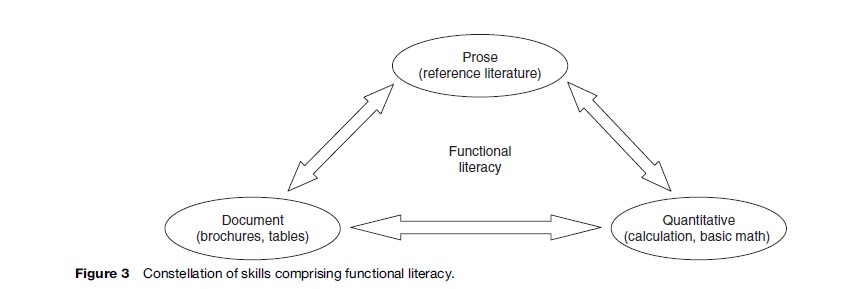
In the United States, estimates of health literacy were first derived from general adult literacy statistics that measured an individual’s functional literacy skills within a variety of daily living situations (including health), as defined by the National Adult Literacy Act of 1991 (see Figure 3). According to the U.S. National Assessment of Adult Literacy (NAAL) of 2003, approximately 14% of U.S. adults possess skills in the lowest level of prose and document literacy, which is termed ‘below basic,’ and 22% are at the lowest level for quantitative literacy. In practical terms, adults at the below-basic level have difficulty reading and understanding information, even in short and common texts (prose, document literacy), and locating easily identifiable numerical information (quantitative literacy). At best, they can perform only the most simple and concrete literacy tasks. However, those with only ‘basic’ literacy proficiency also have limited abilities and are likely to be hindered in routine daily activities. When considering individuals with basic and below-basic skills combined, as many as one-third to one-half of adults in the U.S. have limited literacy skills. Estimates are significantly higher among the elderly; nearly two-thirds of Americans over the age of 65 have limited levels of prose and document literacy. Those who are socioeconomically disadvantaged, belong to racial/ ethnic minority groups, and are from rural locations are also disproportionately afflicted by limited literacy skills.
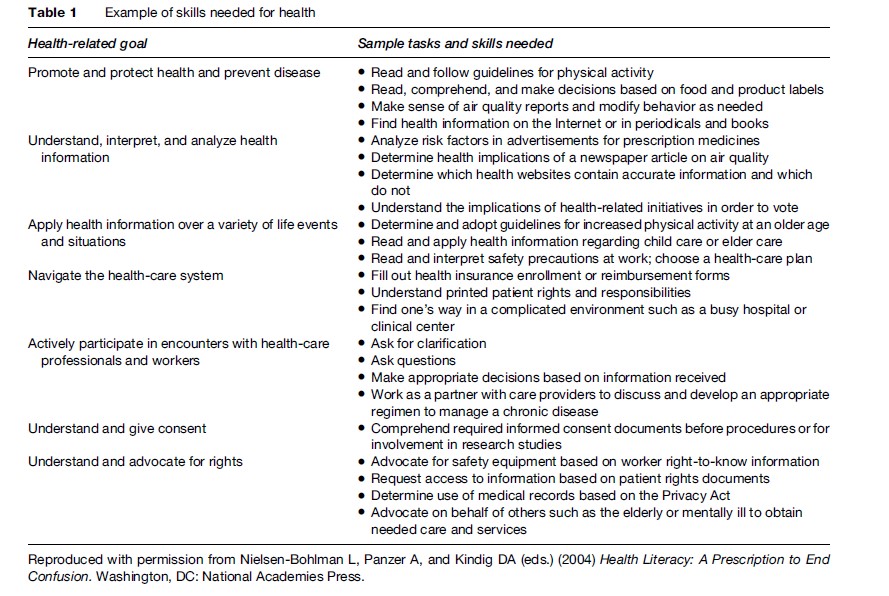
These estimates, however, may not give the full picture for health literacy. For instance, reading fluency and the full range of literacy skills is likely to vary with an individual’s familiarity with the content of the text. Health materials and encounters may be more likely to use difficult and often-unclarified medical terms that are not familiar to many individuals. Therefore, the estimates of limited health literacy using the NAAL general literacy assessment may underestimate the problem. As a response to this concern, the NAAL 2003 included a health literacy assessment that evaluated health literacy proficiency among U.S. adults. However, this and other assessments have all limited the measure of literacy to the ability to use print health information, and not the full list of activities that may fall under capabilities to perform health tasks (see Table 1). The report showed the average health literacy scores of Americans to be lower than average general literacy scores of adults. Those over 65 years of age had the lowest levels of health literacy, placing them on average at the threshold between below-basic and basic proficiency. Adults between the ages of 25–39 reported the highest levels of health literacy, yet still only placing them on average in the basic health literacy proficiency category. Evidence from this first health literacy assessment also confirms the persistence of disparities in health literacy skills as reported with general literacy skills. African-American and Latino/ Hispanic men and women tested at lower levels of health literacy compared to Whites. In all, the conclusion appears to remain the same: Large numbers of U.S. adults lack the basic competencies enabling them to effectively use various health materials and to accomplish health related activities.
Considering Culture
The racial/ethnic divide in literacy and health literacy skills highlights the significance of limited health literacy as a likely contributing factor to noted health disparities in the United States. These differences may be deeply rooted in access and quality of opportunities in education and other needed socioeconomic resources. Educational attainment alone has been strongly linked to poorer health in numerous studies. But health disparities may also reflect less experience with the terminology used by physicians and other health-care providers. For people of all ethnicities, ages, and other variations in experience, cultural factors can strongly influence beliefs, communication, and behaviors related to health. Culture is defined as the shared ideas, meanings, and values acquired by individuals as members of society; this is not entirely separate from the idea of health literacy. Acquiring cultural ideas, meanings and values continues throughout one’s lifetime, as ‘lived experiences’ build for individuals. The World Health Organization has acknowledged health literacy within its own definition of the concept as a set of active, adaptable, and dynamic skills that evolve as does our cultural experience.
For health, culture includes not only language and vocabulary but also the definitions and meanings attached to health and illness concepts, expectations regarding interactions with health professionals, and proper utilization of health-care services. It is the context that influences notions of how people interface with various health services, and this is the ‘lens’ through which an individual interprets and gives meaning to health information, and eventually to what choices are made. Embedded in culture are many individual, family, and societal factors that determine health behaviors and related communication, much of which precede and shape the gradual development of health literacy proficiency.
Measurement
In earlier health literacy studies, general literacy tests from educational research, such as the Wide Reading Achievement Test (WRAT) and the Slosson Oral Reading Test (SORT) were used. Since then, the assessment of health literacy skills in clinical research settings has been predominantly performed with one of two instruments: the Rapid Estimate of Adult Literacy in Medicine (REALM) and/or the Test of Functional Health Literacy in Adults (TOFHLA) or short form (S-TOFHLA). The REALM tests an individual’s ability to recognize and pronounce words, while the TOFHLA measures the ability to read and comprehend text and perform computations involving health-related activities (e.g., reading a prescription label and calculating dosing intervals). Both the REALM and TOFHLA were modeled after general functional literacy measures and provide estimates of literacy ability as applied to health-care contexts.
The limitations of these instruments have often dictated which one would be used in a particular research study.
For instance, the REALM can be administered quickly (approximately 2 min), but it does not measure comprehension and it is only available in English. The TOFHLA, on the other hand, measures comprehension and is available in both English and Spanish, but its length (20 min or more) has been an obstacle to use when research is performed in clinical settings. A shortened version of the TOFHLA (S-TOFHLA) has been developed, but it still requires about 8 min, precluding its use in many busy clinical settings.
A new screening instrument for limited literacy, the Newest Vital Sign (NVS), is a six-item literacy assessment structured around the activity of reading and demonstrating an understanding of information included on a nutrition label. The NVS is short enough (3 min) to use in clinical settings, and it is available in both English and Spanish. Shortened versions of the REALM have also been developed, but are not widely used at this time. Others have also proposed single-item questions to ascertain likelihood of health literacy problems, as well as using years of school completed as a proxy measure for limited literacy ability. Both of these screening strategies have been criticized, though, and may misclassify many patients as having adequate literacy skills when they actually may not.
Authors of these tests recommend only aggregate testing to provide profiles of the reading ability of groups of patients in clinics or health systems. They currently do not recommend testing individual patients unless health education interventions are being specifically tailored for the patient. In addition, these experts recommend attending to privacy issues in recording literacy levels in medical records. If providers test patient’s literacy skills, they need to be sensitive to patient’s concerns and potential embarrassment, and ensure that testing results will be confidential. As an additional word of caution, it should be acknowledged that there is no evidence to date that suggests literacy testing results in improved delivery of health care or improved health outcomes. Clearly, additional research is needed to examine the impact and usefulness of literacy feedback to clinicians before promoting the use of literacy measures in a clinical role.
Why Limited Literacy Or ‘Health Literacy’ Affects Health Outcomes
There is a significant amount of research literature demonstrating that individuals with less education, in terms of years of school completed, have worse health outcomes. In most of these studies, educational attainment appears to have a direct effect on health after adjusting for socioeconomic indicators. However, the causal pathways between education and poorer health, including mortality, have not been extensively articulated. While the relationship between health literacy and health outcomes also is not entirely clear, there are plausible mechanisms by which literacy could directly affect health behaviors, compliance with medications, and other pathways to health. Empirical data collected over the past two decades support these links. Limited health literacy has been associated with less health knowledge, worse self-management skills, higher hospitalization rates, worse health, greater mortality risk, and higher health-care costs. In the few studies that have demonstrated associations between limited literacy and health outcomes, literacy has been a more dominant indicator of outcomes than years of education.
In order to have a general understanding of the projected pathway through which limited health literacy impacts health outcomes, we have broken down the definition of health literacy to describe in more detail its three requisite functions: (1) obtaining health information and services, (2) processing and understanding health information, and (3) making appropriate health decisions.
Obtaining Health Information And Services
Prior studies have shown that individuals with limited oral, written, and quantitative literacy skills face considerable difficulty in accessing print health information materials, and are often challenged when engaging in dialogue with health-care providers. This is likely attributed to the high reading difficulty found among consumer health information materials, which have been reported upon in numerous contexts. Yet low literacy may impair access to health information and subsequent recommended health services in ways other than the ability to read existing printed health materials and to communicate effectively with health services providers. Lower literate adults have previously been found to be more likely to report their physician to be their only source of health information compared to more functionally literate patients, who may often access multiple informational sources. This is problematic, considering many physicians and other health services providers do not communicate health information and instructions in a manner that is understandable to lower-literate patients, in particular, and to patients without clinical training in general.
Many adults, regardless of education and background, find it difficult to navigate the health-care system and decipher the complex health information required to successfully manage personal and family health care. This highlights an important point: An individual’s health literacy skills may be closely related to his or her ability to read, comprehend, and take action based on other types of materials (i.e., general literacy). Yet reading comprehension varies with an individual’s familiarity with the content of the text. Therefore, accessing health information that uses difficult medical terms or conversing with a health-care provider may be problematic for an even larger proportion of adults in the United States than previously suggested.
Processing And Understanding Health Information
As a result of problems accessing health materials, persons with limited health literacy skills are at greater risk of having difficulty comprehending health information and medical instructions. Consequentially, several research studies conducted among individuals living with a chronic disease have reported poorer knowledge among lower literate patients of concepts that are central to having a proper understanding of both disease and treatment. For instance, lower-literate persons with HIV were less able to have a working definition of a CD4 count or viral load. Other studies have cited examples of poor understanding of self-care activities among patients with limited literacy skills, including improper use of metered-dose inhalers for adults with asthma and inadequate knowledge of dietary restrictions among hypertensive patients. This association has also been found for understanding of basic terms commonly used to describe recommended preventive services and medication label instructions.
In many of these cases, however, a sizable percentage of functionally literate adults had difficulty understanding basic medical terms associated with the care of their chronic condition or information presented on a medication label. This is further evidence of the inadequacies that persist throughout health-care systems and their ability to provide services to those with limited health literacy skills.
Making Appropriate Health Decisions
The impact of limited health literacy has a cumulative effect. Limitations in access to comprehensible health information leads to poor knowledge and understanding, affecting decision making and health behaviors, and ultimately health outcomes. Patients and families are increasingly asked to participate and to be held responsible in health-care decisions. Yet those with limited health literacy skills will likely face problems during information exchange and deliberation on health decisions due to a lack of information and/or miscommunication and a desire to appear knowledgeable.
The consequences of less-informed health decisions are reflected in outcomes. Patients defined as having inadequate health literacy according to the TOFHLA have been previously reported as having poorer physical and mental functioning, higher rates of hospitalization, and, among diabetic patients, poorer glycemic control. Recently, studies found that literacy (as measured by both the REALM and S-TOFHLA) was associated with a greater mortality risk among the elderly. Health literacy may be intrinsically linked to several socioeconomic and cultural factors within an ecological model, and the combined effect could be predicting these health outcomes.
Responding To Limited Health Literacy
At present, little information is available on how best to overcome health literacy barriers. Simplifying written health information has been previously recommended to improve comprehension of health information; however, these ‘enhanced print’ strategies support only minimal improvement in knowledge outcomes among lower-literate individuals. The inclusion of visual aids (i.e., graphics) has been proposed as a better way to improve patient comprehension, recall, and compliance with recommended health behaviors. Multimedia tools have also been promoted as a more sophisticated means for health education that might best respond to the special health learning needs of adults with limited literacy. However, findings have been mixed concerning the efficacy of either graphics in print materials or the use of multimedia tools to improve knowledge transfer among patients with limited health literacy.
Other system-based interventions have been developed and tested with more robust results. Clinician-directed training to improve provider–patient communication has led to sizable increases in preventive screening utilization among patients with low literacy. Intensive care-management strategies have been proven to be effective at reducing health literacy barriers among patients with certain chronic conditions, such as heart failure and diabetes, and at a fairly low cost. More research is needed to provide more conclusive evidence as to best practices for overcoming the problem of health literacy, in terms of health promotion, disease prevention, chronic disease management, and health-care navigation.
The Challenge Of A Health-Literate Society
The 55-year-old World Health Organization preamble states that ‘‘informed opinion and active cooperation on the part of the public are of utmost importance in promoting health.’’ Yet many countries have restrictive policies on health information provision, limiting the opportunity for attaining our goal of a health-literate society. In the United States, poor health literacy has been described as a silent epidemic, with almost half of the adult population lacking the literacy skills to understand and use health information. There are increasing demands on people to be informed and activated consumers, able to make good choices about their health plan, which include picking a good provider and hospital for services and choosing the drug benefit program that best serves their needs and is most cost-effective. Health insurers in the United States promote consumerism in health care through the use of high-deductible health plans with savings accounts and health reimbursement arrangements. They promise consumers choice among health plans, providers, and even treatments; however, this all requires well-informed consumers. In reality, most patients in the United States usually depend on their doctors to act in their best interests.
The challenges of addressing the magnitude of the problems of health literacy are heightened by growing diversity in many countries, as culture gives meaning to health information. An evidence-based review of health literacy research by the Agency for Healthcare Quality and Research in 2004 found that numerous interventions had been shown to improve knowledge in mixed populations that included substantial numbers of people with low literacy. However, the field of research is not currently advanced enough to determine whether certain interventions actually reduce literacy-related disparities in health, and more research is needed to better identify approaches for improving health communication for culturally diverse populations.
Informed, activated consumers and patients with better outcomes define a health-literate public. They are more concordant with the people who provide health services; seek care earlier because they recognize and understand warning signs; read and comprehend instructions; understand what their doctors advise them; and are not afraid to ask questions when they do not understand. Health literate people can seek new and reliable information on the Internet, critically hear and read the news, and place new health studies in context. In articulating a vision for a health-literate America, the IOM report described a society in which everyone has the skills to obtain, understand, and use health information effectively. Importantly, health institutions and systems in the society are responsible for facilitating this by providing clear communication and necessary support to promote health.
Those working in public health – private and public funders, professionals from the academic sector, healthcare providers, policy makers, researchers, marketers, publishers, information technology professionals, and others – must educate those on the front lines delivering health to embrace and address health literacy. Perhaps it is time for a multi-sector-driven ‘manifesto’ or ‘convention’ on health information provision to advance the knowledge base and practice to enhance a health-literate public.
Improving health literacy is both a process and an outcome for improving health and health care in the United States and elsewhere. To reach the goal of a health-literate public requires prioritization by leadership and worldwide professional communities to raise awareness of the issue and to develop meaningful solutions.
Bibliography:
- Baker DW (2006) The meaning and the measure of health literacy. Journal of General Internal Medicine 21: 878–883.
- Davis TC, Long SW, Jackson RH, et al. (1993) Rapid estimate of adult literacy in medicine: A shortened screening instrument. Family Medicine 25: 391–395.
- Dewalt DA, Berkman ND, Sheridan S, Lohr KN, and Pignone MP (2004) Literacy and health outcomes: A systematic review of the literature. Journal of General Internal Medicine 19: 1228–1239.
- Gazmararian JA, Williams MV, Peel J, and Baker DW (2003) Health literacy and knowledge of chronic disease. Patient Education and Counseling 51: 267–275.
- Howard DH, Gazmararian J, and Parker RM (2005) The impact of low health literacy on the medical costs of Medicare managed care enrollees. American Journal of Medicine 118: 371–377.
- Human Resources and Social Development Canada (1997) Literacy Skills for the Knowledge Society: Second Report of the International Adult Literacy Survey. Ottawa, Canada: Human Resources and Social Development Canada.
- Kickbusch I (2002) Health literacy: A search for new categories. Health Promotion International 15(3): 183–184.
- Kickbusch I, Wait S, and Maag D (2006) Navigating Health: The Role of Health Literacy. London: Alliance for Health and the Future.
- Kutner M, Greenberg E, and Baer J (2005) A First Look at the Literacy of America’s Adults in the 21st Century (NCES 2006–470). U.S. Department of Education. Washington, DC: National Center for Education Statistics.
- Nielsen-Bohlman L, Panzer A, and Kindig DA (eds.) (2004) Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press.
- Parker RM, Baker DW, Williams MV, and Nurss JR (1995) The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. Journal of General Internal Medicine 10: 537–541.
- Parker RM, Ratzan SC, and Lurie N (2002) Health literacy: a policy challenge for advancing high-quality health care. Health Affairs 22: 147–153.
- Pignone M, DeWalt DA, Sheridan S, Berkman N, and Lohr KN (2005) Interventions to improve health outcomes for patients with low literacy. A systematic review. Journal of General Internal Medicine 20: 185–192.
- Ratzan S. From passive patient to health-competent consumer, Consumer Policy, Review; Nov/Dec 2003: 13: 6 205–211.
- Rudd RE, Kirsch I, and Yamamoto K (2004) Literacy and health in America. Princeton, NJ: Educational Testing Service.
- Schillinger D, Grumbach K, Piette J, et al. (2002) Association of Health Literacy with Diabetes Outcomes. Journal of the American Medical Association 288: 475–482.
- Schwartzberg JG, VanGeest JB, and Wang CC (eds.) (2004) Understanding Health Literacy: Implications for Medicine, Public Health. Chicago, IL: AMA Press.
- Wolf MS, Gazmararian JA, and Baker DW (2005) Health literacy and functional health status among older adults. Archives of Internal Medicine 165: 1946–1952.
- Wolf MS, Knight SJ, Durazo-Arvizu R, et al. (2006) Associations of race, literacy, and income with PSA level among men with newly diagnosed prostate cancer. Urology 68: 89–93.




