View sample public health research paper on social science and public health. Browse research paper examples for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
History
Public health has always been concerned with the ways in which social conditions influence the health and well-being of communities and human populations. The disciplines of both public health and social science emerged in the latter part of the nineteenth century along with a recognition of the needs of the poor and marginalized groups and the association between living conditions and health. However, it was not until the mid-twentieth century that professionally trained social scientists became actively involved in public health programs, and by the 1980s accredited schools of public health in the United States were required to provide formal training in the social and behavioral sciences. The most important challenges for improving health in the twenty-first century involve social, cultural, and behavioral change. Our knowledge about how social and behavioral factors affect health has grown enormously, but achieving the individual and societal changes needed to reach public health goals is no easy task. Political and economic barriers deeply rooted in the social order constrain what is practically feasible. Nevertheless, new emerging approaches to structural change offer possibilities for surmounting these obstacles and producing higher levels of global community health.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
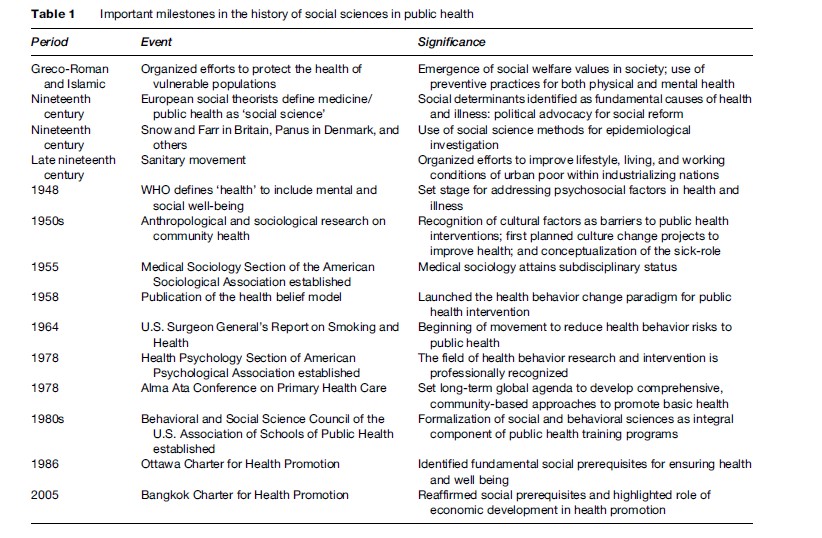
Table 1 highlights important milestones in the history of social science contributions to public health. In the nineteenth century, social theorists in Europe called attention to the unequal distribution of infectious disease among the poor and working classes, citing unhealthy living conditions of crowded urban slums, inadequate diet, and physically taxing labor as contributing to the poor health of the disadvantaged. Many important figures contributed to a broad discourse that framed public health issues as socially produced, some with an overt political agenda such as Marx and Engels, others with a more epidemiological approach such as Snow, Panum, and Farr, some as activist physicians such as Villerme´ and Gue´rin, and still others with a more sociological orientation such as Virchow and Durkheim ( Janes et al., 1986). Often referred to as nineteenth-century ‘social medicine,’ the contributions of this period are significant for establishing the idea that public health is a social science, and that social structures and change generate population-level health effects. Moreover, social reform to improve health is also rooted in the early work of advocates such as Virchow and Chadwick. The late nineteenth century saw the rise of the Sanitary Movement, with organized efforts to improve standards of hygiene, living, and working conditions. However, the turn of the century ushered in the bacteriological era, and attention shifted to the discovery and control of biological pathogens in the early decades of the twentieth century.
The growth of social and behavioral science applications in public health was strengthened by the redefinition of health in 1948 by the newly formed World Health Organization (WHO) as ‘‘a state of complete physical, mental and social well-being, and not merely the absence of disease or infirmity.’’ Since that time, WHO and other national and international organizations have affirmed the importance of psychosocial well-being as an integral component of health. This expanded conceptualization of health required the expertise of many disciplines to formulate policies and design programs to improve health conditions around the globe. The scope of health promotion again expanded in 1986 with the adoption of the Ottawa Charter for Health Promotion, which identified fundamental prerequisites for a healthy society, including peace, shelter, education, food, income, a stable ecosystem, sustainable resources, social justice, and equity. This broad agenda set the stage for an even broader role for social science in public health. The need for comprehensive, multisector approaches to global health promotion was reaffirmed and further outlined in 2005 through the Bangkok Charter for Health Promotion.
Many observers have noted that the AIDS epidemic that became global in the 1980s had a significant impact on the position of social and behavioral research in public health: It was the first modern pandemic that could not be controlled primarily through environmental and technological means such as sanitation and vaccines. Controlling the spread of HIV required changing social norms and values, as well as individual behavior, and social scientists rose to the challenge in large numbers (Benoist and Desclaux, 1995). Anthropologists, sociologists, psychologists, and other social scientists have made important contributions to understanding HIV risk behavior and to designing interventions to promote safer sex and reduce transmission from intravenous drug use. Important conceptual and methodologic advances have accompanied this expanded role.
The 1950s: Seminal Developments
The post-World War II era ushered in a period of tremendous growth and development for the social and behavioral sciences in public health. There were two main thrusts of this groundbreaking era, one focused on health modernization in developing countries, the other focused on population-based screening for medical conditions. It was an era of great optimism about the potential for social engineering of health development and the application of social science methods to understanding and improving the health of populations (Paul, 1956).
In the international arena, anthropologists in the 1930s and 1940s began working on projects aimed at improving the health and diet of traditional populations (Firth, 1934; Richards, 1939; Malinowski, 1945). Diet and nutrition were an important focus of these activities, exemplified by the hiring of Ruth Benedict, Margaret Mead, and others by the U.S. National Research Council’s Committee on Food Habits. Beginning in 1950, a number of anthropologists were appointed to key positions with international health organizations, including Cora DuBois at the World Health Organization, Edward Wellin at the Rockefeller Foundation, Benjamin Paul at the Harvard School of Public Health, and George Foster and others at the Institute for Inter-American Affairs, forerunner of the U.S. Agency for International Development. As Coreil writes:
The appointment of anthropologists to institutional posts paralleled the rapid expansion of public health programs worldwide as modern medicine was introduced on a large scale in many areas. The primary role of anthropologists was seen as that of identifying significant cultural barriers to the acceptance of new public health programs. (Coreil, 1990: 5)
Many of the important development projects of this era are described in the classic volume edited by Benjamin Paul, Health, Culture and Community (1955). These studies defined culture as a barrier to desirable health practice, and introduced the role of social scientist as a culture broker whose expertise could be applied to facilitate directed change. In particular, the focus was on diffusion of health technology to solve problems of ‘underdevelopment’ by overcoming resistance to change grounded in traditional values, institutions, and practices. The conceptualization of culture as a barrier to good health became firmly rooted in social science thinking throughout the latter half of the twentieth century, and it persists to the current day in various reformulations such as ‘cultural awareness’ and ‘cultural diversity.’ However, critics also have challenged this perspective as reflecting ethnocentric and neocolonial ideas of progress through culture change.
Concurrent to the above developments, the 1950s brought forward within industrialized countries such as the United States focused attention to mobilizing large numbers of people to take part in various public health campaigns. Here again, officials encountered resistance to citizen participation and turned to social science expertise for solutions. In this case, social psychologists took the lead in developing approaches to analyzing the problem and formulating interventions based on emergent models of individual behavior change. The seminal framework that emerged was the health belief model. Drawing upon cognitive and behavioral theories of human behavior, the model conceptualized health practices as motivated by value expectancies, or subjective assessments of the personal benefits of particular outcomes and the expectations that certain actions will achieve desired goals ( Janz et al., 2002). Developed in the context of a campaign to screen the adult U.S. population for tuberculosis through voluntary chest X-rays offered in mobile clinics, the model was advanced to help explain why participation remained low, despite the availability of free and convenient screening opportunities. The model posits that the decision to take action to protect one’s health is determined by four factors: (1) whether people consider themselves susceptible to the condition; (2) whether the condition is perceived as having serious personal consequences; (3) whether a specific action is expected to reduce the risk of getting the condition or the consequences of it; and (4) whether the perceived benefits of the action outweigh the subjective costs or barriers to taking action. This rational cost–benefit model dominated health behavior change programs for several decades, with various elaborations and modifications over time, and set the stage for the development of other cognitive-behavioral models of health practice. Various behavior change models based on principles of motivation and learning theory were elaborated in subsequent decades and came to occupy a central position in health promotion interventions.
Maturation Of The Field
Social science contributions to public health were bolstered significantly by the development of more sophisticated conceptual models and methods of research and data analysis, including both quantitative and qualitative techniques. The maturation of the field is reflected in the scope and influence of scholarly articles published in the multidisciplinary journal Social Science and Medicine, which first appeared in 1966 and currently boasts a large international readership and a high impact rating among scientific journals. In the 1980s, significant developments occurred through the involvement of social scientists in international health activities related to child survival programs, HIV/AIDS, and tropical diseases. These activities were promoted and funded through intergovernmental agencies such as UNICEF, WHO, and TDR (the UNDP/World Bank/WHO Program for Research and Training in Tropical Diseases), as well as through bilateral development agencies such as USAID, CIDA, and their European counterparts. Established in 1975, TDR has played an especially important role in advancing social science research on tropical diseases through programs that train scientists in developing countries and that support research focused on sociocultural factors and health. A noteworthy strength of its programs has been the promotion of gender-focused research.
Shift From Infectious To Chronic Disease
Over the course of the twentieth century, the public health enterprise underwent significant transformation as a result of a radical shift in the focus from infectious diseases to chronic conditions as the major challenges to population health in industrialized societies. Tied to demographic, environmental, and social change, this transformation, also known as the ‘epidemiologic transition,’ required profound alterations in how public health problems were addressed. Chronic conditions such as heart disease, cancer, diabetes, mental illness, and health problems of older persons replaced tuberculosis, pneumonia, childhood diarrhea, and other infections as the leading causes of morbidity and mortality in industrial countries (although TB, malaria, and later AIDS remained major killers in developing countries). As chronic diseases and disability became the focus of public health interventions, the role of social and behavioral factors became increasingly important for disease prevention and control. Multilevel models that emphasized the social and political environment reemerged to replace the traditional medical model grounded in the germ theory of disease as well as the traditional public health model emphasizing host–agent–environment interactions. Anthropology, sociology, political science, demography, gerontology, and other social sciences made important contributions to this reframing of public health. With their focus on broad social processes and macro-level determinants, the social sciences helped to redefine the public health agenda as one integrally concerned with policy, economics, social organization, and cultural dynamics across diverse institutions. This shift built upon advances in the professional development of these disciplines, theoretical and methodologic contributions, and political advocacy on the part of diverse communities.
Professional Development Of The Field
At the close of the twentieth century, important conferences and publications marked the maturation of the field and recognition of the significance of ‘higher-level’ analysis of the social and cultural aspects of health. In 1998 the U.S. Centers for Disease Control and Prevention (CDC), in collaboration with the American Psychological Association and other professional social science organizations, sponsored a multidisciplinary conference, ‘‘Public Health in the Twenty-First Century: Behavioral and Social Science Contributions.’’ Two years later, the National Institutes of Health organized an agenda-setting conference called ‘‘Towards Higher Levels of Analysis: Progress and Promise in Research on Social and Cultural Dimensions of Health’’ (Schneiderman et al., 2001). A recurrent theme in these meetings was the recognition that, despite impressive advances in understanding the biological and genetic bases for disease, ‘‘knowledge about biological and genetic markers is important but limited in predicting who gets sick, who seeks treatment for health problems, and who recovers from illness. The social sciences contribute to filling these gaps in our understanding of health’’ (NIH, 2001: 1). These conferences marked a critical juncture in the development of the field, that is, the accumulation of knowledge about the complex interplay of macroand micro-level influences on health, as well as new technologies for putting into practice strategies for influencing the impact of those factors. That same year appeared an integrative textbook for the field, Social and Behavioral Foundations of Public Health (Coreil et al., 2001). Outside the United States, similar events and publications marked this important turning point in the field, such as the volume published by the French Association for Medical Anthropology Applied to Development and Health (AMADES), Syste´mes (Hours, 2001b), the creation of the WHO Commission on Social Determinants of Health (2005), and the 2007 conference ‘‘Social, Cultural and Economic Determinants of Health’’ held in Portugal.
Disciplines
Health Education
In the United States, and to a much lesser extent in Europe and elsewhere, health education has become one of the most organized and professionalized of the social sciences within public health. It is the only field that has its own credentialing system for Certified Health Education Specialists and has an association specifically for professionals working in public health, the Society for Public Health Education. The Health Education Section of the American Public Health Association represents the interests of many social and behavioral scientists working in this field. Most U.S. schools of public health offer graduate degree programs in health education, with a focus on health promotion and health behavior change in their curricula. In line with these foci, health education research and training draw heavily on theories and models of individual behavior change from health psychology. Community-based approaches to health promotion that apply principles of community development and participation have also gained prominence.
Medical Anthropology
The field of medical anthropology emerged in the 1960s, with roots in physical anthropology and human evolution, the study of primitive medicine, cross-cultural psychiatry, and the involvement of anthropologists in international health. The Society for Medical Anthropology, organized in 1967, became a section of the American Anthropological Association in 1972, and today constitutes the largest group within that organization. In contrast, the medical sociology and health psychology sections of their parent organizations have never constituted more than a small percentage of overall membership. The involvement of medical anthropologists in public health has grown steadily over the past 40 years, with the growth of interdisciplinary fields such as social and cultural epidemiology, maternal and child health, international health, environmental health, reproductive health, and health education. Although the number of U.S. medical anthropologists working in domestic public health settings has always outnumbered those working internationally, their contributions to the latter arena have been more prominent because of its cross-cultural orientation. In contrast, medical anthropology departments with an international health focus have occupied prominent positions in European schools of public health, including programs in the Netherlands, the United Kingdom, Italy, et politiques de sante´: de la sant´e publique a` l’anthropologie France, and Germany (Saillant and Genest, 2007). In addition, a number of strong medical anthropology programs have been developed within European departments of anthropology, such as those at the University of Amsterdam and Heidelberg University, which provide graduate-level training for many developing-country students.
Medical Sociology
The Medical Sociology Section of the American Sociological Association was established in 1959. Since that time, sociologists have made important contributions to public health research and practice in a variety of areas. Most notably, sociological research on the social determinants of health, health inequalities, access to care, the organization of services, health policy, and family health have dominated sociological studies of population-based health. In particular, sociology and demography have played a major role in shaping the field of social epidemiology. Using the methods of survey research and statistical analysis, researchers have identified significant variation in health status and conditions for groups defined by sociodemographic variables, including age, gender, race, class, ethnicity, occupation, education, marital status, and religion. Increasingly sophisticated techniques for analyzing large data sets such as vital statistics, population surveys, and health service indicators have provided useful information for identifying populations at risk, for measuring unmet need for services, for planning health programs, and for formulating health policy. In another line of activity, sociologists have made important contributions to understanding the social construction of health problems, that is, how social processes shape how and why societies come to define certain conditions and trends as public health problems. Examples of this include the framing of teen pregnancy as a social problem, public reactions to the AIDS epidemic, and concern with the growing prevalence of obesity in wealthy societies.
Health Psychology
In 1977 George Engel published a seminal article titled ‘‘The Need for a New Medical Model,’’ in which he advocated for a multidisciplinary biopsychosocial model of health that incorporates psychological and social dimensions of well-being. This signaled the emergence of health psychology as a subdiscipline; the following year, the Health Psychology section of the American Psychological Association was established. Like other social and behavioral sciences, the field of health psychology developed partly in response to the rise of chronic disease and to the role of personal health habits in the etiology and management of conditions such as cancer, heart disease, and diabetes. In addition, new models for understanding the complexity of contextual factors in the illness process enlarged the scope of analysis and intervention. The biopsychosocial model emphasizes the interplay of biological, psychological, and social factors in illness, and gives importance to multiple determinants and macro-level processes (Taylor, 2006). For example, stress and social support have been increasingly recognized as contributing factors in health. This broad view is compatible with the ecological perspective of public health.
Important contributions from health psychology include the study of health behaviors such as smoking and exercise; research on stress, social support, and immune function; interventions for addictions; the relationship between mental illness and physical illness; and practical approaches to the management of chronic illness. Some particular areas of note include studies of Type A behavior, hostility, and heart disease; health promotion strategies such as smoking cessation and weight management; methods for enhancing sexual health such as safer sex practices to reduce sexually transmitted infections; and psychosocial factors in the progression of cancer. As noted previously, social psychological models of health behavior change have dominated the public health field of health promotion and education.
Demography
The field of demography has affinity with public health because public health’s core discipline, epidemiology, draws heavily on demographic concepts and methods. Both demography and epidemiology are based on population-based approaches that utilize quantitative indicators such as fertility and mortality rates, changes in population and disease trends over time, statistical modeling of large data sets, and use of secondary data. Key epidemiologic concepts such as morbidity and mortality rates, incidence and prevalence, and trends over time draw heavily on demographic methods. Another example of the interface of the two disciplines is research on the epidemiologic transition, a process that begins with declines in mortality, particularly from reductions in infant and child deaths due to infectious diseases, followed by lower fertility rates and increased longevity and life expectancy. Demographic principles are also closely related to the study of gerontology. As people live longer in both industrial and developing countries, the study of aging and health problems of the elderly has gained increasing importance in public health.
Gerontology
Founded in 1945, the Gerontological Society of America is the oldest of the professional social science associations in the United States reviewed for this research paper. It represents the multidisciplinary field of aging studies, which includes biomedical research and clinical practice, as well as social science, policy, and public health interests. The importance of aging issues for public health was reflected in the formation of the Gerontological Health Section of the American Public Health Association in 1978. As the populations of industrial societies have progressively aged over the past few decades, the need to provide for the health and social needs of older adults has produced many challenges. The needs for long-term care, chronic disease and disability services, and decision making related to end-of-life issues have grown in importance. In particular, as the large cohort of baby boomers who were born in the postWorld War II years reaches old age, nations will continue to be challenged in providing for the well-being of an aging population. Ethical issues related to health-care costs, access to expensive life-prolonging technologies, quality of life, and the right to die continue to be debated. The field of gerontological health offers a variety of perspectives on these issues and will increasingly occupy a central role in the public health arena.
Political Science
Because public health by definition is concerned with issues in the arena of social action, political science offers important perspectives on policy analysis, health legislation and regulation, the influence of commercial interests on health care, and the relationship between the political system of a society and its public health agenda. In a different approach, much has been written on the health systems of communist countries such as Cuba and China, and the public health consequences of the breakup of the former Soviet Union. Analyses of policy cycles and processes offer insights on how political bodies influence the outcome of legislative efforts and social movements. The manipulation of public health issues in the cause of political agendas, such as impacting national election outcomes, provides fertile ground for study. A good example of a political science approach is provided in Turshen’s (1989) book The Politics of Public Health, which takes a critical perspective on health care in capitalist societies. In fact, social scientists from various backgrounds including anthropology and sociology have adopted critical stances on public health issues, applying political economic analyses to problems such as reproductive health, HIV/AIDS, health disparities, and the plethora of health problems affecting the poor and disenfranchised.
Another area of health research based on perspectives from political science focuses on the notion of community engagement and the concept of social capital. Stimulated by the work of Robert Putnam (2000), researchers have investigated the relationship between civic participation in voluntary associations and the overall health status of populations, as measured by indicators such as morbidity and mortality and the prevalence of chronic diseases. This line of research has shown a positive relationship between civic involvement and population health, offering new avenues for community health promotion.
History
Historical studies offer yet another social science approach to understanding the relationship between society and health. Important insights have been gained through the study of health conditions in social and political context through time. Analysis of societal responses to major public health threats in the past and of the consequences of different approaches at critical periods in history offers lessons for current and future planning. For example, Barnes’s (1995) account of competing social constructions of tuberculosis in nineteenth-century France illuminates the political forces behind societal response to disease. Another example is found in Rushing’s (1995) analysis of societal reactions to major epidemics over the centuries, such as the bubonic plague of the Middle Ages, cholera epidemics in the nineteenth century, and the AIDS epidemic of the late twentieth century. Using evidence from both historical accounts and the well-chronicled recent epidemic, he finds parallels in collective behavior and social response to severe, large-scale threats. Finally, we have much to learn from the contrasting ways that societies have dealt with the needs of their most vulnerable groups throughout history.
Conceptual Frameworks
A number of social and behavioral science conceptual frameworks offer tools for understanding the complex etiology of health problems in today’s world, and translate into different approaches to problem amelioration. These can be grouped into four broad categories: social ecology, health promotion, interpretive studies, and critical perspectives.
Social Ecology
The social ecology model is rooted in the traditional public health model of host–agent–environment, developed to study the relationship between human populations (host), disease pathogens (agent), and the physical setting in which people live and work (environment). For instance, the transmission of waterborne illnesses can be studied in terms of the relationship between the environmental reservoir (water source), the introduction of an agent (microorganisms), and host (human) exposure to the water source. The latter model can be contrasted with the traditional biomedical model, which assumes that illness can be explained by the presence of pathogens in the body (germ theory of disease) and abnormal physiological processes or biochemical imbalances. The biomedical model accords only a minor role to psychological and social processes, and views mental and social phenomena as largely independent of biological processes (mind– body dualism). The social ecological model expands the traditional public health model to incorporate aspects of the social environment as fundamental contributors to health problems. It is similar to the biopsychosocial model of illness in that it emphasizes the role of extrasomatic factors, but it differs in its incorporation of social structural and political factors such as health policy, income inequality, racism, and access to care. For this reason, the social ecology model has been more central to public health practice, while the biopsychosocial model has been applied more often to individual health and illness behavior, such as the doctor–patient relationship, and compliance with medical treatment (Ramalingaswami, 1986).
A number of formulations of the social ecology model have been developed. They all have in common the notion of multilevel systems of mutual influence and interaction, moving from the individual level through linkages to larger social networks, including the family, community, social institutions, the state, and global systems. Key concepts include system integration, change, and adaptation over time (Richard et al., 1996). One formulation of the model that has gained prominence is that developed by McLeroy and colleagues for application to health promotion (McLeroy et al., 1988). This model is organized around five hierarchical levels of influence: (1) intrapersonal factors; (2) interpersonal processes and primary groups; (3) institutional factors; (4) community factors; and (5) public policy. It has been widely applied to the study of diverse health topics, including physical activity, drug use, adolescent pregnancy, infant feeding, cancer, and heart disease.
Health Promotion
As noted previously, social psychological models have figured prominently in approaches to health promotion. These models seek to identify determinants and pathways of influence for health-related behaviors such as diet and exercise, smoking, safe sex practices, contraceptive use, and screening behavior. Most important among these were the theory of reasoned action, later modified as the theory of planned behavior (Ajzen, 2002), social learning theory/social cognitive theory (Bandura, 2001), and the transtheoretical model based on the stages of change construct (Prochaska et al., 1992). What the various models have in common is the focus on individual behavior change to improve health through the adoption of health-enhancing practices such as smoking cessation, contraceptive use, and mammography screening. A key construct that emerged through various applications and elaborations of these models is the notion of self-efficacy, the degree to which an individual feels competent to perform a health practice. Originally proposed as part of social learning theory (Bandura, 1977), the construct proved to be a strong predictor of behavior that required sustained lifestyle change. Thus this notion was incorporated into the expanded health belief model, the theory of planned behavior (recast as ‘perceived behavioral capability’), and the transtheoretical model.
Interpretive Studies
Several strands of theoretical development across disciplines can be subsumed under the interpretive studies rubric. In anthropology, it includes cognitive approaches to illness such as Kleinman’s explanatory model framework (Kleinman, 1978) and cultural consensus analysis (Romney et al., 1986). Related sociological perspectives include social constructionism (Berger and Luckmann, 1967) and symbolic interactionism (Blumer, 1969). In psychology, relevant examples include cognitive models of illness such as Levanthal’s parallel process model (Brissette et al., 2003), the notion of illness representations, and attribution theory for explaining beliefs about illness causation. The common denominator of these approaches is a focus on subjective, perceptual, and cognitive dimensions of illness. It is assumed that meanings are neither ‘correct’ nor fixed but are constructed or negotiated through cognitive, social, and cultural filtering. Anthropological distinctions between the concepts of emic and etic and illness and disease are relevant here. ‘Emic’ refers to the insider’s view (e.g., the patient’s subjective experience of illness) and ‘etic’ to the objective view of outsiders (e.g., the health-care provider’s and biomedical understanding). Similarly, ‘illness’ designates the individual’s subjective experience of feeling sick, including the psychosocial aspects, while ‘disease’ refers to the physiological pathology of the episode.
Critical Perspectives
Critical perspectives are those that challenge the dominant paradigms of public health practice and argue for alternative approaches to improving the health of populations. They can be grouped into at least two general categories, those that fault the political economic organization of health systems, and those influenced by postmodern thinking about the role of the state and regulatory practices in producing healthy citizens. The first school of critical theory has historical roots in Marxist theory, critiques of capitalism, and the emergence of the medical–industrial complex. This tradition traces the causes of health inequalities to broad social structural arrangements, such as global systems of trade and neocolonial domination of less developed countries by economic power elites. Likewise, health disparities are attributed to the deleterious effects of the market economy on health issues. Examples include critiques of the disproportionate distribution of the global burden of disease across different regions of the world. Ethical critiques about unequal availability of life-saving drugs would also fit into this category. An example within the United States would be the explanation of health inequalities across racial and ethnic groups in terms of economic structures, racism, and discrimination. Feminist perspectives on the health status of women would also fall within this genre.
The second category of critical perspectives emerged more recently within the poststructuralist theoretical paradigm that analyzes social problems from a constructivist perspective, giving primacy to how we frame healthrelated issues, and how this leads to various control strategies. For example, in modern industrial societies the state has assumed an increasingly larger role in health surveillance and monitoring, constantly urging the populace to adopt healthy lifestyles and conform to the regimes of a healthy citizenship (Petersen and Lupton, 1996) in the pursuit of ‘‘perfect health’’ (Hours, 2001a, 2001b). Threats to public health are constructed as emanating from the unhealthy ‘other,’ such as immigrant groups, and ‘risks’ are seen as ubiquitous and constant, so citizens must remain continually vigilant. The latter tradition includes critiques of the ‘risk factor’ approach to public health thinking as a misguided oversimplification of problems that produces a false sense of security and control.
Critical theorists have been particularly critical of ecological models for accepting as a given the social environmental context of health and the unequal distribution of resources across groups. In an attempt to integrate critical and ecological perspectives, some theorists have developed synthetic models that incorporate aspects of both traditions. For example, the ecosocial model (Krieger, 1994) attempts to link a social production of disease perspective with the multilevel framework of social ecology. It focuses on patterns of inequalities in health across the ecological levels of biological processes, the individual, family systems, community, populations, society, and global systems. It also incorporates the notion of embodiment, that is, how social inequalities are expressed through biological processes. Others have advocated for the development of similar synthetic models, along the lines of a ‘‘critical ecological perspective’’ (Leatherman, 2005).
Key Concepts
Knowledge And Attitudes
In terms of sheer volume, the bulk of social science research and practice has centered on cognitive factors related to health and illness. There are a number of reasons for this. First, the most accessible, simplest, and least costly variables to measure are cognitive; perceptions, attributions, attitudes, and knowledge can be studied through survey and interview techniques. Second, until recently, the prevailing paradigm for social research assumed that the most important obstacles to program success resided in the minds and dispositions of the target audience. Hence, the goal was to uncover faulty understandings so that correct information could be provided, thereby leading to more enlightened behavior. Third, psychological theories have strongly influenced research in this field, and anthropological approaches have also emphasized cultural beliefs as central. The combination of these influences has created a huge body of literature on cognitive factors in health. Some of the key concepts have been previously touched upon, such as basic health beliefs and attitudes, explanatory models of illness, and illness representations. Related concepts that have received particular attention include locus of control (e.g., internal vs. external to the individual), self-efficacy (perceived ability to successfully execute), expectancies (anticipated outcomes), and intentions (anticipated action). However, along with the volume of research on cognitive factors has come the recognition that beliefs often do not lead to behavior, and that it is necessary to study behavior itself and its varied influences.
Health Behavior
The dominance of health behavior models for health promotion has contributed quite a few concepts and methods for the tool kit of the behavioral scientist. To begin with, considerable attention has been accorded to the development of reliable and valid measures of specific health behaviors, such as use of alcohol, tobacco, and drugs, injury prevention practices, food consumption, physical activity and sexual behavior. Likewise, precision has been introduced for measuring frequency, intensity, salience, and other dimensions. Health behavior has also been conceptualized according to different stages, such as initiation, maintenance, and relapse, as well as positive versus negative behavior concepts such as adoption or acceptance versus cessation or refusal. The field of health behavior research has incorporated principles and techniques of testing and measurement to a notable degree, and it is common for researchers to use standardized instruments, structured scales, quantitative indices, and similar tools. In addition, many analyses use secondary data sources such as the U.S. National Behavioral Risk Factor Surveillance Survey conducted annually by the CDC, as well as numerous specialized periodic surveys sponsored by the National Center for Health Statistics. The reliance on specific indicators has come to be described as the ‘risk factor approach’ to health behavior. Even when study designs include higher-level influences, such as social structural and cultural variables, the focus is on ‘predicting’ specific health behaviors by showing a statistical association with structural risk factors. This orientation is favored among researchers from a social psychological and health education background. In contrast, anthropological and sociological research accords greater attention to understanding the sociocultural context in and of itself.
Culture
Despite claiming culture as its central concept, medical anthropology has developed few specialized cultural concepts for studying health. There is a pervasive resistance to systematizing anthropological approaches either theoretically or methodologically; instead, researchers tend to approach their topics purely descriptively and without preconceived notions of defined variables. While the research is usually guided by an explicit theoretical orientation, such as ‘constructivist,’ ‘symbolic,’ or ‘interpretive,’ it is rare to find standardized measures or operational constructs used in the traditional sense of quantitative social science. Many would argue that it is precisely these characteristics of anthropological studies that serve as their greatest strength, and that qualitative, narrative research should ideally remain purely descriptive. On the other hand, the lack of systematization makes it difficult for other health scientists to ‘grasp’ what anthropological studies are about, and has limited the influence of anthropology in public health. Nevertheless, a few key concepts have gained attention and practical utility. The distinction between disease and illness remains relevant, with ‘disease’ referring to the physiological pathology associated with a biomedically defined diagnosis and ‘illness’ describing the complex biopsychosocial experience of feeling sick or unwell. Related concepts include the emic (illness) and etic (disease) distinction previously described. Explanatory models of illness focus on emic perceptions of the causes, consequences, and appropriate treatment for specific illness episodes. Cultural models of illness refer to shared understandings, or shared explanatory models, for locally recognized illness categories.
Methodological development in studying cultural dimensions of illness includes two quantitative approaches with strong epidemiologic orientations. The first is cultural consensus analysis, a technique for measuring the degree to which a set of cultural beliefs are shared within a social group (Weller and Baer, 2002). A related concept is cultural consonance, or the extent to which an individual, in his or her own behavior and lifestyle, conforms to the shared cultural model. The second quantitative approach, referred to as cultural epidemiology (Weiss, 2001), follows a systematic methodology for the comparative study of explanatory models across social groups. It integrates quantitative and qualitative data in describing operationally defined illness experience, meaning, and behavior.
Social Environment
A large body of literature has accumulated related to social environmental factors and health, including the effects of social stress, social support, social networks, and social capital. Beginning in the 1970s, researchers took a serious interest in the health effects of stress, and over the decades the weight of evidence has shown conclusively that stress affects not only chronic disease but almost every health condition imaginable. Early studies of stress investigated the impact of major life events such as bereavement, divorce, and job loss on morbidity and mortality (Lazuras and Folkman, 1984). Subsequent studies expanded this line of inquiry to include ‘daily hassles,’ job-related stress, and other more day-to-day kinds of stress, developing various instruments to measure the varieties of stress. Concomitantly, researchers also began to investigate the health-protective benefits of social support and social networks (Berkman et al., 2000). Often studies of social support investigated its mitigating effects on the impact of stress, developing alternative hypotheses about whether social support operated as an independent, mediating, or moderating variable. The literature on social support identifies at least four major types of support – emotional, instrumental, informational, and appraisal. Other related concepts include direct and indirect support, and formal and informal support. Studies have attempted to identify the variable impact of different kinds of support on particular health outcomes.
A related line of research focuses on the concept of social networks, the connections people have through relationships with others, and develops various measures of social integration and isolation, including network structure (size, density, and dispersion of linkages), and the relational content of support such as sources, types of demands, conflicts, role expectations, and social regulation of behavior. An important milestone study in this genre came out of the previously mentioned Alameda County Study, which documented prospectively the significant positive impact of social connectedness (Berkman and Syme, 1979; House et al., 1982). Similar findings have been documented in other studies in the United States and Europe. More complex research designs have further documented the differential impact that social support has on subgroups in the population, such as comparing men and women, and rural and urban dwellers. As the health effects of social support became well-established, researchers shifted their attention to better understanding the biopsychosocial processes that mediate the association with health.
In recent years, social epidemiologic studies have focused on the concepts of social capital and collective efficacy as explanatory variables in population-level health. Growing out of a renewed interest in the influence of neighborhoods on health conditions, researchers have investigated how shared norms, mutual trust, and reciprocal obligations (social capital) influence diverse health outcomes, including crime and mortality rates (Kawachi and Berkman, 2003). ‘Collective efficacy’ refers to a group’s perceived ability to successfully take action for the benefit of the common good (e.g., crime prevention). Studies have associated collective efficacy with lower rates of violence, for example (Sampson, 2003). However, the ability to achieve common goals is also dependent on the wider political environment, or institutional capacity through linkages among organizations within and outside the focal community.
Methodologic Approaches
The social and behavioral sciences have made significant contributions to public health through important methodologic advances in our ability to study and predict complex health processes and outcomes. Advances in both quantitative and qualitative techniques offer more powerful tools for studying the multifactorial and multilevel determinants of health. Although traditionally public health has favored statistical approaches to data analysis, qualitative methods including ethnographic and narrative techniques have gained prominence, and mixed method designs are increasingly recognized as offering the most robust research strategies. In addition, participatory methods that involve members of the target community in research design and implementation have expanded in community-based health research. Multimethod rapid assessment procedures emerged in the 1980s (Scrimshaw and Hurtado, 1987) as a way to combine the strengths of social science methods with the pragmatic needs of program planners.
Epidemiologic methods for designing population surveys and analyzing large data sets have grown more sophisticated over the decades. Techniques for multivariate analysis have been refined along with new methods of multilevel modeling, which enable the application of complex ecological designs. Advances in the design of cross-sectional surveys, sampling strategies, measurement of, and refinement of techniques for assessing the reliability and validity of data-collection instruments have figured importantly. On the qualitative side, techniques for studying cognitive, emotional, and subjective phenomena have experienced rapid development in recent decades, with numerous methodologic resources published to guide researchers and train students. In particular, the use of in-depth interviews, focus group discussions, participant observation, and textual analysis have become increasingly popular. Examples of participatory methods include the use of community advisory boards, coalition building among stakeholder groups, training lay persons as research assistants, and building in continual feedback and involvement of constituents.
Intervention Strategies
Community-Based Health Promotion
Social scientists have played an important role in the development of interventions based on community development and empowerment models of social change. Community-based approaches date back to the mid-twentieth century with the involvement of anthropologists and sociologists in projects aimed at modernization of traditional communities in both developing and industrializing countries. Many of these projects included health and nutrition improvement goals as it became obvious that widespread urbanization, industrialization, and Westernization often entailed undesirable health related consequences. Deleterious lifestyles and diet often replaced more salubrious traditional systems; thus, the goal of the early interventions was to introduce modern medical practices such as water boiling, immunization, and antibiotic treatment without disrupting desirable traditional practices such as breast-feeding and locally grown food systems. The community development model received a significant boost through the Alma Ata Declaration of 1978 (WHO and UNICEF, 1978), which advocated for basic health services at the community level, with heavy reliance on local resources and participation. Anthropologists and indigenous social scientists joined multidisciplinary teams to help implement community health programs throughout the world in the latter part of the twentieth century.
Although the community development model evolved primarily in the context of rural populations, it has been successfully adapted to urban settings as well. Widespread urbanization throughout the world, along with dramatic population shifts to cities, have created new communities of need. Beginning with the community empowerment movement of the 1960s, local citizens have been increasingly integrated in health promotion programs. Community-based interventions have addressed diverse public health issues such as infant mortality, homelessness, cardiovascular disease, HIV/AIDS, teen pregnancy, and mental health. Particular attention has been given to community-based interventions to reduce coronary heart disease, such as the North Karelia Project of Finland and the Almeda County Study of California. Key principles of community development approaches include community control and ownership, community empowerment, multisectoral activities, and meaningful participation by affected groups. Because of the complexity of the process and the attendant political issues arising from diverse stakeholder interests, there are many challenges to successful implementation of community-based interventions. To help plan such comprehensive programs and anticipate challenges, organized models for community intervention have been developed to guide the process, such as the Planned Approach to Community Health (PATCH) developed by the U.S. Centers for Disease Control and Prevention and the PRECEDE/PROCEED model for intervention design and evaluation.
Policy And Advocacy
One of the least developed traditions of social science applications in public health has been the policy and advocacy arena. Historically, the field has been preoccupied with less political aims, such as modifying the delivery of health services, mobilizing communities, and changing individual behavior. That is not to say that policy and advocacy-oriented research and practice have been missing altogether (e.g., Justice, 1986; Gray and O’Leary, 2000; Whiteford and Manderson, 2000). While it is commonplace for researchers to address the ‘policy implications’ of their findings, designing projects with primary emphasis on the policy process itself is less common. However, researchers are increasingly adopting policy-focused agendas and designing advocacy-oriented interventions that utilize the tools of political action, and are building community coalitions and multisectoral partnerships, lobbying for legislative and regulatory initiatives, and related work (Couto, 1998; Foster-Fishman et al., 2001). Prominent scholars such as anthropologistphysician Paul Farmer (1999) have taken vocal leadership and advocacy positions that challenge the status quo and call for new solutions to global health inequalities. Social scientists are developing new theoretical models and methods for this action arena (McLeroy et al., 1994), and training of public health students is increasingly incorporating competencies related to this approach. In recent years, social scientists working in the field of bioethics have also been actively engaged in addressing critical concerns in public health, calling attention to cultural and structural factors underlying ethical practices in clinical and biomedical research settings throughout the world (Marshall and Koenig, 2004).
Social Marketing
The newest approach to health promotion that has gained increasing acceptance is social marketing, which applies the technologies of commercial marketing to the study, planning, implementation, and evaluation of programs aimed at influencing target audiences to adopt healthy behaviors and take positive social action (Andreasen, 1995). Social marketing programs use the four ‘P’s’ of marketing – product, price, place, and promotion – to encourage adoption of socially beneficial behavior. Grounded in consumer research, the approach relies heavily on in-depth understanding of the target audience and its perceived needs and goals to design appropriate strategies for intervention. Finally, audience segmentation and identification of priority groups is a key component of strategy design (Grier and Bryant, 2005). The application of social marketing in public health first emerged in the international arena in the 1970s as new methods for encouraging the use of contraception were sought. It gained in popularity during the child survival program era of international health activity in the 1980s, particularly through the promotion of oral rehydration therapy. By the 1990s it had surfaced in domestic programs of industrial countries, particularly the United States and Scotland, and has grown steadily as a strategy for promoting a variety of health-enhancing practices such as breast-feeding, healthy diets, physical activity, and safer sex practices.
Primary, Secondary, And Tertiary Prevention
One of the ways in which public health is often contrasted with clinical medicine is the degree to which it focuses on prevention of disease and disability, while medical practice emphasizes the treatment of health problems after they occur. It is commonplace in public health to further distinguish among primary, secondary, and tertiary prevention. In primary prevention, the focus is on activities that forestall the development of pathological conditions. For example, preventing the onset of heart disease through healthy lifestyle behavior fall into this category. Secondary prevention, on the other hand, refers to detection of disease or its precursors at an early stage in order to take ameliorative action that can thwart full development or enable measures to keep the problem in check. Regular screening for detectable conditions such as hypertension, breast and colorectal cancer, diabetes, and sexually transmitted infections fall into this category. Finally, tertiary prevention includes interventions at later stages of disease to prevent secondary complications, sustain optimal disease management, and ensure the best quality of life. Treatment for hypertension, diabetes, depression, osteoporosis, lymphedema, and other chronic conditions illustrate the third category of prevention. Social and behavioral factors figure importantly in all three types of prevention; however, over the decades, interest has grown particularly in their potential contribution to primary prevention. Health economists have demonstrated that it is far more cost-effective to prevent conditions before they develop than to provide long-term care for chronic conditions. The cost factor is particularly salient as more people live to advanced age and governments are mandated to ensure the provision of care. There is also the desire for people to live healthy, productive lives for as long as possible.
Of all the public health disciplines, the social and behavioral sciences can make unique contributions to primary prevention. Influencing lifestyle patterns and the social context in which people live is fundamental to prevention of the major health conditions facing society today. It also poses one of the greatest challenges, because the force of macro-level influences on individual behavior is tremendous. One need only consider the facts of the contemporary way of life, such as sedentary daily routines, people spending many hours of the day in front of computers, increasing reliance on processed and ‘fast’ food, and the tendency toward workaholism, lack of sleep and chronic stress, to appreciate the obstacles facing such programs. It is a basic tenet of intervention that it is far easier to modify the more proximate determinants of health, such as individual food choices, than it is to alter the intermediate and distal forces that affect those choices. Changing the organization of society and the core components of culture poses enormous challenge, yet there is growing recognition that only through alteration of the fundamental causes of disease (e.g., inadequate income and access to health care, unemployment, racial and gender discrimination, lack of social support, stressful work settings, failure to provide educational opportunities) can true primary prevention be realized (Link and Phelan, 1995).
Future Directions
In the decades ahead, further developments will undoubtedly unfold in the theoretical, methodologic, and practical applications of social science within public health. These will expand not only in the areas outlined above, but will take new directions as well. One area of expected growth is critical analysis of public health as a terrain for social policy and action. Similar to the distinction often made between sociology of medicine and sociology in medicine, social scientists will augment their traditional positionality within public health to adopt more outsider gazes that analyze the diverse practices of public health, with the goal of highlighting the consequences of taken-for-granted approaches and perspectives. In addition to elaborating the cultural context of populations served, anthropologists will turn their attention to the organizational culture of public health, illuminating the consequences of collective identities, value orientations, epistemologic assumptions, and the social construction of problems, causality, and modes of intervention. Another thrust will likely expand critical perspectives linking issues of social justice, ethics, and health disparities. Social scientists will move beyond measurement, description, and analysis of health inequalities to advocate agendas for directed change utilizing social theory and methods. These actions will be directed at local, national, and global levels, drawing upon strategies honed in other practice domains as well as producing innovative approaches. The inherent tension in negotiating a balanced interface between insider and outsider perspectives will hopefully produce a rich body of work that further enhances social science contributions to public health.
Bibliography:
- Ajzen I (2002) Perceived behavioral control, self-efficacy, locus of control, and the theory of planned behavior. Journal of Applied Social Psychology 32: 665–683.
- Andreasen A (1995) Marketing Social Change: Changing Behavior to Promote Health, Social Development and the Environment. San Francisco, CA: Jossey-Bass.
- Bandura A (1977) Social Learning Theory. New York: General Learning Press.
- Bandura A (2001) Social cognitive theory: An agentive perspective. Annual Review of Psychology 52: 1–26.
- Barnes DS (1995) The Making of a Social Disease: Tuberculosis in Nineteenth-Century France. Berkeley, CA: University of California Press.
- Benoist J and Desclaux A (1995) Sida et anthropologie: bilan et perspectives. Paris, France: Karthala.
- Berger PL and Luckmann T (1967) The Social Construction of Reality. New York: Anchor.
- Berkman L and Syme SL (1979) Social networks, host resistance, and mortality: A year follow-up study of Alameda Country residents. American Journal of Epidemiology 109: 186–204.
- Berkman L, Glass T, and Brisette I (2000) From social integration to health: Durkheim in the new millennium. Social Science and Medicine 51(6): 843–857.
- Blumer H (1969) Symbolic Interactionism: Perspective and Method. Berkeley, CA: University of California Press.
- Brissette I, Levanthal E, and Levanthal H (2003) The common-sense model of self-regulation of health and illness. In: Cameron LD and Levanthal H (eds.) The Self-Regulation of Health and Illness, pp. 42–65. London: Routledge.
- Coreil J (1990) The evolution of anthropology in international health. In: Coreil J and Mull D (eds.) Anthropology and Primary Health Care, pp. 3–27. Boulder, CO: Westview Press.
- Coreil J, Bryant CA, and Henderson JN (2001) Social and Behavioral Foundations of Public Health. Thousand Oaks, CA: Sage.
- Couto R (1998) Community coalitions and grassroots policies of empowerment. Administration and Society 30(5): 569–594.
- Farmer P (1999) Infections and Inequalities: The Modern Plagues. Berkeley, CA: University of California Press.
- Firth R (1934) The sociological study of native diet. Africa 7: 401–414.
- Foster-Fishman P, Berkowitz D, Lounsbury D, Jacobson S, and Allen N (2001) Building collaborative capacity in community coalitions: A review and integrative framework. American Journal of Community Psychology 29(2): 241–261.
- Gray BH and O’Leary J (2000) The evolving relationship between medical sociology and health policy. In: Bird CE, Conrad P and Fremont AM (eds.) Handbook of Medical Sociology, 5th edn., pp. 258–269. Upper Saddle River, NJ: Prentice Hall.
- Grier S and Bryant CA (2005) Social marketing in public health. Annual Review of Public Health 26: 319–339.
- Hours B (ed.) (2001a) Pour une anthropologie de la sante´ et socie´ te´ s. In: Hours B (ed.) (2001a) Syste`mes et politiques de sante´: De la sante´ publique a` l’anthropologie, pp. 5–21. Paris, France: Karthala.
- Hours B (2001b) Syste`mes et politiques de sante´: De la sante´ publique a` l’anthropologie. Paris, France: Karthala.
- House JS, Robbins C, and Metzner HM (1982) The association of social relationships and activities with mortality: Prospective evidence from the Tecumseh Community Health Study. American Journal of Epidemiology 116: 123–140.
- Janes CR, Stall R, and Gifford SM (1986) Anthropology and Epidemiology. Dort, Netherlands: Reidel.
- Janz NK, Champion VL, and Strecher VJ (2002) The health belief model. In: Glanz K, Rimer BK and Lewis FM (eds.) Health Behavior and Health Education: Theory, Research, and Practice, pp. 45–66. San Francisco, CA: Jossey-Bass.
- Justice J (1986) Policies, Plans and People: Culture and Health Development in Nepal. Berkeley, CA: University of California Press.
- Kawachi I and Berkman LF (eds.) (2003) Neighborhoods and Health. New York: Oxford University Press.
- Kleinman A (1978) Patients and Healers in the Context of Culture: An Exploration of the Borderland between Anthropology, Medicine, and Psychiatry. Berkeley, CA: University of California Press.
- Krieger N (1994) Epidemiology and the web of causation: Has anyone seen the spider: Social Science & Medicine 39: 887–903.
- Lazarus RS and Folkman S (1984) Stress, Appraisal, and Coping. New York: Springer.
- Leatherman T (2005) A space of vulnerability in poverty and health: Political-ecology and biocultural analysis. Ethos 33(1): 46–70.
- Link BG and Phelan J (1995) Social conditions as fundamental causes of disease. Journal of Health and Social Behavior 47: 80–94.
- Malinowski B (1945) The Dynamics of Culture Change: An Inquiry into Race Relations in Africa. New Haven: Yale University Press.
- Marshall P and Koenig B (2004) Accounting for culture in a globalized bioethics. Journal of Law, Medicine and Ethics 32(2): 252–256.
- McLeroy KR, Bibeau D, Steckler A, and Glanz K (1988) An ecological perspective on health promotion programs. Health Education Quarterly 15(4): 351–377.
- McLeroy KR, Kegler M, Steckler A, Burdine JM, and Wisotzky M (1994) Community coalitions for health promotion: Summary and further reflections. Health Education Research 9(1): 1–11.
- National Institutes of Health (2001) Executive summary. In: Toward higher levels of analysis: Progress and promise in research on social and cultural dimensions of health. Report of the National Institutes of Health. NIH Publication No. 01-5020. Washington, DC: National Institute of Health.
- Paul B (1955) Health, Culture and Community: Case Studies of Public Reactions to Health Programs. New York: Russell Sage.
- Paul B (1956) Social science and public health. American Journal of Public Health 46(11): 1389–1396.
- Petersen A and Lupton D (1996) The New Public Health: Health and Self in the Age of Risk. Thousand Oaks, CA: Sage.
- Prochaska JO, DiClemente CC, and Norcross JC (1992) In search of how people change. American Psychologist 47: 1102–1114.
- Putnam RD (2000) Bowling Alone: The Collapse and Revival of American Community. New York: Simon and Schuster.
- Ramalingaswami V (1986) The art of the possible. Social Science and Medicine 22(11): 1097–1103.
- Richard L, Potvin L, Kishchuk N, Prlic H, and Green LW (1996) Assessment of the integration of the ecological approach in health promotion programs. American Journal of Health Promotion 10(4): 318–328.
- Richards A (1939) Land, Labour and Diet in Northern Rhodesia: An Economic Study of the Bemba Tribe. London: Oxford University Press.
- Romney AK, Weller SC, and Batchelder WH (1986) Culture as consensus: A theory of cultural and informant accuracy. American Anthropologist 88: 313–339.
- Rushing WA (1995) The AIDS Epidemic: Social Dimensions of an Infectious Disease. Boulder, CO: Westview.
- Saillant F and Genest S (2007) Medical Anthropology: Regional Perspectives and Shared Concerns. Malden, MA: Blackwell.
- Sampson RJ (2003) Neighborhood-level context and health: Lessons from sociology. In: Kawachi I and Berkman LF (eds.) Neighborhoods and Health, pp. 132–146. New York: Oxford University Press.
- Schneiderman N, Speers MA, Silva JM, Tomes H, and Gentry JH (2001) Integrating Behavioral and Social Sciences with Public Health. Washington, DC: American Psychological Association.
- Scrimshaw S and Hurtado E (1987) Rapid Assessment Procedures for Nutrition and Primary Health Care. Los Angeles: UCLA Latin American Center Publications.
- Taylor S (2006) Health Psychology, 6th edn. New York: McGraw-Hill.
- Turshen M (1989) The Politics of Public Health. New Brunswick, NJ: Rutgers University Press.
- Weiss MG (2001) Cultural epidemiology: An introduction and overview. Anthropology and Medicine 8(1): 5–29.
- Weller S and Baer R (2002) Measuring withinand between-group agreement: Identifying the proportion of shared and unique beliefs across samples. Field Methods 14(1): 6–25.
- Whiteford L and Manderson L (2000) Global Health Policy, Local Realities: The Fallacy of the Level Playing Field. Boulder, CO: Lynne Rienner.
- WHO and UNICEF (1978) Primary Health Care: Report of the International Conference on Primary Health Care. Alma-Ata, USSR, 6–12 September.
- Becker MH (ed.) (1974) The health belief model and personal health behavior. Health Education Monographs 2: .
- Bird CE, Conrad P, and Fremont AM (eds.) (2000) Handbook of Medical Sociology, 5th edn. Upper Saddle River, NJ: Prentice Hall.
- WHO (1995) The Ottawa Charter for Health Promotion. First International Conference on Health Promotion, Canada, 21 November 21.




