Sample Disorders of Childhood and Adolescence Research Paper. Browse other research paper examples and check the list of research paper topics for more inspiration. iResearchNet offers academic assignment help for students all over the world: writing from scratch, editing, proofreading, problem solving, from essays to dissertations, from humanities to STEM. We offer full confidentiality, safe payment, originality, and money-back guarantee. Secure your academic success with our risk-free services.
From the time that modern views of mental illness emerged in the late eighteenth and early nineteenth centuries, significantly less attention has been given to mental health problems in children than it has to problems in adults (Rie, 1971). Even today there are far fewer categories for diagnosing mental disorders in children, and these categories vary in their sensitivity to developmental parameters and context. Current knowledge of child and adolescent disorders is compromised by a lack of child-specific theories, by an unsystematic approach to research (Kazdin, 2001), and by the inherent conceptual and research complexities (Kazdin & Kagan, 1994), which may explain why there are far fewer empirically supported treatments for children than for adults (Chambless & Ollendick, 2001). Despite these caveats, tremendous advances have been made over the last decade (Mash & Barkley, 1996; Mash & Wolfe, 2002; Rutter & Sroufe, 2000).
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
New conceptual frameworks, new knowledge, and new research methods have greatly enhanced our understanding of childhood disorders (Cicchetti & Cohen, 1995; Sameroff, Lewis, & Miller, 2000) as well as our ability to assess and treat children with these problems (Mash & Barkley, 1998; Mash & Terdal, 1997b).
We begin with a discussion of the significance of children’s mental health problems and the role of multiple interacting influences in shaping adaptive and maladaptive patterns of behavior. Next we provide a brief overview of disorders of childhood and adolescence and related conditions as defined by current diagnostic systems (American Psychiatric Association;APA, 2000). We then consider two common categories of problems in children and adolescents: externalizing disorders (disruptive behavior disorders; attention-deficit/ hyperactivity disorder, ADHD), and internalizing disorders (mood disorders, anxiety disorders). We illustrate current issues and approaches to child and adolescent disorders by focusing on ADHD and anxiety disorders as examples. In doing so we consider the main characteristics, epidemiology, developmental course, associated features, proposed causes, and an integrative developmental pathway model for each of these disorders. We conclude with a discussion of current issues and future directions for the field.
The Significance of Children’s Mental Health Problems
Long-overdue concern for the mental health of children and adolescents is gradually coming to the forefront of the political agenda. For example, in the United States the new millennium witnessed White House meetings on mental health in young people and on the use of psychotropic medications with children. ASurgeon General’s Conference on Children’s Mental Health resulted in an extensive report and recommendations (U.S. Public Health Service, 2001a), closely followed by a similar report on youth violence (U.S. Public Health Service, 2001b). Increasingly, researchers in the fields of clinical child psychology, child psychiatry, and developmental psychopathology are becoming attentive to the social policy implications of their work and in effecting improvements in the identification of and services for youth with mental health needs (Cicchetti & Toth, 2000; Weisz, 2000c). Greater recognition is also being given to factors that contribute to children’s successful mental functioning, personal well-being, productive activities, fulfilling relationships, and ability to adapt to change and cope with adversity (U.S. Department of Health and Human Services, 2000; U.S. Public Health Service, 2001a).
The increase in attention to children’s mental health problems derives from a number of sources. First, many young people experience significant mental health problems that interfere with normal development and functioning. As many as one in five children in the United States experience some type of difficulty (Costello & Angold, 2000; Roberts, Attkisson, & Rosenblatt, 1998), and 1 in 10 have a diagnosable disorder that causes some level of impairment (B. J. Burns et al., 1995; Shaffer et al., 1996). These numbers likely underestimate the magnitude of the problem because they do not include a substantial number of children who manifest subclinical or undiagnosed disturbances that may place them at high risk for the later development of more severe clinical problems (McDermott & Weiss, 1995).
Moreover, the frequency of certain childhood disorders— such as antisocial behavior and some types of depression—may be increasing as the result of societal changes and conditions that create growing risks for children (Kovacs, 1997). Among these conditions are chronic poverty, family breakup, single parenting, child abuse, homelessness, problems of the rural poor, adjustment problems of immigrant and minority children, and the impact of HIV, cocaine, and alcohol on children’s growth and development (Duncan, Brooks-Gunn, & Klebanov, 1994; McCall & Groark, 2000). Evidence gathered by the World Health Organization suggests that by the year 2020, childhood neuropsychiatric disorders will rise proportionately by over 50% internationally—to become one of the five most common causes of morbidity, mortality, and disability among children (U.S. Public Health Service, 2001a).
For a majority of children who experience mental health problems, these problems go unidentified—only about 20% receive help, a statistic that has not changed for some time (B. J. Burns et al., 1995). Even when children are identified and receive help for their problems, this help may be less than optimal. For example, only about half of children with identified ADHD seen in real-world practice settings receive care that conforms to recommended treatment guidelines (Hoagwood, Kelleher, Feil, & Comer, 2000). The fact that so few children receive appropriate help is probably related to such factors as inaccessibility, cost, parental dissatisfaction with services, and the stigmatization and exclusion often experienced by children with mental disorders and their families (Hinshaw & Cicchetti, 2000).
Unfortunately, children with mental health problems who go unidentified and unassisted often end up in the criminal justice or mental health systems as young adults (Loeber & Farrington, 2000). They are at a much greater risk for dropping out of school and for not being fully functional members of society in adulthood, which adds further to the costs of childhood disorders in terms of human suffering and financial burdens. For example, average costs of medical care for youngsters with ADHD are estimated to be double those for youngsters without ADHD (Leibson, Katusic, Barberesi, Ransom, & O’Brien, 2001). Moreover, allowing just one youth to leave high school for a life of crime and drug abuse is estimated to cost society from $1.7 to $2.3 million (Cohen, 1998).
Understanding Disorders of Childhood and Adolescence
Much of what we know about disorders of childhood and adolescence is based on findings obtained at a single point in the child’s development and in a single context. Although it is useful, such information is incomplete because it fails to capture dynamic changes in the expression and causal factors that characterize most forms of child psychopathology. Only in the last two decades have efforts to describe and explain psychopathology in children included longitudinal methods and conceptual models that are sensitive to developmental change and the sociocultural context (Cicchetti & Aber, 1998; Boyce et al., 1998; García Coll, Akerman, & Cicchetti, 2000).
The study of child psychopathology is further complicated by the fact that most childhood disorders do not present in neat packages, but rather overlap, co-exist, or both with other disorders. For example, symptoms of anxiety and depression in childhood are highly correlated (Brady & Kendall, 1992; Compas & Oppedisano, 2000), and there is also much overlap among emotional and behavioral disorders, child maltreatment, substance abuse, delinquency, and learning difficulties (e.g., Greenbaum, Prange, Friedman, & Silver, 1991). Many behavioral and emotional disturbances in children are also associated with specific physical symptoms, medical conditions, or both.
Furthermore, few childhood disorders can be attributed to a single cause. Although some rare disorders such as phenylketonuria (PKU) or Fragile X mental retardation may be caused by a single gene, current models in behavioral genetics recognize that more common and complex disorders are the result of multigene systems containing varying effect sizes (Plomin, 1995). Most childhood disorders are the result of multiple and interacting risk and protective factors, causal events, and processes (e.g., Ge, Conger, Lorenz, Shanahan, & Elder, 1995). Contextual factors such as the child’s family, school, community, and culture exert considerable influence, one that is almost always equivalent to or greater than those factors usually thought of as residing within the child (Rutter, 2000b).
Like adult disorders, causes of child psychopathology are multifaceted and interactive. Prominent contributing causes include genetic influences, neurobiological dysfunction, difficult infant temperament, insecure child-parent attachments, problems in emotion regulation or impulse control, maladaptive patterns of parenting, social-cognitive deficits, parental psychopathology, marital discord, and limited family resources, among others. The causes and outcomes of child psychopathology operate in dynamic and interactive ways across time and are not easy to disentangle. The designation of a specific factor as a cause or an outcome of child psychopathology usually reflects the point in an ongoing developmental process that the child is observed and the perspective of the observer. For example, a language deficit may be viewed as a disorder (e.g., mixed receptiveexpressive language disorder), the cause of other problems (e.g., impulsivity), or the result of some other condition or disorder (e.g., autism). In addition, biological and environmental determinants interact at all periods of development. For example, the characteristic styles used by parents in responding to their infants’ emotional expressions may influence the manner in which patterns of cortical mappings and connections within the limbic system are established during infancy (Dawson, Hessl, & Frey, 1994). Thus, early experiences may shape neural structure and function, which may then create dispositions that direct and shape the child’s later experiences (Dawson,Ashman, & Carver, 2000).
The experience and the expression of psychopathology in children are known to have cognitive, affective, physiological, and behavioral components; consequently, many different descriptions and definitions of abnormality in children have been proposed (Achenbach, 2000). However, a central theme in defining disorders of childhood and adolescence is adaptational failure in one or more of these components or in the ways in which these components are integrated and organized (Garber, 1984; Mash & Dozois, 1996). Adaptational failure may involve a deviation from age-appropriate norms, an exaggeration or diminishment of normal developmental expressions, interference in normal developmental progress, a failure to master age-salient developmental tasks, a failure to develop a specific function or regulatory mechanism, or any combination of these (Loeber, 1991).
Numerous etiological models have been proposed to explain psychopathology in children. These models have differed in their relative emphasis on certain causal mechanisms and constructs, and they often use very different terminology and concepts to describe seemingly similar child characteristics and behaviors. Biological paradigms, for example, have emphasized genetic mutations, neuroanatomy, and neurobiological mechanisms as factors contributing to psychopathology, whereas psychological paradigms have focused on the interpersonal and family relationships that shape a child’s cognitive, behavioral, and affective development. Although each of the various models places relative importance to certain causal processes versus others, most models recognize the role of multiple interacting influences. There is a growing recognition to look beyond the emphasis of singlecause theories and to integrate currently available models through intra- and interdisciplinary research efforts (cf. Arkowitz, 1992).
Interdisciplinary perspectives on disorders of childhood and adolescence mirror the considerable investment in children on the part of many different disciplines and professions, each of which has its own unique perspective of child psychopathology. Psychiatry-medicine, for example, has viewed and defined such problems categorically in terms of the presence or absence of a particular disorder or syndrome that is believed to exist within the child. In contrast, psychology has conceptualized psychopathology as an extreme occurrence on a continuum or dimension of characteristic(s) and has also focused on the role of environmental influences that operate outside the child. However, the boundaries are arbitrarily drawn between categories and dimensions, or between inner and outer conditions and causes, and there is growing recognition to find workable ways of integrating the two different worldviews of psychiatry-medicine and psychology (Richters & Cicchetti, 1993).
Child and Adolescent Disorders: an Overview
Many of the disorders that are present in adults are also present in children in one form or another, although admittedly the pathways are complex. Even though children can have similar mental health problems as adults, their problems often have a different focus. Children may experience difficulty with normal developmental tasks, such as beginning school, or they may lag behind other children their age or behave like a younger child during stressful periods. Even when children have problems that appear in adults, their problems may be expressed differently. For example, anxious children may be very concerned about their parents and other family members and may want to be near them at all times to be sure that everyone is all right.
The APA’s Diagnostic and Statistical Manual of Mental Disorders–Fourth Edition–Text Revision (DSM-IV-TR; APA, 2000) recognizes the uniqueness of childhood disorders in a separate section for disorders usually first diagnosed in infancy, childhood, or adolescence. However, this designation is viewed primarily as a matter of convenience, recognizing that the distinction between disorders in children and those in adults is not always clear. For example, although most individuals with disorders display symptoms during childhood and adolescence, they sometimes are not diagnosed until adulthood. In addition, many disorders not included in the childhood disorders section of DSM-IV-TR often have their onset during childhood and adolescence, such as depression, schizophrenia, and bipolar disorder.
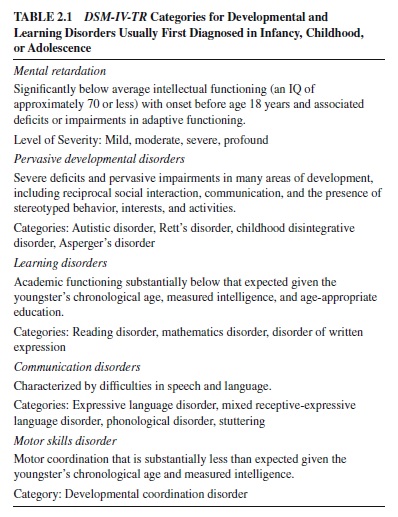
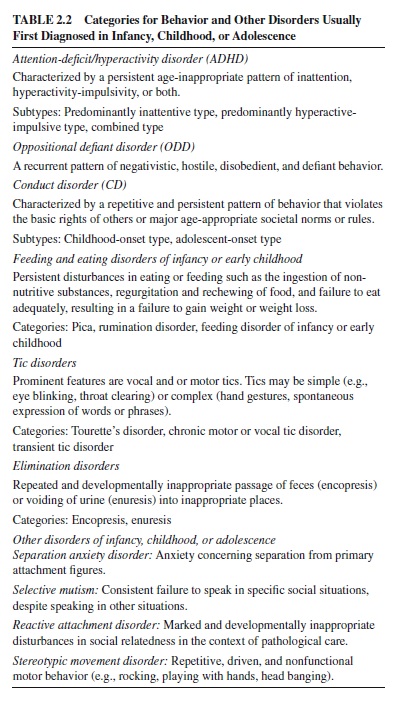
A brief overview of DSM-IV-TR disorders of childhood is presented in Table 2.1 for problems in development and learning and in Table 2.2 for behavior and other disorders. The disorders listed in these tables have traditionally been thought of as first occurring in childhood or as exclusive to childhood and as requiring child-specific operational criteria.
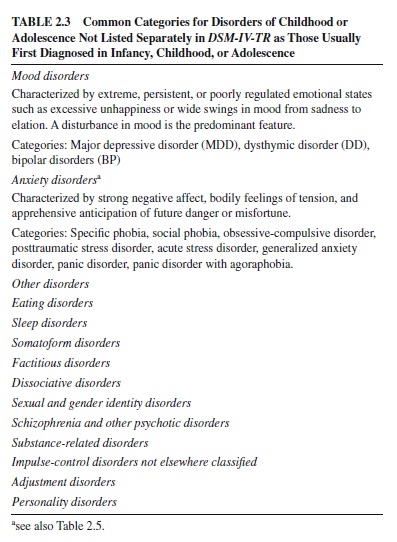
In addition to the separate listing of disorders of childhood and adolescence, many other DSM-IV-TR disorders apply to children and adolescents. As highlighted in Table 2.3, the most common of these are mood and anxiety disorders. For these disorders, the same diagnostic criteria are used for children and adults with various adjustments made based on the age-appropriateness, duration, and—in some instances—the types of symptoms.
The DSM-IV-TR distinction between child and adult categories is recognized as being arbitrary—more a reflection of our current lack of knowledge concerning the continuitiesdiscontinuities between child and adult disorders than of the existence of qualitatively distinct conditions (Silk, Nath, Siegel, & Kendall, 2000). Recent efforts to diagnose ADHD in adults illustrate this problem (Faraone, Biederman, Feighner, & Monuteaux, 2000). Whereas the criteria for ADHD were derived from work with children and the disorder is included in the child section of DSM-IV-TR, the same criteria are used to diagnose adults even though they may not fit the expression of the disorder in adults very well. Similarly, it is not clear that the degree of differentiation represented by the many DSM-IV-TR categories for anxiety disorders in adults fits with how symptoms of anxiety are expressed during childhood, which may reflect differences related to when symptoms appear in development rather than to the type of disorder (Zahn-Waxler, Klimes-Dougan, & Slattery, 2000). The more general issue here is whether there is a need for separate diagnostic criteria for children versus adults or whether the same criteria can be used by adjusting them to take into account differences in developmental level and context.
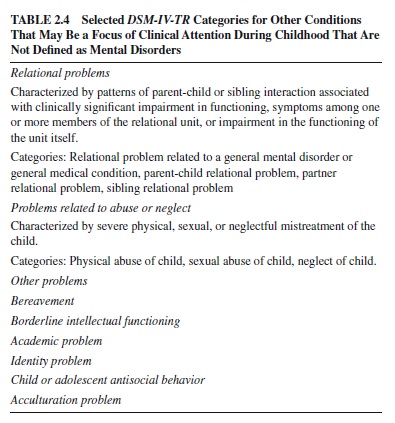
There are a number of additional DSM-IV-TR categories for other conditions that are not defined as mental disorders but are frequently a focus of clinical attention during childhood. As highlighted in Table 2.4, these categories include relational problems, maltreatment, and academic and adjustment difficulties. The relational nature of most childhood disorders underscores the significance of these categories for diagnosing children and adolescents (Mash & Johnston, 1996). Although DSM-IV-TR does not provide the specifics needed to adequately diagnose these complex concerns, it does call attention to their importance.
In the sections that follow, we consider the two most common types of child and adolescent disorders: externalizing and internalizing problems. Youngsters with externalizing problems generally display behaviors that are disruptive and harmful to others (Campbell, Shaw, & Gilliom, 2000). In contrast, those with internalizing problems experience inner-directed negative emotions and moods such as sadness, guilt, fear, and worry (Zahn-Waxler et al., 2000). In reality, both types of disorders have behavioral, emotional, and cognitive components, and there is substantial overlap between the two.
Externalizing Disorders: Attention-Deficit/Hyperactivity Disorder (Adhd)
Externalizing disorders are characterized by a mix of impulsive, overactive, aggressive, and delinquent acts (G. L. Burns et al., 1997). They include a wide range of acting-out behaviors—from annoying but mild behaviors such as noncompliance and tantrums to more severe behaviors such as physical aggression and stealing (McMahon & Estes, 1997). The two major types of externalizing disorders are (a) disruptive behavior disorders and (b) ADHD. We limit our discussion to ADHD and discuss its symptoms and subtypes, epidemiology, developmental course, accompanying disorders, associated features, causes, and possible developmental pathways. Many of the issues that we address in discussingADHD (e.g., prevalence estimates, comorbidity, gender and cultural factors, multiple and interacting causes, developmental pathways) have relevance for most other disorders of childhood.
ADHD is characterized by persistent and age-inappropriate symptoms of inattention, hyperactivity-impulsivity, or both (Campbell, 2000). Children with ADHD have great difficulty focusing on demands, are in constant motion, act without thinking, or any combination of these. Views of ADHD have changed dramatically over the past century as a result of new findings and discoveries (Barkley, 1998).
Symptoms and Subtypes
The main attention deficit in ADHD appears to be one of sustained attention (Douglas, 1999). When presented with an uninteresting or repetitive task, the performance of a child with ADHD deteriorates over time compared to that of other children. However, findings are not always consistent and may depend on the definitions and tasks used to assess this construct (Hinshaw, 1994). Symptoms of hyperactivity and behavioral impulsivity are best viewed as a single dimension of behavior called hyperactivity-impulsivity (Lahey et al., 1988). The strong link between hyperactivity and behavioral impulsivity has led to suggestions that both are part of a more fundamental deficit in behavioral inhibition (Barkley, 1997; Quay, 1997).
The three core features of ADHD—inattention, hyperactivity, and impulsivity—are complex processes. The current view is that hyperactivity-impulsivity is an essential feature of ADHD. In contrast to inattention, it distinguishes children withADHD from those with other disorders and from normal children (Halperin, Matier, Bedi, Sharma, & Newcorn, 1992). As such, impulsivity-hyperactivity appears to be a specific marker for ADHD, whereas inattention is not (Taylor, 1995). Children with ADHD display a unique constellation and severity of symptoms but do not necessarily differ from comparison children on all types and measures of inattention, hyperactivity, and impulsivity (Barkley, 1998).
DSM-IV-TR specifies three ADHD subtypes based on the child’s primary symptoms, which have received growing empirical support (Eiraldi, Power, & Nezu, 1997; Faraone, Biederman, & Friedman, 2000; Gaub & Carlson, 1997a). Children with the combined type display symptoms of both inattention and hyperactivity; those with the predominantly hyperactive-impulsive type display primarily symptoms of hyperactivity-impulsivity; and those with the predominantly inattentive type display primarily symptoms of inattention. Children with the combined and predominantly hyperactiveimpulsive types are more likely to display problems in inhibiting behavior and in behavioral persistence than are those who are predominantly inattentive. They are also more likely to be aggressive, defiant, and oppositional; to be rejected by their peers; and to be suspended from school or placed in special education classes (Lahey & Carlson, 1992). Because children who are predominantly hyperactive-impulsive are usually younger than those with the combined type, it is not yet known whether these are actually two distinct subtypes or the same type at different ages (Barkley, 1996).
Children who are predominantly inattentive are described as inattentive and drowsy, daydreamy, spacey, in a fog or easily confused, and they commonly experience a learning disability. They process information slowly and find it hard to remember things. Their main deficits seem to be speed of information processing and selective attention. Growing—but not yet conclusive—evidence suggests that children who are predominantly inattentive constitute a distinct subgroup from other two types (Maedgen & Carlson, 2000). They appear to display different symptoms, associated conditions, family histories, outcomes, and responses to treatment (Barkley, 1998).
The DSM-IV-TR criteria for ADHD have a number of limitations (Barkley, 1996), several of which apply to other childhood disorders as well. First, they are developmentally insensitive, using the same symptom criteria for individuals of all ages—even though some symptoms, such as running and climbing, apply more to young children. In addition, the number of symptoms needed to make a diagnosis is not adjusted for age or level of maturity even though many of these symptoms show a general decline with age. Second, according to DSM-IV-TR, ADHD is a disorder that the child either has or does not have. However, because the number and severity of symptoms are also a matter of degree, children who fall just below the cutoff for ADHD are not necessarily qualitatively different from those who are just above it. In fact, over time, some children move in and out of the DSMIV-TR category as a result of fluctuations in their behavior. Third, there is some uncertainty about the DSM-IV-TR requirement that symptoms must have an onset prior to age 7. There seems to be little difference between children with an onset of ADHD before or after age 7 (Barkley & Biederman, 1997), and about half of children with ADHD who are predominantly inattentive do not manifest the disorder until after age 7 (Applegate et al., 1997). Finally, the requirement of persistence for 6 months may be too brief for young children. Many preschoolers display symptoms for 6 months, and the symptoms then go away. These limitations highlight the fact that DSM-IV-TR criteria are designed for specific purposes—classification and diagnosis. They help shape our understanding of ADHD and other childhood disorders but are also shaped by—and in some instances lag behind—new research findings.
Epidemiology
As many as one half of all clinic-referred children display ADHD symptoms either alone or in combination with other disorders, making it one of the most common referral problems in North America (Barkley, 1998). The best estimate is that about 3–7% of all school-age children in North America have ADHD (APA, 2000; Jensen et al., 1999). However, as with other disorders, estimates can and do vary widely because informants in different settings do not always agree on symptoms or may emphasize different symptoms. Teachers, for example, are especially likely to rate a child as inattentive when oppositional symptoms are also present (Abikoff, Courtney, Pelham, & Koplewicz, 1993). Because adults may disagree, prevalence estimates are much higher when based on just one person’s opinion than they are when based on a consensus (Lambert, Sandoval, & Sassone, 1978).
ADHD occurs much more frequently in boys than in girls, with estimates ranging from 6–9% for boys and from 2–3% for girls in the 6- to 12-year age range. In adolescence, overall rates of ADHD drop for both boys and girls, but boys still outnumber girls by the same ratio of 2:1 to 3:1. This ratio is even higher in clinic samples, in which boys outnumber girls by 6:1 or more—most likely because boys are referred more frequently due to their defiance and aggression (Szatmari, 1992). ADHD in girls may go unrecognized and unreported because teachers may fail to recognize and report inattentive behavior unless it is accompanied by the disruptive symptoms normally associated with boys (McGee & Feehan, 1991). In fact, many of the DSM-IV-TR symptoms, such as excessive running around, climbing, and blurting out answers in class are generally more common in boys than in girls. Thus, sampling, referral, and definition biases may be a factor in the greater reported prevalence ofADHD in boys than in girls.
In the past, girls with ADHD were a highly under-studied group (Arnold, 1996). However, recent findings show that girls with ADHD are more likely to have conduct, mood, and anxiety disorders; lower IQ and school achievement scores; and greater impairment on measures of social, school, and family functioning than are girls without ADHD (Biederman et al., 1999; Greene et al., 2001; Rucklidge & Tannock, 2001). In addition, the expression, severity of symptoms, family correlates, and response to treatment are similar for boys and girls with ADHD (Faraone et al., 2000; Silverthorn, Frick, Kuper, & Ott, 1996). When gender differences are found, boys show more hyperactivity, more accompanying aggression and antisocial behavior, and greater impairment in executive functions, whereas girls show greater intellectual impairment (Gaub & Carlson, 1997b; Seidman, Biederman, Faraone, & Weber, 1997).
Developmental Course
The symptoms of ADHD are probably present at birth, although reliable identification is difficult until the age of 3–4 years when hyperactive-impulsive symptoms become increasingly more salient (Hart, Lahey, Loeber, Applegate, & Frick, 1996). Preschoolers with ADHD act suddenly without thinking, dashing from activity to activity, grabbing at immediate rewards; they are easily bored and react strongly and negatively to routine events (Campbell, 1990; DuPaul, McGoey, Eckert, & VanBrakle, 2001). Symptoms of inattention emerge at 5–7 years of age, as classroom demands for sustained attention and goal-directed persistence increase (Hart et al., 1996). Symptoms of inattention continue through grade school, resulting in low academic productivity, distractibility, poor organization, trouble meeting deadlines, and an inability to follow through on social promises or commitments to peers (Barkley, 1996).
The child’s hyperactive-impulsive behaviors that were present in preschool continue, with some decline, during the years from 6 to 12. During elementary school, oppositional defiant behaviors may also develop (Barkley, 1998). By 8–12 years, defiance and hostility may take the form of serious problems, such as lying or aggression. Through the school years,ADHD increasingly takes its toll as children experience problems with self-care, personal responsibility, chores, trustworthiness, independence, social relationships, and academic performance (Koplowicz & Barkley, 1995; Stein, Szumoski, Blondis, & Roizen, 1995). Although hyperactive-impulsive behaviors decline significantly by adolescence, they still occur at a level higher than in 95% of same-age peers (Barkley, 1996). The disorder continues into adolescence for at least 50% or more of clinic-referred elementary school children (Barkley, Fisher, Edelbrock, & Smallish, 1990; Weiss & Hechtman, 1993). Childhood symptoms of hyperactivityimpulsivity (more so than those of inattention) are generally related to poor adolescent outcomes (Barkley, 1998). Some youngsters withADHD either outgrow their disorder or learn to cope with it. However, many continue to experience problems, leading to a lifelong pattern of suffering and disappointment (Mannuzza & Klein, 1992).
Accompanying Disorders and Symptoms
As many as 80% of children with ADHD have a co-occurring disorder (Jensen, Martin, & Cantwell, 1997). About 25% or more have a specific learning disorder (Cantwell & Baker, 1992; Semrud-Clikeman et al., 1992) and 30–60% have impairments in speech and language (Baker & Cantwell, 1992; Cohen et al., 2000). About half of all children with ADHD— mostly boys—also meet criteria for oppositional defiant disorder (ODD) by age 7 or later, and 30–50% eventually develop conduct disorder (CD; Barkley, 1998; Biederman, Faraone, & Lapey, 1992). ADHD, ODD, and CD tend to run in families, which suggests a common causal mechanism (Biederman et al., 1992). However, ADHD is usually associated with cognitive impairments and neurodevelopmental difficulties, whereas conduct problems are more often related to family adversity, parental psychopathology, and social disadvantage (Schachar & Tannock, 1995).
About 25% of children with ADHD—usually younger boys—experience excessive anxiety (Tannock, 2000). It is interesting to note that the overall relationship between ADHD and anxiety disorders is reduced or eliminated in adolescence. The co-occurrence of an anxiety disorder may inhibit the adolescent with ADHD from engaging in the impulsive behaviors that characterize other youngsters with ADHD (Pliszka, 1992). As many as 20% of children with ADHD experience depression, and even more eventually develop depression or another mood disorder by early adulthood (Mick, Santangelo, Wypij, & Biederman, 2000; Willcutt, Pennington, Chhabildas, Friedman, & Alexander, 1999). The association between ADHD and depression may be a function of family risk for one disorder’s increasing risk for the other (Biederman et al., 1995).
Associated Features
Children with ADHD display many associated cognitive, academic, and psychosocial deficits. They consistently show deficits in executive functions—particularly those related to motor inhibition (Pennington & Ozonoff, 1996). Most children with ADHD are of at least normal overall intelligence, but they experience severe difficulties in school nevertheless (Fischer, Barkley, Edelbrock, & Smallish, 1990). In fact, the academic skills of children with ADHD have been found to be impaired even before they enter the first grade (Mariani & Barkley, 1997).
The association between ADHD and general health is uncertain at this time (Barkley, 1998; Daly et al., 1996), although a variety of health problems have been suggested (e.g., upper respiratory infections, asthma, allergies, bedwetting, and other elimination problems). Instability of the sleep-wake system is characteristic of children with ADHD, and sleep disturbances are common (Gruber, Sadeh, & Raviv, 2000). Resistance to going to bed and fewer total hours may be the most significant sleep problems (Wilens, Biederman, & Spencer, 1994), although the precise nature of the sleep disturbance in ADHD is not known (Corkum, Tannock, & Moldofsky, 1998). Up to 50% of children with ADHD are described as accident-prone, and they are more than twice as likely as other children to experience serious accidental injuries, such as broken bones, lacerations, severe bruises, poisonings, or head injuries (Barkley, 1998).As young adults, they are at higher risk for traffic accidents and offenses (NadaRaja et al., 1997) as well as for substance abuse (Wilens, Biederman, Mick, Faraone, & Spencer, 1997) and risky sexual behaviors such as multiple partners and unprotected sex (Barkley, Fisher, & Fletcher, 1997).
Families of children withADHD experience many difficulties, including interactions characterized by negativity, child noncompliance, high parental control, and sibling conflict (Whalen & Henker, 1999). Parents may experience high levels of distress and related problems; the most common ones are depression in mothers and antisocial behavior (i.e., substance abuse) in fathers. Further stress on family life stems from the fact that parents of children with ADHD may themselves have ADHD and other associated conditions (Johnston & Mash, 2001). It is critical to note that high levels of family conflict and the links between ADHD and parental psychopathology and marital discord seem to be related to the child’s co-occurring conduct problems rather than toADHD alone.
Children and adolescents with ADHD display little of the give and take, cooperation, and sharing that characterize other children (Dumas, 1998; Henker & Whalen, 1999). They are disliked and uniformly rejected by peers, have few friends, and are often unhappy (Gresham, MacMillan, Bocian, Ward, & Forness, 1998; Landau, Milich, & Diener, 1998). Their difficulties in regulating their emotions (Melnick & Hinshaw, 2000) and the aggressiveness that frequently accompanies ADHD often lead to conflict and negative peer reputation (Erhardt & Hinshaw, 1994).
Causes
Current research into causal factors provides strong evidence for ADHD as a disorder with neurobiological determinants (Biederman & Spencer, 1999; Tannock, 1998). However, biological and environmental risk factors together shape the expression of ADHD symptoms over time following several different pathways (Johnston & Mash, 2001; Taylor, 1999). ADHD is a complex and chronic disorder of brain, behavior, and development; its cognitive and behavioral outcomes affect many areas of functioning (Rapport & Chung, 2000). Therefore, any explanation of ADHD that focuses on a single cause and single outcome is likely to be inadequate (Taylor, 1999).
Genetics
Several sources of evidence point to genetic influences as important causal factors in ADHD (Kuntsi & Stevenson, 2000). First, about one third of immediate and extended family members of children with ADHD are also likely to have the disorder (Faraone, Biederman, & Milberger, 1996; Hechtman, 1994). Of fathers who had ADHD as children, one third of their offspring have ADHD (Biederman et al., 1992; Pauls, 1991). Second, studies of biologically related and unrelated pairs of adopted children have found a strong genetic influence that accounts for nearly half of the variance in attentionproblem scores on child behavior rating scales (van den Oord, Boomsma, & Verhulst, 1994). Third, twin studies report heritability estimates ofADHD averaging .80 or higher (Tannock, 1998). Both the symptoms and diagnosis of ADHD show average concordance rates for identical twins of 65%—about twice that of fraternal twins (Gilger, Pennington, & DeFries, 1992). Twin studies also find that the greater the severity of ADHD symptoms, the greater the genetic contributions (Stevenson, 1992).
Finally, genetic analysis suggests that specific genes may account for the expression of ADHD in some children (Faraone et al., 1992). Preliminary studies have found a relation between the dopamine transporter (DAT) gene and ADHD (Cook et al., 1995; Gill, Daly, Heron, Hawi, & Fitzgerald, 1997). Studies have also focused on the gene that codes for the dopamine receptor gene (DRD4), which has been linked to the personality trait of sensation seeking (high levels of thrill-seeking, impulsive, exploratory, and excitable behavior; Benjamin et al., 1996; Ebstein et al., 1996). Findings that implicate specific genes within the dopamine system in ADHD are intriguing, and they are consistent with a model suggesting that reduced dopaminergic activity may be related to the behavioral symptoms of ADHD (Faraone et al., 1999; Winsberg & Comings, 1999). However, other genetic findings indicate that the serotonin system also plays a crucial role in mediating the hyperactive-impulsive components of ADHD (Quist & Kennedy, 2001). As with other disorders of childhood, it is important to keep in mind that in the vast majority of cases, the heritable components of ADHD are likely to be the result of multiple interacting genes on several different chromosomes. Taken together, the findings from family, adoption, twin, and specific gene studies suggest that ADHD is inherited, although the precise mechanisms are not yet known (Edelbrock, Rende, Plomin, & Thompson, 1995; Tannock, 1998).
Pre- and Perinatal Factors
Many factors that compromise the development of the nervous system before and after birth—such as pregnancy and birth complications, low birth weight, malnutrition, early neurological insult or trauma, and diseases of infancy—may be related toADHD symptoms (Milberger, Biederman, Faraone, Chen, & Jones, 1996; Milberger, Biederman, Faraone, Guite, & Tsuang, 1997). Although these early factors predict later symptoms ofADHD, there is little evidence that they are specific to ADHD because they also predict later symptoms of other disorders as well. A mother’s use of cigarettes, alcohol, or other drugs during pregnancy can have damaging effects on her unborn child. Mild or moderate exposure to alcohol before birth may lead to inattention, hyperactivity, impulsivity, and associated impairments in learning and behavior (Streissguth, Bookstein, Sampson, & Barr, 1995). Other substances used during pregnancy—such as nicotine or cocaine—can adversely affect the normal development of the brain and lead to higher than normal rates of ADHD (Weissman et al., 1999).
Neurobiological Factors
There is both indirect and direct support for neurobiological causal factors in ADHD (Barkley, 1998; Faraone & Biederman, 1998). There are known associations between events or conditions known to be related to neurological status and symptoms of ADHD. Among these are peri- and postnatal events and diseases; environmental toxins such as lead; language and learning disorders; and signs of neurological immaturity, such as clumsiness, poor balance and coordination, and abnormal reflexes. Other sources of indirect support include the improvement in ADHD symptoms produced by stimulant medications known to affect the central nervous system, the similarity between symptoms of ADHD and symptoms associated with lesions to the prefrontal cortex (Grattan & Eslinger, 1991), and the deficient performances of children with ADHD on neuropsychological tests associated with prefrontal lobe functions (Barkley, Grodzinsky, & DuPaul, 1992).
Neuroimaging studies have found that children with ADHD have a smaller right prefrontal cortex than do those without ADHD (Filipek et al., 1997) and show structural abnormalities in several parts of the basal ganglia (SemrudClikeman et al., 2000). Although simple and direct relations cannot be assumed between brain size and abnormal function, anatomic measures of frontostriatal circuitry are related to children’s performance on response inhibition tasks (Casey et al., 1997). In adults with ADHD and in adolescent girls with ADHD, positron-emission tomography (PET) scan studies have found reduced glucose metabolism in the areas of the brain that inhibit impulses and control attention (Ernst et al., 1994). Significant correlations have also been found between diminished metabolic activity in the left anterior frontal region and severity of ADHD symptoms in adolescents (Zametkin et al., 1993). Taken together, the findings from neuroimaging studies suggest the importance of the frontostriatal region of the brain inADHD. These studies tell us that in children with ADHD, there is a structural difference or less activity in certain regions of the brain, but they don’t tell us why.
Family Factors
Genetic studies find that psychosocial factors in the family account for only a small amount of the variance (less than 15%) in ADHD symptoms (Barkley, 1998), and explanations of ADHD based exclusively on negative family influences have received little support (Silverman & Ragusa, 1992; Willis & Lovaas, 1977). Nevertheless, family influences are important in understanding ADHD for several reasons (Johnston & Mash, 2001; Whalen & Henker, 1999). First, family influences may lead to ADHD symptoms or to a greater severity of symptoms. In some circumstances,ADHD symptoms may be the result of interfering and insensitive early caregiving practices (Jacobvitz & Sroufe, 1987). In addition, for children at risk for ADHD, family conflict may raise the severity of their hyperactive-impulsive symptoms to a clinical level (Barkley, 1996). Second, family problems may result from interacting with a child who is impulsive and difficult to manage (Mash & Johnston, 1990). The clearest support for this child-to-parent direction of effect comes from double-blind placebo control drug studies in which children’s ADHD symptoms were decreased using stimulant medications. Decreases in children’s ADHD symptoms produced a corresponding reduction in the negative and controlling behaviors that parents had previously displayed when their children were unmedicated (Barkley, 1988; Humphries, Kinsbourne, & Swanson, 1978). Third, family conflict is probably related to the presence, maintenance, and later emergence of associated ODD and CD symptoms. Many interventions for ADHD try to change patterns of family interaction to head off an escalating cycle of oppositional behavior and conflict (Sonuga-Barke, Daley, Thompson, LaverBradbury, & Weeks, 2001). Family influences may play a major role in determining the outcome of ADHD and associated problems even if such influences are not the primary cause of ADHD (Johnston & Mash, 2001).
Summary and Integration
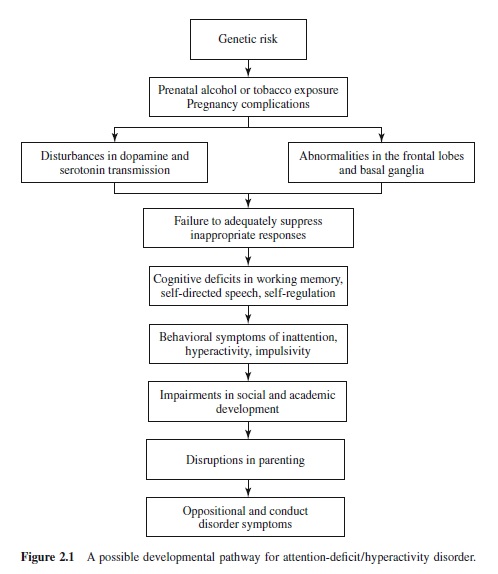
ADHD has a strong biological basis, and for many children, it is an inherited condition. However, the specific cause of the disorder is not known.ADHD is probably the result of a complex pattern of interacting influences.We are just beginning to understand the complex causal pathways through which biological risk factors, family relationships, and broader system influences interact to shape the development and outcome of ADHD over time (Hinshaw, 1994; Taylor, 1999). Although data do not yet permit a comprehensive causal model, a possible developmental pathway for ADHD that highlights several known causal influences and outcomes is shown in Figure 2.1. Findings generally suggest that inherited variants of genes related to the transmission of dopamine and serotonin lead to structural and functional abnormalities in the frontal lobes and basal ganglia regions of the brain. Altered neurological function causes changes in psychological function involving a failure of children to adequately suppress inappropriate responses; this in turnleads to many failures in cognitive performance. The outcome involves a pattern of restless and disorganized behavior that is identified as ADHD, that also impairs social development and functioning, and that may lead to symptoms of ODD and CD (Barkley, 1997; Taylor, 1999).
Internalizing Disorders: Anxiety Disorders
Internalizing disorders involve a core disturbance in emotions and moods such as worry, fear, sorrow, and guilt (ZahnWaxler et al., 2000). The two major types of internalizing disorders are (a) mood disorders and (b) anxiety disorders. Children with mood disorders experience extreme, persistent, or poorly regulated emotional states such as excessive unhappiness or wide swings in mood from sadness to elation. The two most common mood disorders in childhood are major depressive disorder (MDD) and dysthymic disorder (DD; APA, 2000). MDD and DD are related; many children with DD eventually develop MDD, and some children may experience both disorders (Lewinsohn, Rohde, Seeley, & Hops, 1991). A third mood disorder, bipolar disorder, is rare in children, although there is growing interest in this problem in young people (Carlson, Bromet, & Sievers, 2000; Geller & Luby, 1997). In the sections to follow, we limit our discussion to anxiety disorders, highlighting many of the same features that we covered for ADHD. Once again, issues that we raise in discussing anxiety disorders have relevance for other childhood disorders as well.
Anxiety disorders are among most common mental health problems in young people (Majcher & Pollack, 1996; Vasey & Ollendick, 2000). However, because milder forms of anxiety are a common occurrence in normal development and because anxiety disorders are not nearly as damaging to other people or property as are ADHD and disruptive behavior disorders, anxiety disorders frequently go unnoticed, undiagnosed, and untreated (Albano, Chorpita, & Barlow, 1996). Anxiety was once thought of as a transient problem, but we now know that many children who experience anxiety continue to have problems well into adolescence and adulthood (Ollendick & King, 1994). Although isolated symptoms of fear and anxiety are usually short-lived, anxiety disorders in children have a more chronic course (March, 1995). In fact, nearly half of those affected have an illness duration of 8 years or more (Keller et al., 1992).
Symptoms and Types
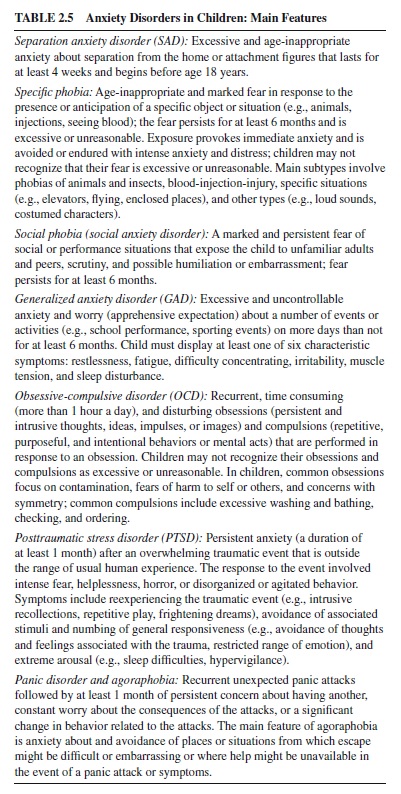
Anxiety is a mood state characterized by strong negative emotion and bodily symptoms of tension in which an individual apprehensively anticipates future danger or misfortune (Barlow, 1988). The term anxiety disorder describes children who experience excessive and debilitating anxiety. However, as described in Table 2.5, these disorders take a number of different forms that vary in focus and severity as a function of development. It is important to keep in mind that there is substantial overlap among these disorders in childhood (Pine, Cohen, Cohen, & Brook, 2000). Many children suffer from more than one type—either at the same time or at different times during their development (Zahn-Waxler et al., 2000).
Epidemiology and Accompanying Disorders
The overall prevalence rates for anxiety disorders in children range from about 6–18% (Costello & Angold, 2000). Rates vary as a function of whether functional impairment is part of the diagnostic criteria, with the informant, and with the type of anxiety disorder.
Separation Anxiety Disorder (SAD)
SAD is the most common anxiety disorder in youths, occurring in about 10% of all children. It seems to be equally common in boys and girls, although when gender differences are found they tend to favor girls (Last, Perrin, Hersen, & Kazdin, 1992). Most children with SAD have another anxiety disorder—most commonly generalized anxiety disorder (Last, Perrin, Hersen, & Kazdin, 1996). About one third develop a depressive disorder within several months of the onset of SAD. They may also display specific fears of getting lost or of the dark. School reluctance or refusal is also quite common in older children with SAD (King & Bernstein, 2001).
Specific Phobia
About 2–4% or more of all children experience specific phobias at some time in their lives (Essau, Conradt, & Petermann, 2000; Muris & Merckelbach, 2000). However, only a very small number of these children are referred for treatment, suggesting that most parents do not view specific phobias as a significant problem. Specific phobias— particularly blood phobia—are generally more common in girls than boys (Essau et al., 2000). The most common cooccurring disorder for children with a specific phobia is another anxiety disorder. Although comorbidity is frequent for children with specific phobias, it tends to be lower than it is for other anxiety disorders (Strauss & Last, 1993). Phobias involving animals, darkness, insects, blood, and injury typically have their onset at 7–9 years, which is similar to normal development. However, clinical phobias are much more likely to persist over time than are normal fears, even though both decline with age. Specific phobias can occur at any age but seem to peak between ages 10 and 13 years (Strauss & Last, 1993).
Social Phobia (Social Anxiety Disorder)
Social phobia occurs in 1–3% of children, affecting slightly more girls than boys (Essau, Conradt, & Petermann, 1999). Girls may experience more social anxiety because they are more concerned with social competence than are boys and attach greater importance to interpersonal relationships (Inderbitzen-Nolan & Walters, 2000). Among children referred for treatment for anxiety disorders, as many as 20% have social phobia as their primary diagnosis, and it is also the most common secondary diagnosis for children referred for other anxiety disorders (Albano et al., 1996). Even so, many cases of social phobia are overlooked because shyness is common in our society and because these children are not likely to call attention to their problem even when they are severely distressed (Essau et al., 1999). Two thirds of children and adolescents with a social phobia have another anxiety disorder—most commonly a specific phobia or panic disorder (Beidel, Turner, & Morris, 1999). About 20% of adolescents with a social phobia also suffer from major depression. They may also use alcohol and other drugs as a form of self-medication and as a way of reducing their anxiety in social situations (Albano et al., 1996).
Social phobias generally develop after puberty, with the most common age of onset in early to midadolescence (Strauss & Last, 1993). The disorder is extremely rare in children under the age of 10. The prevalence of social phobia appears to increase with age, although little information is available to describe the natural course of the disorder or its long-term outcome.
Generalized Anxiety Disorder (GAD)
Along with SAD, GAD is one of the most common anxiety disorders of childhood, occurring in 3–6% of all children (Albano et al., 1996). It is equally common in boys and girls, with perhaps a slightly higher prevalence in older adolescent females (Strauss, Lease, Last, & Francis, 1988). Children with GAD present with a high rate of other anxiety disorders and depression. For younger children, co-occurring SAD and ADHD are most frequent; older children with GAD tend to have specific phobias and major depression, impaired social adjustment, low self-esteem, and an increased risk for suicide (Keller et al., 1992; Strauss, Last, Hersen, & Kazdin, 1988). About half of children referred for treatment for anxiety disorders have GAD. This proportion is higher than it is for adults, in whom the disorder is more common, but fewer adults seek treatment (Albano et al., 1996).
The average age of onset for GAD is 10–14 years (Albano et al., 1996). In a community sample of adolescents with GAD, the likelihood of their having GAD at follow-up was higher if symptoms at the time of initial assessment were severe (Cohen, Cohen, & Brook, 1993). Nearly half of severe cases were rediagnosed after 2 years, suggesting that severe generalized anxiety symptoms persist over time, even in youngsters who have not been referred for treatment.
Obsessive-Compulsive Disorder (OCD)
The prevalence of OCD in children and adolescents is 2–3%, which suggests that it occurs about as often in young people as in adults (Piacentini & Graae, 1997). Clinic-based studies of younger children indicate that OCD is twice as common in boys as it is in girls. However, this gender difference has not been found in community samples of adolescents, which may be a function of age, referral bias, or both (Albano et al., 1996). The most common comorbidities for OCD are other anxiety disorders, depressive disorders (especially in older children with OCD), and disruptive behavior disorders (Piacentini & Graae, 1997). Substance use disorders, learning disorders, and eating disorders are also overrepresented in children with OCD, as are vocal and motor tics (Peterson, Pine, Cohen, & Brook, 2001; Piacentini & Graae, 1997).
The mean age of onset of OCD is 9–12 years with two peaks—one in early childhood and another in early adolescence (Hanna, 1995). Children with an early onset of OCD (age 6–10) are more likely to have a family history of OCD than are those with a later onset, which indicates a greater role of genetic influences in such cases (Swedo, Rapoport, Leonard, Lenane, & Cheslow, 1989). These children have prominent motor patterns, engaging in compulsions without obsessions and displaying odd behaviors, such as finger licking or compulsively walking in geometric designs. One half to two thirds of children with OCD continue to meet the criteria for the disorder 2–14 years later. Although most children, including those treated with medication, show some improvement in symptoms,fewerthan10%showcompleteremission(Albano, Knox, & Barlow, 1995).
Posttraumatic Stress Disorder (PTSD)
PTSD is common in children exposed to traumatic events (Perrin, Smith, & Yule, 2000). The prevalence of PTSD symptoms is greater in children who are exposed to lifethreatening events than it is in those who are not. For example, nearly 40% of children exposed to the Buffalo Creek dam collapse in 1972 showed probable PTSD symptoms 2 years after the disaster (Fletcher, 1996). PTSD in children is also strongly correlated with degree of exposure. In children exposed to a school yard sniper attack, proximity to the attack was linearly related to the risk of developing PTSD symptoms (Pynoos et al., 1987).Traumatized children frequently exhibit symptoms of other disorders besides PTSD, and children with other disorders may have PTSD as a comorbid diagnosis (Famularo, Fenton, Kinscherff, & Augustyn, 1996). The PTSD that occurs in children traumatized by fires, hurricanes, or chronic maltreatment may worsen or lead to disruptive behavior disorders (Amaya-Jackson & March, 1995).
Because PTSD can strike at any time during childhood, its course depends on the age of the child when the trauma occurred and on the nature of the trauma. Because the traumatic experience is filtered cognitively and emotionally before it can be appraised as an extreme threat, how trauma is experienced depends on the child’s developmental level. Some children appear to have different trauma thresholds, although exposure to horrific events is traumatic to nearly all children. Several trauma-related, child, and family factors appear to be important in predicting children’s course of recovery from PTSD following exposure to a natural disaster (La Greca, Silverman, & Wasserstein, 1998). Among these are loss and disruption following the trauma, preexisting child characteristics (e.g., psychopathology), coping styles, and social support (Perrin et al., 2000).
Longitudinal findings suggest that PTSD can become a chronic psychiatric disorder, persisting for decades or a lifetime (Fletcher, 1996). Children with chronic PTSD may display a developmental course marked by remissions and relapses. Moreover, individuals exposed to a traumatic event may not exhibit symptoms until months or years afterwards, when a situation that resembles the original trauma triggers the onset of PTSD. For example, sexual abuse during childhood may lead to PTSD in adult survivors.
Panic Disorder (PD)
Whereas panic attacks are common among adolescents (about 35–65%), panic disorder is much less common, affecting less than 1% to almost 5% of teens (Ollendick, Mattis, & King, 1994). Adolescent females are more likely to experience panic attacks than are adolescent males, and a fairly consistent association has been found between panic attacks and stressful life events (King, Ollendick, & Mattis, 1994; Last & Strauss, 1989). About half of adolescents with PD have no other disorder, and for the remainder an additional anxiety disorder and depression are the most common secondary diagnoses (Kearney, Albano, Eisen, Allan, & Barlow, 1997; Last & Strauss, 1989). After months or years of unrelenting panic attacks and the restricted lifestyle that results from avoidance behavior, adolescents and young adults with PD may develop severe depression and may be at risk for suicidal behavior. Others may begin to use alcohol or drugs as a way of alleviating their anxiety.
The average age of onset for a first panic attack in adolescents with PD is 15–19 years, and 95% of adolescents with the disorder are postpubertal (Bernstein, Borchardt, & Perwien, 1996; Kearney & Allan, 1995). PD occurs in otherwise emotionally healthy youngsters about half the time. The most frequent prior disturbance when there is one is a depressive disorder (Last & Strauss, 1989). Unfortunately, children and adolescents with PD have the lowest rate of remission for any of the anxiety disorders (Last et al., 1996).
Gender, Ethnicity, and Culture
Studies have found a preponderance of anxiety disorders in girls during childhood and adolescence (Lewinsohn, Gotlib, Lewinsohn, Seeley, & Allen, 1998). By age 6, twice as many girls as boys have experienced symptoms of anxiety, and this discrepancy persists through childhood and adolescence. Such findings should be interpreted cautiously, however, because the possibility that girls are more likely than are boys to report anxiety cannot be ruled out as an alternative explanation.
Research into the relationship between ethnic and cultural factors and childhood anxiety disorders is limited and inconclusive. Studies comparing the number and nature of fears in African American and White youngsters have found the two groups to be quite similar (Ginsburg & Silverman, 1996; Treadwell, Flannery-Schroeder, & Kendall, 1994). However, African American children report more symptoms of anxiety than do White children (Cole, Martin, Peeke, Henderson, & Harwell, 1998). White children endorse more symptoms of social phobia and fewer symptoms of separation anxiety than do African American children (Compton, Nelson, & March, 2000). The underrepresentation of minorities and children of lower socioeconomic status (SES) for certain anxiety disorders such as OCD could also reflect a bias in which minority children are less likely to be referred for treatment (Neal & Turner, 1991).
Among children referred for anxiety disorders, Whites are more likely to present with school refusal and higher severity ratings, whereas African Americans are more likely to have a history of PTSD and a somewhat greater number of fears (Last & Perrin, 1993). Although anxiety may be similar in the two groups, patterns of referral, help-seeking behaviors, diagnoses, and treatment processes are likely to differ. For example, African Americans may be more likely to turn for help with their child’s OCD symptoms to members of their informal social network, such as clergy or medical personnel, than to mental health professionals (Hatch, Friedman, & Paradis, 1996). Their family members are also less likely to be drawn into the child’s OCD symptoms.
Research comparing phobic and anxiety disorders in Hispanic and White children finds marked similarities on most measures, including age at intake, gender, primary diagnoses, proportion of school refusal, and proportion with more than one diagnosis. Hispanic children are more likely to have a primary diagnosis of SAD. Hispanic parents also rate their children as more fearful than do White parents (Ginsburg & Silverman, 1996). Few studies have examined anxiety disorders in Native American children. Prevalence estimates from one study of Native American youth in Appalachia (mostly Cherokee) indicate rates of anxiety disorders similar to those for White youth, with the most common disorder for both groups being SAD. Rates of SAD were slightly higher for Native American youth, especially for girls (Costello, Farmer, Angold, Burns, & Erkanli, 1997).
Although cross-cultural research into anxiety disorders in children is limited, specific fears in children have been studied and documented in virtually every culture. Developmental fears (e.g., a fear of loud noises or separation anxiety) occur in children of all cultures at about the same age. The number of fears in children tends to be highly similar across cultures, as does the presence of gender differences in pattern and content. Nevertheless, the expression and developmental course of fear and anxiety may be affected by culture. Cultures that favor inhibition, compliance, and obedience have increased levels of fear in children (Ollendick, Yang, King, Dong, & Akande, 1996).
Accompanying Disorders and Symptoms
A child’s risk for accompanying disorders varies with the type of anxiety disorder. Social phobia, GAD, and SAD are more commonly associated with depression than is specific phobia. Depression is also diagnosed more often in children with multiple anxiety disorders and in those who show severe impairments in their everyday functioning (Bernstein, 1991).
The strong and undeniable relationship between anxiety and depression in young people merits further discussion (Kendall & Brady, 1995; Mesman & Koot, 2000). Does anxietyleadtodepression,areanxietyanddepressionthesamedisorder with different clinical features, are they on a continuum of severity, or are they distinct disorders with different causes but some overlapping features (Seligman & Ollendick, 1998; Zahn-Waxler et al., 2000)? Children with anxiety and depression are older at age of presentation than are children with anxiety alone, and in most cases symptoms of anxiety both precede and predict those of depression (Brady & Kendall, 1992; Cole, Peeke, Martin, Truglio, & Seroczynski, 1998). Symptoms of anxiety and depression may form a single indistinguishable dimension in younger children but are increasingly distinct in older children and in children with at least one diagnosable disorder (Cole, Truglio, & Peeke, 1997; Gurley, Cohen, Pine, & Brook, 1996). Recent studies of children’s negative emotional symptoms generally support the three distinct constructs of anxiety, depression, and fear, with anxiety corresponding to negative affect, depression to low positive affect, and fear to physiological overarousal (Chorpita, Daleiden, Moffitt,Yim, & Umemoto, 2000; Joiner & Lonigan, 2000; Lonigan, Hooe, David, & Kistner, 1999).
Associated Features
Children with anxiety disorders are typically of normal intelligence, and there is little evidence of a strong relationship between anxiety and IQ. However, excessive anxiety may be related to deficits in specific areas of cognitive functioning, such as memory, attention, and speech or language. High levels of anxiety can interfere with academic performance. One study found that anxiety in the first grade predicted anxiety in the fifth grade and significantly influenced fifthgrade achievement (Ialongo, Edelsohn, Werthamer-Larsson, Crockett, & Kellam, 1995). The specific mechanisms involved could include anything from frequent absences to direct interference on cognitive tasks, such as writing a test or solving a math problem.
Children with anxiety disorders selectively attend to information that may be potentially threatening, a tendency referred to as anxious vigilance or hypervigilance (Vasey, El-Hag, & Daleiden, 1996). Anxious vigilance is maintained because it permits the child to avoid potentially threatening events by means of early detection and with minimal anxiety and effort. Although this strategy may benefit the child in the short term, it has the negative long-term effect of maintaining and heightening anxiety by interfering with the informationprocessing and coping responses needed to learn that many potentially threatening events are not so dangerous after all (Vasey et al., 1996).
When faced with a clear threat, both normal and anxious children use rules to confirm information about danger and play down information about safety. However, high-anxious children often do this in the face of less obvious threats, suggesting that their perceptions of threat activate a dangerconfirming reasoning strategy (Muris, Merckelbach, & Damsma, 2000). Anxious children generally engage in more negative self-talk than do nonanxious children. However, positive self-talk does not distinguish anxious children from controls, suggesting that their internal dialogue is more negative but not necessarily less positive than that of other children (Treadwell & Kendall, 1996). Although cognitive errors and distortions are associated with anxiety in children, their possible role in causing anxiety has not been established (Seligman & Ollendick, 1998).
Children with anxiety disorders often experience somatic symptoms such as stomachaches or headaches. These complaints are more common in youngsters with PD and SAD than in those with a specific phobia. Somatic complaints are also more frequent in adolescents than in younger children and in children who display school refusal. Children with anxiety disorders may also have sleep disturbances. Some may experience nocturnal panic—an abrupt waking in a state of extreme anxiety—that is similar to a daytime panic attack. Nocturnal panic attacks usually occur in adolescents with PD (Craske & Rowe, 1997).
Many children with anxiety disorders have low social competence and high social anxiety, and their parents and teachers are likely to view such children as anxious and socially maladjusted (Chansky & Kendall, 1997; Krain & Kendall, 2000; Strauss, Lease, Kazdin, Dulcan, & Last, 1989). Compared to their peers, these children are more likely to see themselves as shy and socially withdrawn and more likely to report low selfesteem, loneliness, and difficulties in starting and maintaining friendships. Some of their difficulties with peers may be related to specific deficits in emotion understanding—particularly in hiding and changing emotions (Southam-Gerow & Kendall, 2000). Findings are mixed regarding how children with anxiety disorders are viewed by other children (Kendall, Panichelli-Mindel, Sugarman, & Callahan, 1997). It appears that childhood anxiety disorders are most likely to be associated with diminished peer popularity when they coexist with depression (Strauss, Lahey, Frick, Frame, & Hynd, 1988).
Causes
It is important to recognize that different anxiety disorders may require different causal models. For example, the affective, physiological, and interpersonal processes in GAD may differ from those in other anxiety disorders (T. M. Borkovec & Inz, 1990). Current models of anxiety emphasize the importance of interacting biological and environmental influences (Chorpita & Barlow, 1998; Zahn-Waxler et al., 2000).
Early Temperament
Early temperament has been implicated as a precursor for anxiety disorders. Children differ markedly in their reactions to novel or unexpected events—perhaps because of genetics, gender, cultural background, prior experience, or a combination of factors. Orienting, attending, vigilance, wariness, and motor readiness in response to the unfamiliar are important mechanisms for survival. From an evolutionary perspective, abnormal fears and anxieties partly reflect variation among infants in their initial behavioral reactions to novelty (Kagan, 1997).
This variation is a reflection of inherited differences in the neurochemistry of structures that are thought to play an important role in detecting discrepant events (Kagan, Snidman, Arcus, & Reznick, 1994). These structures include the amygdala and its projections to the motor system, the cingulate and frontal cortex, the hypothalamus, and the sympathetic nervous system. Children who have a high threshold to novelty are presumed to be at low risk for developing anxiety disorders. Other children are born with a tendency to become overexcited and to withdraw in response to novel stimulation—an enduring trait for some and a possible risk factor for the development of later anxiety disorders (Kagan & Snidman, 1999; Schwartz, Snidman, & Kagan, 1999).
The pathway from a shy-inhibited temperament in infancy and childhood to a later anxiety disorder is neither direct nor straightforward. Although a shy-inhibited temperament may contribute to later anxiety disorders, it is not an inevitable outcome (Prior, Smart, Sanson, & Oberklaid, 2000). Such an outcome probably depends on whether the inhibited child grows up in an environment that fosters this tendency (Kagan, Snidman, & Arcus, 1992). For example, a parent’s use of firm limits that teach inhibited children how to cope with stress may reduce their risk for later anxiety. In contrast, it is possible that well-meaning but overprotective parents who shield their sensitive child from stressful events may inadvertently encourage a continuation of timidity by preventing the child from confronting fears and—by doing so— eliminating them. Such tendencies in the parents of inhibited children may be common (Hirshfeld et al., 1992; Rosenbaum et al., 1991). Thus, inhibited children may be at high risk not only because of their inborn temperament but also because of their elevated risk of exposure to anxious, overprotective parenting (Turner, Beidel, & Wolff, 1996).
Genetics
Family and twin studies suggest a biological vulnerability to anxiety disorders, indicating that children’s general tendencies to be inhibited, tense, or fearful are inherited (DiLalla, Kagan, & Reznick, 1994). However, little research exists at present to support a direct link between specific genetic markers and specific types of anxiety disorders. Contributions from multiple genes seem related to anxiety only when certain psychological and social factors are also present.
The overall concordance rates for anxiety disorders are significantly higher for monozygotic (MZ) twins than for dizygotic (DZ) twins (Andrews, Stewart, Allen, & Henderson, 1990). However, MZ twin pairs do not typically have the same types of anxiety disorders. This finding suggests that what is inherited is a disposition to become anxious, and the form that the disorder takes is a function of environmental influences. Twin and adoption studies of anxiety in children and adolescents may be summarized as follows: There is a genetic influence on anxiety in childhood that accounts for about one third of the variance in most cases; heritability for anxiety may be greater for girls than for boys; shared environmental influences or experiences that make children in the same family resemble one another (e.g., maternal psychopathology, ineffective parenting, or poverty) have a significant influence on anxiety disorders in children and adolescents (Eley, 1999).
Two lines of evidence suggest that anxiety disorders run in families. First, parents of children with anxiety disorders have increased rates of current and past anxiety disorders. Second, children of parents with anxiety disorders have an increased risk for anxiety disorders (McClure, Brennan, Hammen, & Le Brocque, 2001). Children of parents with anxiety disorders are about five times more likely to have anxiety disorders than are children of parents without anxiety disorders (Beidel & Turner, 1997). However, they are not necessarily the same anxiety disorders (Mancini, van Ameringen, Szatmari, Fugere, & Boyle, 1996). Nearly 70% of children of parents with agoraphobia meet diagnostic criteria for disorders such as anxiety and depression, and they report more fear and anxiety and less control over various risks than do children of comparison parents. However, the fears of parents with agoraphobia and the fears of their children are no more closely aligned than are those of nonanxious parents and their children, once again supporting the view that it is a general predisposition for anxiety that is perpetuated in families (Capps, Sigman, Sena, & Henker, 1996).
Neurobiological Factors
The part of the brain most often connected with anxiety is the limbic system, which acts as a mediator between the brain stem and the cortex (Sallee & Greenawald, 1995). Signs of potential danger are monitored and sensed by the more primitive brain stem, which then relays them to the higher cortical centers via the limbic system. This brain system is referred to as the behavioral inhibition system and is believed to be overactive in children with anxiety disorders. Neuroimaging studies point to abnormalities in limbic-based amygdala, septohippocampal, and brain stem hypothalamic circuits as being associated with anxiety disorders (Pine & Grun, 1999).
Agroup of neurons known as the locus ceruleus is a major brain source for norepinephrine, an inhibitory neurotransmitter. Overactivation of this region is presumed to lead to a fear response, and underactivity is presumed to lead to inattention, impulsivity, and risk taking. Abnormalities of these systems appear to be related to anxiety states in children (Sallee & Greenawald, 1995). The neurotransmitter system that has been implicated most often in anxiety disorders is the gamma-aminobutyric acid (GABAergic) system.
Family Factors
Surprisingly little is known about the relation between parenting styles or family factors and anxiety disorders. Parents of anxious children are often described as overinvolved, intrusive, or limiting of their child’s independence. Observations of interactions between 9- to 12-year-old children with anxiety disorders and their parents found that parents of children with anxiety disorders were rated as granting less autonomy to their children than were other parents; the children rated their mothers and fathers as being less accepting (Siqueland, Kendall, Steinberg, 1996). Other studies have found that mothers of children previously identified as behaviorally inhibited are more likely to use criticism when interacting with their children and that emotional overinvolvement by parents is associated with an increased occurrence of SAD in their children (Hirshfeld, Biederman, Brody, & Faraone, 1997; Hirshfeld, Biederman, & Rosenbaum, 1997). These findings generally support the notion of excessive parental control as a parenting style associated with anxiety disorders in children, although the causal role of such a style is not yet known (Chorpita & Barlow, 1998; Rapee, 1997).
Not only do parents of children with anxiety disorders seem to be more controlling than do other parents, but they also have different expectations of their children. For example, when they thought the child was being asked to give a videotaped speech, mothers of children with anxiety disorders expected their children to become upset and had low expectations for their children’s coping (Kortlander, Kendall, & Panichelli-Mindel, 1997). It is likely that parental attitudes shape—and are shaped by—interactions with the child, during which parent and child revise their expectations and behavior as a result of feedback from the other (Barrett, Rapee, Dadds, & Ryan, 1996).
Insecure early attachments may be a risk factor for the development of later anxiety disorders (Bernstein et al., 1996; Manassis & Bradley, 1994). Mothers with anxiety disorders have been found to have insecure attachments themselves, and 80% of their children are also insecurely attached (Manassis, Bradley, Goldberg, Hood, & Swinson, 1994). Infants who are ambivalently attached have more anxiety diagnoses in childhood and adolescence (Bernstein et al., 1996).Although it is a risk factor, insecure attachment may be a nonspecific one in that many infants with insecure attachments develop disorders other than anxiety (e.g., disruptive behavior disorder), and many do not develop any disorders.
Summary and Integration
There is much debate regarding the distinctness of the DSMIV-TR childhood anxiety disorders, with some individuals emphasizing the similarities among these disorders and others emphasizing the differences (Pine, 1997). An emphasis on similarities is consistent with the strong associations among the different disorders, the presence of shared risk factors such as female gender, and evidence of a broad genetic predisposition for anxiety. An emphasis on differences is consistent with different developmental progressions and outcomes as well as differences in the biological correlates of anxiety disorders in children versus adults (Pine et al., 2000). Children with anxiety disorders will most likely display features that are shared across the various disorders as well as other features that are unique to their particular disorder.
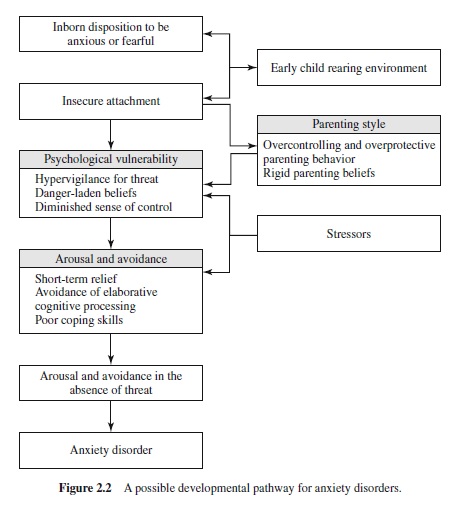
A possible developmental pathway for anxiety disorders in children is shown in Figure 2.2. In children with an inborn predisposition to be anxious or fearful, the child’s sense that the world is not a safe place may create a psychological vulnerability to anxiety. After anxiety occurs, it feeds on itself. The anxiety and avoidance continue long after the stresses that provoked them are gone. In closing, it is important to keep in mind that many children with anxiety disorders do not continue to experience problems as adults. Therefore, it will be important to identify risk and protective factors that would explain these differences in outcomes (Pine & Grun, 1999).
Current Issues and Future Directions
ADHD and anxiety—like most disorders of childhood and adolescence—involve broad patterns of behavior and dysfunction that unfold over time as the result of multiple interacting risk and protective factors in the child and the environment (Rutter & Sroufe, 2000). Building on our discussion of these disorders, we next highlight a number of current issues and future directions related to the study of child psychopathology more generally.
Defining Disorders of Childhood and Adolescence
Defining child psychopathology and identifying the boundaries between abnormal and normal functioning are arbitrary processes at best—subject to meaning-based cultural interpretations (Hoagwood & Jensen, 1997). Traditional psychiatric approaches to defining mental disorders in children have emphasized concepts such as symptoms, diagnosis, and illness as residing within the child, and by doing so, they have strongly influenced the ways in which we think about child psychopathology and related questions (Richters & Cicchetti, 1993). Implicit in these approaches was the view that a single primary cause would be found for each disorder and that this cause would be diagnosis specific (Rutter & Sroufe, 2000). They also gave little attention to causes as dynamic processes that operate over time, the role of context, direct and indirect influences, and developmental pathways.
The DSM-IV-TR diagnostic categories for childhood disorders clearly reflect this tradition. As a result, there has been ongoing concern about the subjective formulation and static nature of these categories, their insensitivity to developmental, age, gender, and contextual parameters, and their heterogeneity and overlap (Mash & Terdal, 1997a). In addition, many of the DSM-IV-TR categories for describing child psychopathology are downward extensions of concepts and categories developed for adults. There remains a need for a developmental system of classification.
Many childhood disorders such as anxiety, depression, and disruptive behavior appear to reflect dimensions of personality rather than categorical problems (Werry, 2001). Even disorders such as autism that have traditionally been viewed as categorical in nature can be conceptualized as an extreme on a continuum of social behavior (Baron-Cohen, 2000). For dimensional disorders, children who score just below the cutoff for a diagnosis may one day meet criteria and often show impairment that is comparable to that of children who score above the cutoff. Similarly, those above the cutoff may someday move below.
Current definitions of child psychopathology are cognizant of the need for standardized approaches to diagnosis and classification, and the DSM-IV-TR criteria represent a considerable improvement over the idiosyncratic definitions that characterized previous practices. However, the limitations of traditional diagnostic approaches indicate a need to broaden these perspectives to incorporate dimensional concepts and dynamic causal processes. This melding of ideas and approaches within the interdisciplinary framework known as developmental psychopathology (Cicchetti & Sroufe, 2000) will likely continue to advance our definition and understanding of childhood disorders and our ability to help children who suffer from them.
Healthy Functioning
The study of child psychopathology requires attention to normal developmental processes for several reasons (Cicchetti & Richters, 1993). First, judgments of abnormality require knowledge about developmental functioning relative to same-age peers and to the child’s own baseline of development. Second, normal and abnormal functioning represent two sides of the same coin in that dysfunction in a particular domain of development (e.g., cognitive) is usually accompanied by a failure to meet developmental tasks and expectations in the same domain (e.g., academic performance). Third, in addition to the specific problems that lead to referral and diagnosis, disturbed children are also likely to show impairments in other areas of adaptive functioning. Fourth, most children with specific disorders are known to cope effectively in some areas of their lives. Understanding the child’s competencies informs our knowledge of the disorder and provides a basis for the development of effective treatment strategies. Finally, many child behaviors that are not classifiable as deviant at a particular point in time may nevertheless represent less extreme expressions or compensations of an already existing disorder or early expressions of a later progression to deviant extremes as development continues (Adelman, 1995). Therefore, any understanding of abnormality requires that we also attend to these less extreme problems. Future research on child psychopathology is likely to expand its focus on normal developmental processes, normative and representative community samples of children, and resilient children who show normal development despite adversity.
Context
Any consideration of disorders of childhood and adolescence needs to consider the social context in which these disorders develop (Boyce et al., 1998; Cicchetti & Aber, 1998). Children’s development and behavior changes rapidly such that descriptions taken at one point in time or in one context may yield information very different from that taken at other times or in other contexts. Understanding context requires a consideration of both proximal and distal events. Among these are events that impinge directly on the child in a particular situation at a particular point in time, extrasituational events that affect the child indirectly (e.g., a parent’s workrelated stress), and temporally remote events that continue to affect the child through their representation in memory. Defining context has been—and continues to be—a matter of some complexity (Mischel, 1968). For example, contextual events such as stress (Compas, Connor-Smith, Saltzman, Thomsen, & Wadsworth, 2001) and maltreatment (Wolfe, 1999) have been defined in numerous ways. Contexts for the development of psychopathology encompass heterogeneous sets of circumstances whose effects are likely to vary as a function of the configuration of these circumstances over time, when and where outcomes are assessed, and the specific domains of development that are affected.
Comorbidity
Comorbidity refers to the manifestation of two or more disorders whose co-occurrence is greater than what would be expected by chance alone. As we saw for ADHD and anxiety disorders, supposedly distinct forms of psychopathology often co-occur in the same child (Angold, Costello, & Erkanli, 1999). In fact, rates of comorbidity as high as 50% have been reported in community samples, with even higher rates in clinical samples (Caron & Rutter, 1991).
Although research has become increasingly sensitive to the occurrence and pattern of co-occurring disorders, less attention has been given to the mechanisms underlying these associations (Rutter & Sroufe, 2000). At least some of the overlap may be due to sampling biases or false assumptions about diagnostic categories and boundaries (e.g., viewing anxiety disorders as distinct conditions rather than as overlapping conditions or as different points in the progression of the same disorder). Alternatively, both disorders may result from the same set of risk factors—for example, genetic risk or maternal psychopathology; or the presence of one disorder may predispose the child to developing another—for example, when the presence of early ADHD disrupts family relations and leads to later CD (Johnston & Mash, 2001). Comorbidity in childhood disorders may also be partly a function of developmental level—that is, of underlying processes that have not yet achieved full differentiation (Lilienfeld, Waldman, & Israel, 1994). Finally, differing rates of comorbidity with age may reflect the fact that the appearance of one disorder or problem may precede the appearance of another—for example, inattention preceding impulsivity or anxiety preceding depression (Brady & Kendall, 1992).
Because the presence and patterning of comorbidity can easily distort or confuse how findings are interpreted, a better understanding of the mechanisms underlying these associations may serve to increase our understanding of both the disorders of interest as well as related risk and protective factors. Whatever ambiguities surround the construct of comorbidity, the fact that many disorders cluster together has important implications for how child psychopathology is conceptualized and treated (Kazdin & Kagan, 1994). For example, the presence of certain comorbid conditions has been found to influence the effectiveness of both behavioral and pharmacological interventions in children with ADHD (Jensen et al., 2001).
Prevalence
Prevalence estimates for most childhood disorders are directly related to changing diagnostic practices and trends. Earlier versions of DSM (APA, 1952, 1968) contained few separate child categories, and many forms of child psychopathology were constructed, so to speak, with the introduction of DSM-III in 1980 (APA, 1980) and reconstructed in subsequent revisions. For example, empirical findings in the 1980s did not support the category of attention deficit disorder without hyperactivity as a unique symptom cluster (Routh, 1990). As a result, this category was not included in DSM-III-R; however, as a result of new findings, it appeared in DSM-IV as the predominantly inattentive subtype. Similarly, several of the DSM-III-R categories for anxiety disorders for children changed in DSM-IV, lost their status as an independent category for children, or were dropped entirely (e.g., overanxious disorder; Albano et al., 1996).
Changes in diagnostic criteria based on new findings and other considerations (e.g., eligibility for services) are likely to continue to influence prevalence estimates. For example, current estimates of autism are about three times higher than previous ones (Fombonne, 1999; Tanguay, 2000), and this increase is primarily due to a broadening of the criteria used to diagnose autism and an increased recognition of milder forms of the disorder (Bryson & Smith, 1998; Gillberg & Wing, 1999). There is also ongoing debate about whether Asperger’s disorder is a variant of autism or simply describes higher-functioning individuals with autism (Schopler, Mesibov, & Kunce, 1998; Volkmar & Klin, 2000). The resolution of this debate and prevalence estimates for both autism and Asperger’s disorder will depend on how the diagnosis of Asperger’s disorder is used, because no official definition for this disorder existed until it was introduced in DSM-IV-TR (Volkmar & Klin, 1998).
The most consistent conclusions to be drawn from epidemiological findings are that prevalence rates for childhood problems are generally high but that rates vary as a result of several factors. These include the criteria used to define the problem; the nature of the disorder; the age, gender, social class, and ethnicity of the child; the method and source of information; and sampling considerations such as the settings in which children are identified.
Gender Differences
There are important differences in the prevalence, expression, accompanying disorders, underlying processes, outcomes, and developmental course of psychopathology in boys versus girls (Eme, 1979, 1992; Hops, 1995; Zahn-Waxler, 1993). ADHD, autism, childhood disruptive behavior disorders, and learning and communication disorders are all more common in boys than in girls, whereas the opposite is true for most anxiety disorders, adolescent depression, and eating disorders (Hartung & Widiger, 1998). Although gender differences are well established, the meaning of these differences is not well understood. For example, it is difficult to determine whether observed gender differences are a function of referral or reporting biases, the way in which disorders are currently defined, differences in the expression of the disorder (e.g., direct vs. indirect aggressive behavior), or sex differences in biological characteristics and environmental susceptibilities. All are possible, and there is a need for research into the processes underlying these gender differences. Clearly the mechanisms and causes of gender differences may vary for different disorders (e.g., ADHD vs. depression) or for the same disorder at different ages—for example, child versus adolescent OCD or earlyversus late-onset CD.
Boys show greater difficulties than girls do during early or middle childhood—particularly with respect to disruptive behavior disorders. Girls’ problems may increase during adolescence, with higher prevalence rates from midadolescence through adulthood. For example, conduct disorders and hyperactivity have been found to be more frequent in 12- to 16-year-old boys than they are in girls, whereas emotional problems have been found to be more frequent for girls than they are for boys in this age group (Boyle et al., 1987; Offord et al., 1987). Additionally, early signs of aggression have been found to predict later antisocial behavior for boys but not for girls (Tremblay et al., 1992).
Girls are less likely than boys are to be identified as having problems, largely due to sampling biases in which boys, who are more severely disruptive, are also more likely to be referred and studied (Spitzer, Davies, & Barkley, 1990). As a result, there is a predominance of externalizing problems in boys and of internalizing problems in adolescent girls in samples of children who are referred for treatment, but these differences are less in nonreferred samples of children (Achenbach, Howell, Quay, & Conners, 1991). Different factors may also be associated with psychopathology in boys versus girls. For example, in a population-based sample of 9- to 15-year-olds, headaches were associated with depression and anxiety in girls, but with conduct disorder in boys (Egger, Angold, & Costello, 1998). In addition, the types of child-rearing environments predicting resilience to adversity may differ for boys and girls. Resilience in boys is associated with households in which there is a male model (e.g., father, grandfather, older sibling), structure, rules, and some encouragement of emotional expressiveness. In contrast, resilient girls come from households that combine risk taking and independence with support from a female caregiver (e.g., mother, grandmother, older sister; Werner, 1995).
Although the prevalence of disruptive behavior is lower in girls than in boys, the risk of comorbid conditions such as anxiety is higher in girls. It may be that girls’heightened level of interpersonal sensitivity, caring, and empathy serves as a protective factor in insulating them from developing antisocial behavior. At the same time, however, girls’ overreceptivity to the plight of others and their reluctance to assert their own needs in situations involving conflict and distress may elevate their risk for the development of internalizing problems (Zahn-Waxler, Cole, Welsh, & Fox, 1995).
Socioeconomic Status
Although most children with mental health problems are from the middle class, mental health problems are disproportionately represented among the very poor. About 20% or more of children in the United States and Canada are living in poverty, and a significant number of them display impairments in their social, behavioral, and academic functioning. The impact of socioeconomic disadvantage on children derives from the fact that SES is a composite variable that includes many potential sources of negative influence. In addition to low income, low SES is often accompanied by low maternal education, a low level of employment, single-parent status, limited resources, and negative life events (e.g., poor nutrition, exposure to violence). Because overall indexes of SES may include one or more of these variables in any given study, the relationship that is reported between SES and child psychopathology may vary as a function of the particular index used as well as of racial and ethnic factors (McLeod & Nonnemaker, 2000).
Lower-SES children have been reported to display more psychopathology and other problems than do upper-SES children (e.g., Hollingshead & Redlich, 1958). However, although the reported relationships between SES and child psychopathology are statistically significant, the effects are small and should be interpreted cautiously (Achenbach et al., 1991). More important is that global estimates of SES often tell us little about the associated processes through which SES exerts its influence on the child. Knowledge of such processes is needed to inform our understanding of the disorder. For example, the effects of SES on aggression can be explained mostly by stressful life events and by beliefs that are accepting of aggression (Guerra, Huesmann, Tolan, Van-Acker, & Eron, 1995).
Ethnicity and Culture
Despite the growing ethnic diversity of the North American population, ethnic representation in research studies and the study of ethnicity-related issues more generally have received relatively little attention in studies of child psychopathology, with most data drawn largely from European-American culture (Foster & Martinez, 1995). Research into child psychopathology has generally been insensitive to possible differences in prevalence, age of onset, developmental course, and risk factors related to ethnicity (Kazdin & Kagan, 1994). In addition, few studies have compared ethnic groups while controlling for other important variables such as SES, sex, age, and geographic region (Achenbach et al., 1991). In recent comparisons that have controlled for these variables African American and Hispanic American children are identified and referred at the same rates as other children, but they are much less likely to actually receive specialty mental health services or psychotropic medications (García Coll, & Garrido, 2000). White and Native American children have been found to display similar mental health problems with the exception of substance abuse, which has higher rates for Native American youngsters (Costello, Farmer, & Angold, 1999).
Some studies that have included a small number of African American children in their samples have reported somewhat higher rates of externalizing problems for this group (Costello, 1989; Velez, Johnson, & Cohen, 1989). However, other studies with much larger national samples that included non-Hispanic White, African-American, and Hispanic children have reported either no or very small differences related to race or ethnicity when SES, sex, age, and referral status were controlled for (Achenbach & Edelbrock, 1981; Achenbach et al., 1991; Lahey et al., 1995). Thus, although externalizing problems have been reported to be more common among African American children, this finding is probably an artifact related to SES. Externalizing disorder is associated with both ethnicity and with SES; furthermore, because there is an overrepresentation of minority-status children in low-SES groups in North America, caution must be exercised in interpreting the relationships among SES, ethnicity, and aggression (Guerra et al., 1995; Lahey et al., 1995).
In contrast to the mixed findings for conduct disorder, race has not been found to be strongly associated with risk for eating disorders (Leon, Fulkerson, Perry, & Early-Zald, 1995). However, Catalano et al. (1993) have reported different patterns of substance abuse related to ethnicity. More research is needed, but these and other findings suggest that the effects of ethnicity probably vary with the problem under consideration. As was the case for SES, global comparisons of the prevalence of different types of problems for different ethnic groups are not likely to be very revealing. On the other hand, studies into the processes that influence the form, associated factors, and outcomes of different disorders for various ethnic groups hold promise for increasing our understanding of the relationship between ethnicity and child psychopathology.
Recent conceptualizations have looked at ethnicity-related sources of stress such as stereotype threat and stereotype confirmation concern and own group conformity pressure. Research suggests that members of ethnic minority groups are not passive recipients of prejudice and discrimination (this is true of mental health labels too); rather, they actively attempt to make sense of and cope with multiple and distinct ethnicity-related threats (Contrada et al., 2000).
The values, beliefs, and practices that characterize a particular ethnocultural group contribute to the development and expression of childhood distress and dysfunction, which in turn are organized into categories through cultural processes that further influence their development and expression (Harkness & Super, 2000). Through shared views about causality and intervention, culture also structures the way in which people and institutions react to the child’s problems. Because the meaning of children’s social behavior is influenced by cultural beliefs and values, it is not surprising that the form, frequency, and predictive significance of different forms of child psychopathology vary across cultures or that cultural attitudes influence diagnostic and referral practices (Lambert & Weisz, 1992).
Cross-cultural research on child psychopathology would suggest that the expression and experience of mental disorders in children is not universal (Fisman & Fisman, 1999). Patterns of onset and duration of illness and the nature and relationship among specific symptoms vary from culture to culture and across ethnic groups within cultures (Hoagwood & Jensen, 1997). However, few studies have compared the attitudes, behaviors, and biological and psychological processes of children with mental disorders across different cultures. Such information is needed to understand how varying social experiences and contexts influence the expression, course, and outcome of different disorders across cultures. For example, greater social connectedness and support in more traditional cultures and greater access to resources and opportunities in industrialized societies are examples of mechanisms that may alter outcomes across cultures. Sensitivity to the role of cultural influences in child psychopathology has increased (Evans & Lee, 1998; Lopez & Guarnaccia, 2000) and is likely to continue to do so as globalization and rapid cultural change become increasingly more common (García Coll et al., 2000).
Causal Processes
As illustrated by the models we presented for ADHD and anxiety disorders, all forms of child psychopathology are influenced by multiple and complex interactional and transactional processes—between characteristics of the child and the changing environmental context for development and behavior—that unfold over time. This view has led to an increasingly integrative approach to the etiology of child psychopathology that recognizes the role of multiple causal processes, including neurobiological, psychological, social, and cultural influences (Rutter & Sroufe, 2000). Models based on this approach are complex—at times even overwhelming—but necessary if disorders of childhood and adolescence are to be understood (Cicchetti & Canon, 1999). Constraints on the amount of diversity that is possible and the fact that not all outcomes are equally likely makes the task of understanding individual patterns of adaptation and maladaptation during childhood and adolescence somewhat more manageable (Cicchetti & Sroufe, 2000).
Genetic, neurobiological, neurophysiological, and neuroanatomical evidence suggests a neurobiological basis for many childhood disorders, including ADHD, autistic disorder, adolescent depression, and OCD, to name a few. With respect to genetics, recent research using molecular genetics has identified specific genes for autism (International Molecular Genetic Study of Autism Consortium, 1998), ADHD (Kuntsi & Stevenson, 2000), and Rett’s disorder (Amir et al., 1999). The identification of specific genes has the potential to greatly enhance our understanding of a disorder as well as its specific components (Stodgell, Ingram, & Hyman, 2000). However, the initial steps in identifying a specific gene for any disorder address only a small part of the genetic risk. Similar searches will be needed to identify other genes, and multiple interacting genes are a far more likely cause than is a single gene (Rutter, 2000a). Genetic influences are probabilistic, not deterministic, and environmental and genetic factors are generally of about equal importance (Plomin & Rutter, 1998). Most forms of child psychopathology are polygenic, involving a number of susceptibility genes that interact with one another and with environmental influences to result in observed levels of impairment (State, Lombroso, Pauls, & Leckman, 2000).
As our discussion of ADHD illustrated, research on brain structure and function using neuroimaging procedures has identified specific brain regions for ADHD and many other disorders. Neuroimaging studies tell us that one region or another may be involved but they do not tell us why, and the findings for particular disorders are not always consistent from study to study, for children of different ages, or for boys versus girls. Research into specific neurotransmitters has also provided promising leads, although findings have also been inconsistent. One of the difficulties in research in this area is that most forms of child psychopathology often involve the same brain structures and neurotransmitters, making it difficult to assess the specificity of their contributions to particular disorders. Such findings may reflect the limitations of existing categorical diagnostic systems that we discussed earlier.
Child psychopathology research has increasingly focused on the role of the family system, the complex relationships within families, and the reciprocal influences among various family subsystems (Fiese, Wilder, & Bickham, 2000). There is a need to consider the processes occurring within disturbed families and the common and unique ways in which these processes affect both individual family members and subsystems. Within the family, the role of the mother-child and marital subsystems have received the most research attention to date, with less attention given to the role of siblings or fathers (Hetherington, Reiss, & Plomin, 1994; Phares & Compas, 1992).
Research into family processes and child psychopathology has not kept pace with family theory and practice. Family members are frequently viewed as either the causes of childhood disorders or as passive responders. An integrative perspective in which family members are viewed as partners in a complex process of reciprocal interaction is needed (Hinshaw & Cicchetti, 2000). To accomplish this end, there is a need for the development of sophisticated methodologies and valid measures that will capture the complex relationships that are operative in disturbed and normal family systems (Bray, 1995; Bray, Maxwell, & Cole, 1995). This task is complicated by a lack of consensus concerning how dysfunctional or healthy family functioning should be defined or what specific family processes are important to assess (Bray, 1994; Mash & Johnston, 1996).
Continuities and Discontinuities
Acentral issue for theory and research in child psychopathology concerns the continuity of disorders identified from one time to another and the relationship between child and adult disorders (Kazdin & Johnson, 1994; Rutter & Sroufe, 2000). Prior to the emergence of a disorder, certain pathways may suggest a failure to adapt to age-salient developmental tasks; this failure in turn increases the likelihood of later problems, given particular environmental events. Childhood disorders are not static entities, and many children experience periods of relapse, remission, or degrees of severity over the course of their development. The concept of developmental pathways is crucial for understanding continuities and discontinuities in psychopathology. A pathway defines the sequence and timing of behavioral continuities and transformations and relationships between successive behaviors (Loeber, 1991). Different pathways may lead to similar disorders (equifinality), and similar initial pathways may result in different disorders (multifinality), depending on the organization of the larger system in which they occur. The systematic delineation of developmental pathways, such as the ones that we presented for ADHD and anxiety disorders, attempts to capture the changing expressions of a given disorder and to assess causal process, the patterning of comorbid conditions over time, and diverse outcomes.
Evidence in support of the continuity between child and adult disorders is equivocal and depends on a number of methodological factors related to research design, assessment instruments, the nature of the study sample, and the type and severity of the disorder. In general, the literature suggests that child psychopathology is continuous with adult disorders for some but not all problems. Some evidence appears to favor the stability of externalizing problems over internalizing problems. However, previous findings may reflect the severity and pervasiveness of the disorders assessed, referral biases, and the fact that findings from longitudinal investigations of children with internalizing disorders are just beginning to accumulate.
Research has focused not only on continuities and discontinuities in childhood disorders but also on the identification of factors that predict them. One factor that has been studied in the context of CD is age of onset. It has been found that early onset of symptoms relates to higher rates and more serious antisocial acts over a longer period of time for both boys and girls. However, psychosocial variables that are present prior to and following onset may influence the seriousness and chronicity more than age of onset per se (Tolan & Thomas, 1995). An issue that needs to be addressed concerns whether early age of onset operates in a causal fashion for later problems—and if so, how?
Although research supports the notion of continuity of disorders, it does not support the continuity of identical symptoms over time (e.g., homotypic correspondence). Continuity over time for patterns of behavior rather than for specific symptoms is the norm. For example, although externalizing disorders in boys are stable over time, the ways in which these behavioral patterns are expressed change dramatically over the course of development (Olweus, 1979). Even with wide fluctuations in the expression of behavior over time, children may show consistency in the adaptive and maladaptive ways in which they organize their experiences and interact with the environment. For example, behavioral inhibition in infancy may affect later adjustment by influencing the way in which the child adapts to new and unfamiliar situations and the ensuing person-environment interactions over time. Certain genes and neural systems may also play a significant predisposing role in influencing the continuity of psychopathology (Pennington & Ozonoff, 1991). Discontinuities in observable behavior may obscure continuities in the mechanisms underlying observable behavior.
Given that developmental continuity is reflected in general patterns of organization over time rather than in isolated behaviors or symptoms, the relationships between early adaptation and later psychopathology are unlikely to be simple, direct, or uncomplicated. The links between early and later psychopathology are marked by continuities and by discontinuities. The degree of continuity or discontinuity will vary as a function of changing environmental circumstances and transactions between the child and environment that affect the child’s developmental trajectory.
Risk and Resilience
Resilience, which refers to successful adaptations in children who experience significant adversity has received a good deal of attention (Luthar, Cicchetti, & Becker, 2000). Early patterns of adaptation influence later adjustment in complex and reciprocal ways. Adverse conditions, early struggles to adapt, and failure to meet developmental tasks do not inevitably lead to a fixed and unchanging abnormal path. Rather, many different factors—including chance events and encounters—can provide turning points whereby success in a particular developmental task (e.g., educational advances, peer relationships) alters a child’s course onto a more adaptive trajectory. Conversely, there are numerous events and circumstances that may deflect the child’s developmental trajectory toward that of maladaptation (e.g., dysfunctional home environment, peer rejection, difficulties in school, parental psychopathology, intergenerational conflict).
Further attention needs to be directed to the conceptual and methodological problems that have plagued research on resilience (Luthar et al., 2000), not the least of which is the lack of a consistent vocabulary, conceptual framework, and methodological approach. It is particularly important to ensure that resilience is not defined as a universal, categorical, or fixed attribute of the child; individual children may be resilient in relation to some forms of environmental stress but not to others, and resilience may vary over time and across contexts. Rather than a direct causal pathway leading to a particular outcome, resilience involves ongoing interactions between risk and protective factors within the child and his or her environment. These factors need to be conceptualized as processes rather than as absolutes, because the same event or condition can operate as a protective or risk factor as a function of the overall context in which it occurs. More than a decade of research suggests that resilience is not indicative of any rare or special qualities of the child per se (i.e., the invulnerable child); rather, it is the result of the interplay of normal developmental processes such as brain development, cognition, caregiver-child relationships, regulation of emotion and behavior, and the motivation for learning (Masten, 2001).
Implications for Treatment and Prevention
As a result of the emergent concepts and findings discussed in this research paper, treatment approaches for children’s mental health problems have grown tremendously in sophistication and breadth over the past two decades (Mash & Barkley, 1998). Many interventions today combine the most effective approaches to particular problems in an ongoing, developmentally sensitive manner (Kazdin, 2000). Moreover, because children’s symptoms are often an expression of their unsuccessful attempts to adapt to their circumstances, more emphasis today is placed on the child’s family, school, and peers—not just on the child (Howard & Kendall, 1996). Accordingly, treatment goals often focus on building children’s skills for adapting to their social environment—skills that will facilitate long-term adjustment—not just on eliminating problem behaviors or reducing subjective distress in the short term.
Although many of the disorders discussed in this research paper begin early in life, accurate early identification is difficult. The reliability of many early symptoms such as social withdrawal, labile mood, and perceptual and cognitive disturbances in predicting later problems is in many cases unknown. Nevertheless, growing evidence for the early presence of subclinical symptoms for some childhood disorders (e.g., schizophrenia), the fact that certain symptoms (e.g., aggressive behavior) are known to predict later problems, and the early age of onset of many forms of child psychopathology have led to an increasing interest in prevention (Cicchetti, Rappaport, Sandler, & Weissberg, 2000). Prevention efforts for most forms of child psychopathology are now available, although their long-term effectiveness is still being evaluated; however, early findings are promising, suggesting that the early detection and treatment of childhood disorders may lead to a better prognosis and outcome in adolescence and adulthood (U.S. Public Health Service, 2001a).
Efforts to evaluate treatments for childhood disorders have intensified (Weisz, Donenberg, Han, &Weiss, 1995), resulting in several noteworthy conclusions based on carefully controlled research trials: (a) Changes achieved by children receiving psychotherapy are consistently greater than are those for children not receiving therapy; (b) the average child who is treated is better off at the end of therapy than at least 75% of those children who did not receive treatment; (c) treatments have been shown to be equally effective for children with internalizing and externalizing disorders; (d) treatments are producing focused changes in targeted areas such as anxiety, rather than producing nonspecific or global effects such as changes in how the child feels (Kazdin, 1996; Weisz, 1998; Weisz & Weiss, 1993); and (e) the more outpatient therapy sessions children receive, the more improvement is seen in their symptoms (Angold, Costello, Burns, Erkanli, & Farmer, 2000).
In contrast to these findings for research therapy, however, studies of clinic therapy (i.e., in real-world settings) have resulted in less favorable outcomes (Andrade, Lambert, & Bickman, 2000; Weiss, Catron, Harris, & Phung, 1999; Weisz et al., 1995; for exceptions, see study by Angold et al., 2000; and meta-analytic review by Shadish, Matt, Navarro, & Phillips, 2000). These findings suggest that conventional services for children may be of limited effectiveness and that integrating these commonly used interventions into more coordinated systems of care also shows minimal support for the beneficial effects of treatment (Weisz, 1998). However, few studies exist of child therapy outcomes in settings where treatment is typically conducted; thus, it is premature to draw any conclusions from the findings from clinic and community studies until more empirical data about therapy in practice are available (Shadish et al., 1997). In order to address the differences in findings from research versus clinic studies, there is a growing interest in the development and evaluation of treatment strategies that reflect decision-making and service delivery as it occurs in clinical practice settings (T. D. Borkovec, 2001; Weisz, 2000a, 2000b).
Bibliography:
- Abikoff, H., Courtney, M., Pelham, W., & Koplewicz, H. (1993). Teachers’ ratings of disruptive behaviors: The influence of halo effects. Journal of Abnormal Child Psychology, 21, 519–533.
- Achenbach, T. M. (2000). Assessment of psychopathology. In A. J. Sameroff & M. Lewis (Eds.), Handbook of developmental psychopathology (2nd ed., pp. 41–56). New York: Kluwer Academic/Plenum Publishers.
- Achenbach, T. M., & Edelbrock, C. (1981). Behavioral problems and competencies reported by parents of normal and disturbed children aged four through sixteen. Monographs of the Society for Research in Child Development, 46(Serial No. 188, Whole No. 1).
- Achenbach, T. M., Howell, C. T., Quay, H. C., & Conners, C. K. (1991). National survey of problems and competencies among four- to sixteen-year-olds: Parents’ reports for normative and clinical samples. Monographs of the Society for Research in Child Development, 56(Serial No. 225, Whole No. 3).
- Adelman, H. S. (1995). Clinical psychology: Beyond psychopathology and clinical interventions. Clinical Psychology: Science and Practice, 2, 28–44.
- Albano, A. M., Chorpita, B. F., & Barlow, D. H. (1996). Childhood anxiety disorders. In E. J. Mash & R. A. Barkley (Eds.), Child psychopathology (pp. 196–241). New York: Guilford Press.
- Albano, A. M., Knox, L. S., & Barlow, D. H. (1995). Obsessivecompulsive disorder. In A. R. Eisen, C. A. Kearney, & C. A. Schaefer (Eds.), Clinical handbook of anxiety disorders in children and adolescents (pp. 282–316). Northvale, NJ: Jason Aronson.
- Amaya-Jackson, L., & March, J. S. (1995). Posttraumatic stress disorder. In J. S. March (Ed.), Anxiety disorders in children and adolescents (pp. 276–300). New York: Guilford Press.
- American Psychiatric Association. (1952). Diagnostic and statistical manual of mental disorders. Washington, DC: Author.
- American Psychiatric Association. (1968). Diagnostic and statistical manual of mental disorders (2nd ed.). Washington, DC: Author.
- American Psychiatric Association. (1980). Diagnostic and statistical manual of mental disorders (3rd ed.). Washington, DC: Author.
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., Text Revision). Washington, DC: Author.
- Amir, R. E., Van den Veyver, I. B., Wan, M., Tran, C. Q., Francke, U., & Zoghbi, H, Y. (1999). Rett Syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nature Genetics, 23, 185–188.
- Andrade, A. R., Lambert, E. W., & Bickman, L. (2000). Dose effect in child psychotherapy: Outcomes associated with negligible treatment. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 161–168.
- Andrews, G., Stewart, G., Allen, B., & Henderson, A. S. (1990). The genetics of six neurotic disorders: A twin study. Journal of Affective Disorders, 19, 23–29.
- Angold,A., Costello, J., Burns, B. J., Erkanli,A., & Farmer, E. M. Z. (2000). Effectiveness of nonresidential specialty mental health services for children and adolescents in the “real world.” Journal of the American Academy of Child and Adolescent Psychiatry, 39, 154–160.
- Angold, A., Costello, E., & Erkanli, A. (1999). Comorbidity. Journal of Child Psychology and Psychiatry, 40, 55–87.
- Applegate, B., Lahey, B. B., Hart, E. L., Biederman, J., Hynd, G. W., Barkley,R.A.,Ollendick,T.,Frick,P.J.,Greenhill,L.,McBurnett, , Newcorn, J. H., Kerdyk, L., Garfinkel, B., Waldman, I., & Shaffer, D. (1997). Validity of the age-of-onset criterion for ADHD: A report from the DSM-IV field trials. Journal of the AmericanAcademyofChildandAdolescentPsychiatry,36,1211– 1221.
- Arkowitz, H. (1992). Integrative theories of therapy. In D. K. Freedheim (Ed.), History of psychotherapy: A century of change (pp. 261–303). Washington, DC: American Psychological Association.
- Arnold, L. E. (1996). Sex differences in ADHD: Conference summary. Journal of Abnormal Child Psychology, 24, 555–569.
- Baker, L., & Cantwell, D. P. (1992). Attention deficit disorder and speech/language disorders. Comprehensive Mental Health Care, 2, 3–16.
- Barkley, R. A. (1988). The effects of methylphenidate on the interactions of preschool ADHD children with their mothers. Journal of the American Academy of Child and Adolescent Psychiatry, 27, 336–341.
- Barkley, R. A. (1996). Attention-deficit/hyperactivity disorder. In E. J. Mash & R. A. Barkley (Eds.), Child psychopathology (pp. 63–112). New York: Guilford Press.
- Barkley, R. A. (1997). ADHD and the nature of self-control. New York: Guilford Press.
- Barkley, R. A. (1998). Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment (2nd ed.). New York: Guilford Press.
- Barkley, R. A., & Biederman, J. (1997). Toward a broader definition of the age-of-onset criterion for attention-deficit-hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 1204–1210.
- Barkley, R. A., Fischer, M., Edelbrock, C. S., & Smallish, L. (1990). The adolescent outcome of hyperactive children diagnosed by research criteria: I. An 8-year prospective follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry, 29, 546–557.
- Barkley, R. A., Fischer, M., & Fletcher, K. (1997). Young adult outcome of hyperactive children diagnosed by research criteria. NIMH Grant, University of Massachusetts Medical Center.
- Barkley, R. A., Grodzinsky, G., & DuPaul, G. J. (1992). Frontal lobe functions in attention deficit disorder with and without hyperactivity: A review and research report. Journal of Abnormal Child Psychology, 20, 163–188.
- Barlow, D. H. (1988). Anxiety and its disorders: The nature and treatment of anxiety and panic. New York: Guilford Press.
- Baron-Cohen, S. (2000). Is Asperger syndrome/high functioning autism necessarily a disability? Development and Psychopathology, 12, 489–500.
- Barrett, P. M., Rapee, R. M., Dadds, M. M., & Ryan, S. M. (1996). Family enhancement of cognitive style in anxious and aggressive children. Journal of Abnormal Child Psychology, 24, 187– 203.
- Beidel, D. C., & Turner, S. M. (1997). At risk for anxiety: I. Psychopathology in the offspring of anxious parents. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 918–924.
- Beidel, D. C., Turner, S. M., & Morris, T. L. (1999). Psychopathology of childhood social phobia. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 643–650.
- Benjamin, J., Li, L., Patterson, C., Greenberg, B. D., Murphy, D. L., & Hamer, D. H. (1996). Population and familial association between the D4 dopamine receptor gene and measures of novelty seeking. Nature Genetics, 12, 81–84.
- Bernstein, G. A. (1991). Comorbidity and severity of anxiety and depressive disorders in a clinic sample. Journal of the American Academy of Child and Adolescent Psychiatry, 30, 43–50.
- Bernstein, G. A., Borchardt, C. M., & Perwien, A. R. (1996). Anxiety disorders in children and adolescents: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 1110–1119.
- Biederman, J., Faraone, S. V., & Lapey, K. (1992). Comorbidity of diagnosis in attention-deficit hyperactivity disorders. In G. Weiss (Ed.), Child and adolescent psychiatric clinics of North America: Attention-deficithyperactivitydisorder(pp.335–360).Philadelphia: Saunders.
- Biederman, J., Faraone, S. V., Mick, E., Williamson, S., Wilens, T. E., Spencer, T. J., Weber, W., Jetton, J., Kraus, I., Pert, J., & Zallen, B. (1999). Clinical correlates of ADHD in females: Findings from a large group of girls ascertained from pediatric and psychiatric referral sources. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 966–975.
- Biederman, J., & Spencer, T. (1999). Attention-deficit/hyperactivity disorder (ADHD) as a noradrenergic disorder. Biological Psychiatry, 46, 1234–1242.
- Biederman, J., Wozniak, J., Kiely, K., Ablon, S., Faraone, S., Mick, E., Mundy, E., & Kraus, I. (1995). CBCL clinical scales discriminate prepubertal children with structured-interviewderived diagnosis of mania from those with ADHD. Journal of the American Academy of Child and Adolescent Psychiatry, 34, 464–471.
- Borkovec, T. D. (2001, winter). Scientifically rigorous research in the practice setting: Practice research networks. Clinical Science Newsletter (winter), 2–3.
- Borkovec, T. M., & Inz, J. (1990). The nature of worry in generalized anxiety disorder: A predominance of thought activity. Behaviour Research and Therapy, 28, 153–158.
- Boyce, W. T., Frank, E., Jensen, P. S., Kessler, R. C., Nelson, C. A., & Stenberg, L. (1998). Social context in developmental psychopathology: Recommendations for future research from the MacArthur Network on Psychopathology and Development. Development and Psychopathology, 10, 143–164.
- Boyle, M. H., Offord, D. R., Hoffman, H. G., Catlin, G. P., Byles, A., Cadman, D. T., Crawford, J. W., Links, P. S., Rae-Grant, N. I., & Szatmari, P. (1987). Ontario Child Health Study: I. Methodology. Archives of General Psychiatry, 44, 826–831.
- Brady, E., & Kendall, P. C. (1992). Comorbidity of anxiety and depression in children and adolescents. Psychological Bulletin, 3, 244–255.
- Bray, J. H. (1994). Family assessment: Current issues in evaluating families. Unpublished manuscript, Department of Family Medicine, Baylor College of Medicine, Houston, TX.
- Bray, J. H. (1995). Methodological advances in family psychology research: Introduction to the special section. Journal of Family Psychology, 9, 107–109.
- Bray, J. H., Maxwell, S. E., & Cole, D. (1995). Multivariate statistics for family psychology research. Journal of Family Psychology, 9, 144–160.
- Bryson, S. E., & Smith, I. M. (1998). Epidemiology of autism: Prevalence, associated characteristics, and implications for research and service delivery. Mental Retardation and Developmental Disabilities Research Reviews, 4, 97–103.
- Burns, B. J., Costello, E. J., Angold, A., Tweed, D., Stangl, D., Farmer, E. M. Z., & Erkanli, A. (1995). Data watch: Children’s mental health service use across service sectors. Health Affair, 14, 147–159.
- Burns, G. L., Walsh, J. A., Patterson, D. R., Holte, C. S., SomersFlanagan, R., & Parker, C. M. (1997). Internal validity of the disruptive behavior disorder symptoms: Implications from parent ratings for a dimensional approach to symptom validity. Journal of Abnormal Child Psychology, 25, 307–319.
- Campbell, S. B. (1990). Behavior problems in preschool children: Clinical and developmental issues. New York: Guilford Press.
- Campbell, S. B. (2000). Attention-deficit/hyperactivity disorder: A developmental view. In A. J. Sameroff, M. Lewis, & S. M. Miller (Eds.), Handbook of developmental psychopathology (2nd ed., pp. 383–401). New York: Kluwer Academic.
- Campbell, S. B., Shaw, D. S., & Gilliom, M. (2000). Early externalizing behavior problems: Toddlers and preschoolers at risk for later maladjustment. Development and Psychopathology, 12, 467–488.
- Cantwell, D. P., & Baker, L. (1992). Association between attention deficit-hyperactivity disorder and learning disorders. In S. E. Shaywitz & B. A. Shaywitz (Eds.), Attention deficit disorder comes of age: Toward the twenty-first century (pp. 145–164). Austin, TX: Pro-ed.
- Capps, L., Sigman, M., Sena, R., & Henker, B. (1996). Fear, anxiety and perceived control in children of agoraphobic parents. Journal of Child Psychology and Psychiatry, 37, 445–452.
- Carlson, G. A., Bromet, E. J., & Sievers, S. (2000). Phenomenology and outcome of subjects with early and adult-onset psychotic mania. American Journal of Psychiatry, 157, 213–220.
- Caron, C., & Rutter, M. (1991). Comorbidity in child psychopathology: Concepts, issues, and research strategies. Journal of Child Psychology and Psychiatry, 32, 1063–1080.
- Casey, B. J., Castellanos, F. X., Giedd, J. N., Marsh, W. L., Hamburger, S. D., Schubert, A. B., Vauss, Y. C., Vaituzis, A. C., Dickstein, D. P., Sarfetti, S. E., & Rapoport, J. L. (1997). Implication of right frontostriatal circuitry in response inhibition and attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 374–383.
- Catalano, R. F., Hawkins, J. D., Krenz, C., Gilmore, M., Morrison, D., Wells, E., & Abbott, R. (1993). Using research to guide culturally appropriate drug abuse prevention. Journal of Consulting and Clinical Psychology, 61, 804–811.
- Chambless, D. L., & Ollendick, T. H. (2001). Empirically supported psychological interventions: Controversies and evidence. Annual Review of Psychology, 52, 685–716.
- Chansky, T. E., & Kendall, P. C. (1997). Social expectancies and self-perceptions in anxiety-disordered children. Journal of Anxiety Disorders, 11, 347–363.
- Chorpita, B. F., & Barlow, D. H. (1998). The development of anxiety: The role of control in the early environment. Psychological Bulletin, 124, 3–21.
- Chorpita, B. F., Daleiden, E. L., Moffitt, C., Yim, L., & Umemoto, L. A. (2000). Assessment of tripartite factors of emotion in children and adolescents: I. Structural validity and normative data of an affect and arousal scale. Journal of Psychopathology and Behavioral Assessment, 23, 141–160.
- Cicchetti, D., & Aber, J. L. (Eds.). (1998). Contextualism and developmental psychopathology [Special issue]. Development and Psychopathology, 10, 137–426.
- Cicchetti, D., & Cannon, T. D. (1999). Neurodevelopmental processes in the ontogenesis and epigenesis of psychopathology. Development and Psychopathology, 11, 375–393.
- Cicchetti, D., & Cohen, D. J. (Eds.). (1995). Developmental psychopathology: Vol. 1. Theory and methods. New York: Wiley.
- Cicchetti, D., Rappaport, J., Sandler, I., & Weissberg, R. P. (Eds.). (2000). The promotion of wellness in children and adolescents. Washington, DC: Child Welfare League of America, Inc.
- Cicchetti, D., & Richters, J. E. (1993). Developmental considerations in the investigation of conduct disorder. Development and Psychopathology, 5, 331–344.
- Cicchetti, D., & Sroufe, L. A. (2000). Editorial: The past as prologue to the future: The times, they’ve been a-changin’. Development and Psychopathology, 12, 255–264.
- Cicchetti, D., & Toth, S. L. (2000). Social policy implications of research in developmental psychopathology, Developmental Psychopathology, 12, 551–554.
- Cohen, M. (1998). The monetary value of saving a high risk youth. Journal of Quantitative Criminology, 14, 5–34.
- Cohen, P., Cohen, J., & Brook, J. S. (1993).An epidemiological study ofdisordersinlatechildhoodandadolescence:II.Persistenceofdisorders. Journal of Child Psychology and Psychiatry, 34, 869–877.
- Cohen, N. J., Vallance, D. D., Barwick, M., Im, N., Menna, R., Horodezky, N. B., & Isaacson, L. (2000). The interface between ADHD and language impairment: An examination of language, achievement, and cognitive processing. Journal of Child Psychology and Psychiatry, 41, 353–362.
- Cole, D. A., Martin, J. M., Peeke, L., Henderson, A., & Harwell, J. (1998). Validation of depression and anxiety measures in White and Black youths: Multitrait-multimethod analyses. Psychological Assessment, 10, 261–276.
- Cole, D. A., Peeke, L., Martin, Truglio, & Seroczynski, A. D. (1998). A longitudinal look at the relation between depression and anxiety in children and adolescents. Journal of Consulting and Clinical Psychology, 66, 451–460.
- Cole, D. A., Truglio, R., & Peeke, L. (1997). Relation between symptoms of anxiety and depression in children: A multitraitmultimethod-multigroup assessment. Journal of Consulting and Clinical Psychology, 65, 110–119.
- Compas, B. E., Connor-Smith, J. K., Saltzman, H., Thomsen, A. H., & Wadsworth, M. E. (2001). Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin, 127, 87–127.
- Compas, B. E., & Oppedisano, G. (2000). Mixed anxiety/depression in children and adolescents. In A. J. Sameroff, M. Lewis, & S. M. Miller (Eds.), Handbook of developmental psychopathology (2nd ed., pp. 531–548). New York: Kluwer Academic.
- Compton, S. N., Nelson, A. H., & March, J. S. (2000). Social phobia and separation anxiety symptoms in community and clinical samples of children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 1040–1046.
- Contrada, R. J.,Ashmore, R. D., Gary, M. L., Coups, E., Egeth, J. D., Sewell,A., Ewell, K., Goyal, T. M., & Chasse, V. (2000). Ethnicity-related sources of stress and their effects on well-being. Current Directions in Psychological Science, 9, 136–139.
- Cook, E. H., Stein, M. A., Krasowski, M. D., Cox, N. J., Olkon, D. M., Kieffer, J. E., & Leventhal, B. L. (1995). Association of attention-deficit disorder and the dopamine transporter gene. American Journal of Human Genetics, 56, 993–998.
- Corkum, P., Tannock, R., & Moldofsky, H. (1988). Sleep disturbances in children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 37, 637–646.
- Costello, E. J. (1989). Developments in child psychiatric epidemiology. Journal of the American Academy of Child and Adolescent Psychiatry, 28, 836–841.
- Costello, E. J., & Angold, A. C. (2000). Developmental epidemiology: A framework for developmental psychopathology. In A. Sameroff, M. Lewis, & S. Miller (Eds.), Handbook of developmental psychopathology (2nd ed., pp. 57–73). New York: Plenum.
- Costello, E. J., Farmer, E. M. Z., & Angold, A. (1999). Same place, different children: White and American Indian children in the Appalachian mountains. In P. Cohen & C. Slomkowski (Eds.), Historical and geographical influences on psychopathology (pp. 279–298). Mahwah, NJ: Erlbaum.
- Costello, E. J., Farmer, E. M. Z., Angold, A., Burns, B. J., & Erkanli, A. (1997). Psychiatric disorders among American Indian and white youth in Appalachia: The Great Smoky Mountains Study. American Journal of Public Health, 87, 827–832.
- Craske, M. G., & Rowe, M. K. (1997). Nocturnal panic. Clinical Psychology: Science and Practice, 4, 153–174.
- Daly, J. M., Biederman, J., Bostic, J. Q., Maraganore, A. M., Lelon, E., Jellinek, M., & Lapey, A. (1996). The relationship between childhood asthma and attention deficit hyperactivity disorder: A review of the literature. Journal of Attention Disorders, 1, 31–40.
- Dawson, G., Ashman, S. B., & Carver, L. J. (2000). The role of early experience in shaping behavioral and brain development and its implications for social policy. Development and Psychopathology, 12, 695–712.
- Dawson, G., Hessl, D., & Frey, K. (1994). Social influences on early developing biological and behavioral systems related to risk for affective disorder. Development and Psychopathology, 6, 759– 779.
- DiLalla, L. F., Kagan, J., & Reznick, J. S. (1994). Genetic etiology of behavioral inhibition among 2-year-old children. Infant Behavior and Development, 17, 405–412.
- Douglas, V. I. (1999). Cognitive control processes in attention deficit/hyperactivity disorder. In H. C. Quay & A. E. Hogan (Eds.), Handbook of disruptive behavior disorders (pp. 105– 138). New York: Kluwer Academic.
- Dumas, M. C. (1998). The risk of social interaction problems among adolescents with ADHD. Education & Treatment of Children, 21, 447–460.
- Duncan, G. J., Brooks-Gunn, J., & Klebanov, P. K. (1994). Economic deprivation and early-childhood development. Child Development, 65, 296–318.
- DuPaul, G. J., McGoey, K. E., Eckert, T. L., & VanBrakle, J. (2001). Preschool children with attention-deficit/hyperactivity disorder: Impairments in behavioral, social, and school functioning. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 508–515.
- Ebstein, R. P., Novick, O., Umansky, R., Priel, B., Osher, Y., Blaine, D., Bennett, E. R., Nemanov, L., Katz, M., & Belmaker, R. H. (1996). Dopamine D4 receptor (D4DR) exon III polymorphism associated with the human personality trait of novelty seeking. Nature Genetics, 12, 78–80.
- Edelbrock, C. S., Rende, R., Plomin, R., & Thompson, L. A. (1995). A twin study of competence and problem behavior in childhood and early adolescence. Journal of Child Psychology and Psychiatry, 36, 775–786.
- Egger, H. L., Angold, A., & Costello, E. J. (1998). Headaches and psychopathology in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 37, 951–958.
- Eiraldi, R. B., Power, T. J., & Nezu, C. M. (1997). Patterns of comorbidity associated with subtypes of attention-deficit/ hyperactivity disorder among 6- to 12-year-old children. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 503–514.
- Eley, T. C. (1999). Behavioral genetics as a tool for developmental psychology: Anxiety and depression in children and adolescents. Clinical Child and Family Psychology Review, 2, 21–36.
- Eme, R. F. (1979). Sex differences in child psychopathology: A review. Psychological Bulletin, 86, 574–595.
- Eme, R. F. (1992). Selective female affliction in development of disorders of childhood: A literature review. Journal of Clinical Child Psychology, 21, 354–364.
- Erhardt, D., & Hinshaw, S. P. (1994). Initial sociometric impressions of attention-deficit hyperactivity disorder and comparison boys: Predictions from social behaviors and from nonbehavioral variables. Journal of Consulting and Clinical Psychology, 62, 833–842.
- Ernst, M., Liebenauer, M. A., King, C., Fitzgerald, G. A., Cohen, R. M., & Zametkin, A. J. (1994). Reduced brain metabolism in hyperactive girls. Journal of the Academy of Child and Adolescent Psychiatry, 33, 858–868.
- Essau, C. A., Conradt, J., & Petermann, F. (1999). Frequency and comorbidity of social phobia and social fears in adolescents. Behaviour Research and Therapy, 37, 831–843.
- Essau, C. A., Conradt, J., & Petermann, F. (2000). Frequency, comorbidity, and psychosocial impairment of specific phobia in adolescents. Journal of Clinical Child Psychology, 29, 221–231.
- Evans, B., & Lee, B. K. (1998). Culture and child psychopathology. In S. S. Kazarian & D. R. Evans (Eds.), Cultural clinical psychology: Theory, research, and practice (pp. 289–315). New York: Oxford University Press.
- Famularo, R., Fenton, T., Kinscherff, R., & Augustyn, M. (1996). Psychiatric comorbidity in childhood posttraumatic stress disorder. Child Abuse and Neglect, 20, 953–961.
- Faraone, S. V., & Beiderman, J. (1998). Neurobiology of attention deficithyperactivitydisorder.BiologicalPsychiatry,44,951–958.
- Faraone, S. V., Biederman, J., Chen, W. J., Krifcher, B., Keenan, K., Moore, C., Sprich, S., & Tsuang, M. T. (1992). Segregation analysis of attention deficit hyperactivity disorder. Psychiatric Genetics, 2, 257–275.
- Faraone, S. V., Biederman, J., Feighner, J. A., & Monuteaux, M. C. (2000). Assessing symptoms of attention deficit hyperactivity disorder in children and adults: Which is more valid? Journal of Consulting and Clinical Psychology, 68, 830–842.
- Faraone, S. V., Biederman, J., & Friedman, D. (2000). Validity of DSM-IV subtypes of attention-deficit/hyperactivity disorder: A family study perspective. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 300–307.
- Faraone,S.V.,Biederman,J.,&Milberger,S.(1996).Anexploratory study of ADHD among second degree relatives of ADHD children. Society of Biological Psychiatry, 35, 398–402.
- Faraone, S. V., Biederman, J., Weiffenbach, B., Keith, T., Chu, M. P., Weaver, A., Spencer, T. J., Wilens, T. E., Frazier, J., Cleves, M., & Sakai, J. (1999). Dopamine D-sub-4 gene 7-repeat allele and attention deficit hyperactivity disorder. American Journal of Psychiatry, 156, 768–770.
- Fiese, B. H., Wilder, J., & Bickham, N. L. (2000). Family context in developmental psychopathology. In A. J. Sameroff, M. Lewis, & S. M. Miller (Eds.), Handbook of developmental psychopathology (2nd ed., pp. 115–134). New York: Kluwer Academic.
- Filipek, P. A., Semrud-Clikeman, M., Steingard, R. J., Renshaw, P. F., Kennedy, D. N., & Beiderman, J. (1997). Volumetric MRI analysis comparing subjects having attention-deficit hyperactivity disorder with controls. Neurology, 48, 589–601.
- Fischer, M., Barkley, R. A., Edelbrock, C. S., & Smallish, L. (1990). The adolescent outcome of hyperactive children diagnosed by research criteria: II. Academic, attentional, and neuropsychological status.JournalofConsultingandClinicalPsychology,58,580–588.
- Fisman, S., & Fisman, R. (1999). Cultural influences on symptom presentation in childhood. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 782–783.
- Fletcher, K. E. (1996). Childhood posttraumatic stress disorder. In E. J. Mash & R. A. Barkley (Eds.), Child psychopathology (pp. 242–276). New York: Guilford Press.
- Fombonne, E. (1999). The epidemiology of autism: A review. Psychological Medicine, 29, 769–786.
- Foster, S. L., & Martinez, C. R., Jr. (1995). Ethnicity: Conceptual and methodological issues in child clinical research. Journal of Clinical Child Psychology, 24, 214–226.
- Garber, J. (1984). Classification of childhood psychopathology: A developmental perspective. Child Development, 55, 30–48.
- García Coll, C., Akerman, A., & Cicchetti, D. (2000). Cultural influence on developmental processes and outcomes: Implications for the study of development and psychopathology. Development and Psychopathology, 12, 333–356.
- García Coll, C., & Garrido, M. (2000). Minorities in the United States: Sociocultural context for mental health and developmental psychopathology. In A. J. Sameroff, M. Lewis, & S. M. Miller (Eds.), Handbook of developmental psychopathology (2nd ed., 177–195). New York: Kluwer Academic.
- Gaub, M., & Carlson, C. L. (1997a). Behavioral characteristics of DSM-IV subtypes in a school-based population. Journal of Abnormal Child Psychology, 25, 103–111.
- Gaub, M., & Carlson, C. L. (1997b). Gender differences in ADHD: A meta-analysis and critical review. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 1036–1045.
- Ge, X., Conger, R. D., Lorenz, F. O., Shanahan, M., & Elder, G. H., Jr. (1995). Mutual influences in parent and adolescent distress. Developmental Psychology, 31, 406–419.
- Geller, B., & Luby, J. (1997). Child and adolescent bipolar disorder: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 1168–1176.
- Gilger, J. W., Pennington, B. F., & DeFries, J. C. (1992). A twin study of the etiology of comorbidity: Attention-deficit hyperactivity disorder and dyslexia. Journal of the American Academy of Child and Adolescent Psychiatry, 321, 343–348.
- Gill, M., Daly, G., Heron, S., Hawi, Z., & Fitzgerald, M. (1997). Confirmation of a dissociation between attention deficit hyperactivity disorder and a dopamine transporter polymorphism. Biological Psychiatry, 2, 311–313.
- Gillberg, C., & Wing, L. (1999). Autism: Not an extremely rare disorder. Acta Psychiatrica Scandinavica, 99, 399–406.
- Ginsburg, G., & Silverman, W. (1996). Phobic and anxiety disorders in Hispanic and Caucasian youth. Journal of Anxiety Disorders, 10, 517–528.
- Grattan, L. M., & Eslinger, P. J. (1991). Frontal lobe damage in children and adults: A comparative review. Developmental Neuropsychology, 7, 283–326.
- Greenbaum, P. E., Prange, M. E., Friedman, R. M., & Silver, S. E. (1991). Substance abuse prevalence and comorbidity with other psychiatric disorders among adolescents with severe emotional disturbances. Journal of the American Academy of Child and Adolescent Psychiatry, 30, 575–583.
- Greene, R. W., Biederman, J., Faraone, S. V., Monuteaux, M. C., Mick, E., DuPre, E. P., Fine, C. S., & Goring, J. C. (2001). Social impairment in girls with ADHD: Patterns, gender comparisons, and correlates. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 704–710.
- Gresham, F. M., MacMillan, D. L., Bocian, K. M., Ward, S. L., & Forness, S. R. (1998). Comorbidity of hyperactivity-impulsivityinattention and conduct problems: Risk factors in social, affective, and academic domains. Journal of Abnormal Child Psychology, 26, 393–406.
- Gruber, R., Sadeh, A., & Raviv, A. (2000). Instability of sleep patterns in children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 495–501.
- Guerra, N. G., Huesmann, L. R., Tolan, P. H., Van-Acker, R., & Eron, L. D. (1995). Stressful events and individual beliefs as correlates of economic disadvantage and aggression among urban children. Journal of Consulting and Clinical Psychology, 63, 518–528.
- Gurley, D., Cohen, P., Pine, D. S., & Brook, J. (1996). Discriminating depression and anxiety in youth: A role for diagnostic criteria. Journal of Affective Disorders, 39, 191–200.
- Halperin, J. M., Matier, K., Bedi, G., Sharma, V., & Newcorn, J. H. (1992). Specificity of inattention, impulsivity, and hyperactivity to the diagnosis of attention-deficit hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 190–196.
- Hanna, G. (1995). Demographic and clinical features of obsessivecompulsive disorder in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 34, 19–27.
- Harkness, S., & Super, C. M. (2000). Culture and psychopathology. In A. J. Sameroff, M. Lewis, & S. M. Miller (Eds.), Handbook of developmental psychopathology (2nd ed., pp. 197–214). New York: Kluwer Academic.
- Hart, E. L., Lahey, B. B., Loeber, R., Applegate, B., & Frick, P. J. (1996). Developmental change in attention-deficit hyperactivity disorder in boys: A four-year longitudinal study. Journal of Abnormal Child Psychology, 23, 729–749.
- Hartung, C. M., & Widiger, T. A. (1998). Gender differences in the diagnosis of mental disorders: Conclusions and controversies of DSM-IV. Psychological Bulletin, 123, 260–278.
- Hatch,M.L.,Friedman,S.,&Paradis,C.M.(1996).Behavioraltreatment of obsessive-compulsive disorder in African Americans. Cognitive and Behavioral Practice, 3, 303–315.
- Hechtman, L. (1994). Genetic and neurobiological aspects of attention deficit hyperactivity disorder: A review. Journal of Psychiatric Neurosciences, 19, 193–201.
- Henker, B., & Whalen, C. K. (1999). The child with attentiondeficit/hyperactivity disorder in school and peer settings. In H. C. Quay & A. E. Hogan (Eds.), Handbook of disruptive behavior disorders (pp. 157–178). New York: Kluwer Academic.
- Hetherington, E. M., Reiss, D., & Plomin, R. (Eds.). (1994). Separate social worlds of siblings: The impact of nonshared environment on development. Hillsdale, NJ: Erlbaum.
- Hinshaw, S. P. (1994). Attention deficits and hyperactivity in children. Thousand Oaks, CA: Sage.
- Hinshaw, S. P., & Cicchetti, D. (2000). Stigma and mental disorder: Conceptions of illness, public attitudes, personal disclosure, and social policy. Development and Psychopathology, 12, 555–598.
- Hirshfeld, D. R., Biederman, J., Brody, L., & Faraone, S. V. (1997). Associations between expressed emotion and child behavioral inhibition and psychopathology: Apilot study. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 205–213.
- Hirshfeld, D. R., Biederman, J., & Rosenbaum, J. F. (1997). Expressedemotiontowardchildrenwithbehavioralinhibition:Associations with maternal anxiety disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 910–919.
- Hirshfeld, D. R., Rosenbaum, J. F., Biederman, J., Bolduc, E. A., Faraone, S. V., Snidman, N., Reznick, J. S., & Kagan, J. (1992). Stable behavioral inhibition and its association with anxiety disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 103–111.
- Hoagwood, K., & Jensen, P. (1997). Developmental psychopathology and the notion of culture. Applied Developmental Science, 1, 108–112.
- Hoagwood, K., Kelleher, K. J., Feil, M., & Comer, D. M. (2000). Treatment services for children with ADHD: A national perspective. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 198–206.
- Hollingshead, A. B., & Redlich, F. C. (1958). Social class and mental illness. New York: Wiley.
- Hops, H. (1995). Age- and gender-specific effects of parental depression: Acommentary. Developmental Psychology, 31, 428– 431.
- Howard, B. L., & Kendall, P. C. (1996). Cognitive-behavioral family therapy for anxiety-disordered children: A multiple-baseline evaluation. Cognitive Therapy and Research, 20, 423–443.
- Humphries, T., Kinsbourne, M., & Swanson, J. (1978). Stimulant effects on cooperation and social interaction between hyperactive children and their mothers. Journal of Child Psychology and Psychiatry, 19, 12–22.
- Ialongo, N., Edelsohn, G., Werthamer-Larsson, L., Crockett, L., & Kellam, S. (1995). The significance of self-reported anxious symptoms in first grade children: Prediction to anxious symptoms and adaptive functioning in fifth grade. Journal of Child Psychology and Psychiatry, 36, 427–437.
- Inderbitzen-Nolan, H. M., & Walters, K. S. (2000). Social anxiety scale for adolescents: Normative data and further evidence of constructvalidity.JournalofClinicalChildPsychology,29,360– 371.
- International Molecular Genetic Study of Autism Consortium. (1998). A full genome screen for autism with evidence for linkage to a region on chromosome 7q. Human Molecular Genetics, 7, 571–578.
- Jacobvitz, D., & Sroufe, L. A. (1987). The early caregiver-child relationship and attention-deficit disorder with hyperactivity in kindergarten: A prospective study. Child Development, 58, 1496–1504.
- Jensen, P. S., Hinshaw, S. P., Kraemer, H. C., Lenora, N., Newcorn, J. H., Abikoff, H. B., March, J. S., Arnold, L. E., Cantwell, D. P., Connors, C. K., Elliott, G. R., Greenhill, L. L., Hechtman, L., Hoza, B., Pelham, W. E., Severe, J. B., Swanson, J. M., Wells, K. C., Wigal, T., & Vitiello, B. (2001). ADHD comorbidity findings from the MTA study: Comparing comorbid subgroups. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 147–158.
- Jensen, P. S., Kettle, L., Roper, R. S., Sloan, M. T., Dulcan, M. K., Hoven, C., Bird, H. R., Bauermeister, J. J., & Payne, J. D. (1999). Are stimulants overprescribed? Treatment of ADHD in four U.S. communities. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 797–804.
- Jensen, P. S., Martin, B. A., & Cantwell, D. P. (1997). Comorbidity in ADHD: Implications for research, practice, and DSM-IV. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 1065–1079.
- Johnston, C., & Mash, E. J. (2001). Families of children with Attention Deficit Hyperactivity Disorder: Review and recommendations for future research. Clinical Child and Family Psychology Review, 4, 183–207.
- Joiner, T. E., Jr., & Lonigan, C. J. (2000). Tripartite model of depression and anxiety in youth psychiatric inpatients: Relations with diagnostic status and future symptoms. Journal of Clinical Child Psychology, 29, 372–382.
- Kagan, J. (1997). Temperament and the reactions to unfamiliarity. Child Development, 68, 139–143.
- Kagan, J., & Snidman, N. (1999). Early child predictors of adult anxiety disorders. Biological Psychiatry, 46, 1536–1541.
- Kagan, J., Snidman, N., & Arcus, D. M. (1992). Initial reactions to unfamiliarity. Current Directions in Psychological Science, 1, 171–174.
- Kagan, J., Snidman, N., Arcus, D. M., & Reznick, J. S. (1994). Galen’s prophecy: Temperament in human nature. New York: Basic Books.
- Kazdin, A. E. (1996). Developing effective treatments for children and adolescents. In E. D. Hibbs & P. S. Jensen (Eds.), Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice (pp. 9–18). Washington, DC: American Psychological Association.
- Kazdin, A. E. (2000). Psychotherapy for children and adolescents: Directions for research and practice. New York: Oxford University Press.
- Kazdin, A. E. (2001). Bridging the enormous gaps of theory with therapy research and practice. Journal of Clinical Child Psychology, 30, 59–66.
- Kazdin, A. E., & Johnson, B. (1994). Advances in psychotherapy for children and adolescents: Interrelations of adjustment, development, and intervention. Journal of School Psychology, 32, 217– 246.
- Kazdin, A. E., & Kagan, J. (1994). Models of dysfunction in developmental psychopathology. Clinical Psychology: Science and Practice, 1, 35–52.
- Kearney, C. A., Albano, A. M., Eisen, A. R., Allan, W. D., & Barlow, D. A. (1997). The phenomenology of panic disorder in youngsters: An empirical study of a clinical sample. Journal of Anxiety Disorders, 11, 49–62.
- Kearney, C. A., & Allan, W. D. (1995). Panic disorder with or without agoraphobia. In A. R. Eisen, C. A. Kearney, & C. A. Schaefer (Eds.), Clinical handbook of anxiety disorders in children and adolescents (pp. 251–281). Northvale, NJ: Jason Aronson.
- Keller, M., Lavori, P., Wunder, J., Beardslee, W., Schwartz, C., & Roth, J. (1992). Chronic course of anxiety disorders in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 595–599.
- Kendall, P. C., & Brady, E. (1995). Comorbidity in the anxiety disorders of childhood. In K. Craig & K. Dobson (Eds.), Anxiety and depression in adults and children (pp. 3–36). Newbury Park, CA: Sage.
- Kendall, P. C., Panichelli-Mindel, S. M., Sugarman, A., & Callahan, S. A. (1997). Exposure to child anxiety: Theory, research, and practice. Clinical Psychology: Science and Practice, 4, 29–39.
- King, N. J., & Bernstein, G.A. (2001). School refusal in children and adolescents: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 197–205.
- King, N. J., Ollendick, T. H., & Mattis, S. G. (1994). Panic in children and adolescents: Normative and clinical studies. Australian Psychologist, 29, 89–93.
- Koplowicz, S., & Barkley, R. A. (1995). Sense of time in children with attention deficit hyperactivity disorder and normal children. Unpublished manuscript, University of Massachusetts Medical Center, Worcester.
- Kortlander, E., Kendall, P. C., & Panichelli-Mindel, S. M. (1997). Maternal expectations and attributions about coping in anxious children. Journal of Anxiety Disorders, 11, 297–315.
- Kovacs, M. (1997). Depressive disorders in childhood: An impressionistic landscape. Journal of Child Psychology and Psychiatry, 38, 287–298.
- Krain, A. L., & Kendall, P. C. (2000). The role of parental emotional distress in parent report of child anxiety. Journal of Clinical Child Psychology, 29, 328–335.
- Kuntsi, J., & Stevenson, J. (2000). Hyperactivity in children: A focus on genetic research and psychological theories. Clinical Child Family Psychology Review, 3, 1–23.
- La Greca, A. M., Silverman, W. K., & Wasserstein, S. B. (1998). Children’s predisaster functioning as a predictor of posttraumatic stress following Hurricane Andrew. Journal of Consulting and Clinical Psychology, 66, 883–892.
- Lahey, B. B., & Carlson, C. L. (1992). Validity of the diagnostic category of attention deficit disorder without hyperactivity: A review of the literature. In S. E. Shaywitz & B. A. Shaywitz (Eds.), Attention deficit disorder comes of age: Toward the twenty-first century (pp. 119–144). Austin, TX: Pro-ed.
- Lahey, B. B., Hartdagen, S. E., Frick, P. J., McBurnett, K., Connor, R., & Hynd, G. W. (1988). Conduct disorder: Parsing the confounded relationship between parental divorce and antisocial personality. Journal of Abnormal Psychology, 97, 334–337.
- Lahey, B. B., Loeber, R., Hart, E. L., Frick, P. J., Applegate, B., Zhang, Q., Green, S. M., & Russo, M. F. (1995). Four-year longitudinal study of conduct disorder in boys: Patterns and predictors of persistence. Journal of Abnormal Psychology, 104, 83–93.
- Lambert, N. M., Sandoval, J., & Sassone, D. (1978). Prevalence of hyperactivity in elementary school children as a function of social system definers. American Journal of Orthopsychiatry, 48, 446–463.
- Lambert, M. C., & Weisz, J. R. (1992). Jamaican and American adult perspectives on child psychopathology: Further exploration of the threshold model. Journal of Consulting and Clinical Psychology, 60, 146–149.
- Landau, S., Milich, R., & Diener, M. B. (1998). Peer relations of childrenwithattention-deficithyperactivitydisorder.Reading&Writing Quarterly: Overcoming Learning Difficulties, 14, 83–105.
- Last, C. G., & Perrin, S. (1993). Anxiety disorders in AfricanAmerican and white children. Journal of Abnormal Child Psychology, 21, 153–164.
- Last, C. G., Perrin, S., Hersen, M., & Kazdin, A. E. (1992). DSMIII-R anxiety disorders in children: Sociodemographic and clinical characteristics. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 1070–1076.
- Last, C. G., Perrin, S., Hersen, M., & Kazdin, A. E. (1996). A prospective study of childhood anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 1502–1510.
- Last, C. G., & Strauss, C. C. (1989). Panic disorder in children and adolescents. Journal of Anxiety Disorders, 3, 87–95.
- Leibson, C. L., Katusic, S. K., Barberesi, W. J., Ransom, J., & O’Brien, P. (2001). Use and costs of medical care for children and adolescents with and without attention-deficit/hyperactivity disorder (ADHD). Journal of the American Medical Association, 285, 60–66.
- Leon, G. R., Fulkerson, J. A., Perry, C. L., & Early-Zald, M. B. (1995). Prospective analysis of personality and behavioral vulnerabilities and gender influences in later development of disordered eating. Journal of Abnormal Psychology, 104, 140– 149.
- Lewinsohn, P. M., Gotlib, I. H., Lewinsohn, M., Seeley, J. R., & Allen, N. B. (1998). Gender differences in anxiety disorders and anxiety symptoms in adolescents. Journal of Abnormal Psychology, 107, 109–117.
- Lewinsohn, P. M., Rohde, P., Seeley, J. R., & Hops, H. (1991). The comorbidity of unipolar depression: Part 1. Major depression with dysthymia. Journal of Abnormal Psychology, 100, 205– 213.
- Lilienfeld, S. O., Waldman, I. D., & Israel, A. C. (1994). A critical examination of the use of the term and concept of comorbidity in psychopathology research. Clinical Psychology: Science and Practice, 1, 71–83.
- Loeber, R. (1991). Questions and advances in the study of developmental pathways. In D. Cicchetti & S. L. Toth (Eds.), Rochester symposium on developmental psychopathology: Vol. 3. Models and integrations (pp. 97–116). Rochester, NY: University of Rochester Press.
- Loeber, R., & Farrington, D. P. (2000). Young children who commit crime: Epidemiology, developmental origins, risk factors, early interventions, and policy implications. Development and Psychopathology, 12, 737–762.
- Lonigan, C. J., Hooe, E. S., David, C. F., & Kistner, J. A. (1999). Positive and negative affectivity in children: Confirmatory factor analysis of a two-factor model and its relation to symptoms of anxiety and depression. Journal of Consulting and Clinical Psychology, 67, 374–386.
- Lopez, S. R., & Guarnaccia, P. J. (2000). Cultural psychopathology: Uncovering the social world of mental illness. Annual Review of Psychology, 51, 571–598.
- Luthar, S. S., Cicchetti, D., & Becker, B. (2000). The construct of resilience: A critical evaluation and guidelines for future work. Child Development, 71, 543–562.
- Maedgen, J. W., & Carlson, C. L. (2000). Social functioning and emotional regulation in the attention deficit hyperactivity disorder subtypes. Journal of Clinical Child Psychology, 29, 30–42.
- Majcher, D., & Pollack, M. H. (1996). Childhood anxiety disorders. In L. Hechtman (Ed.), Do they grow out of it? Long-term outcomes of childhood disorders (pp. 139–170). Washington, DC: American Psychiatric Press.
- Manassis, K., & Bradley, S. (1994). The development of childhood anxiety disorders: Toward an integrated model. Journal of Applied Developmental Psychology, 15, 345–366.
- Manassis, K., Bradley, S., Goldberg, S., Hood, J., & Swinson, R. P. (1994). Attachment in mothers with anxiety disorders and their children. Journal of the American and Adolescent Psychiatry, 33, 1106–1113.
- Mancini, C., van Ameringen, M., Szatmari, P., Fugere, C., & Boyle, (1996). A high-risk pilot study of the children of adults with social phobia. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 1511–1517.
- Mannuzza, S., & Klein, R. (1992). Predictors of outcome of children with attention-deficit hyperactivity disorder. In G. Weiss (Ed.), Child and adolescent psychiatric clinics of North America: Attention-deficithyperactivitydisorder(pp.567–578).Philadelphia: Saunders.
- March, J. S. (Ed.). (1995). Anxiety disorders in children and adolescents. New York: Guilford Press.
- Mariani, M. A., & Barkley, R. A. (1997). Neuropsychological and academic functioning in preschool boys with attention deficit hyperactivity disorder. Developmental Neuropsychology, 13, 111– 129.
- Mash, E. J., & Barkley, R. A. (Eds.). (1996). Child psychopathology. New York: Guilford.
- Mash, E. J., & Barkley, R. A. (Eds.). (1998). Treatment of childhood disorders. New York: Guilford.
- Mash, E. J., & Dozois, D. J. A. (1996). Child psychopathology: A developmental systems perspective. In E. J. Mash & R. A. Barkley (Eds.), Child psychopathology (pp. 3–60). New York: Guilford.
- Mash, E. J., & Johnston, C. (1990). Determinants of parenting stress: Illustrations from families of hyperactive children and families of physically abused children. Journal of Clinical Child Psychology, 19, 313–328.
- Mash, E. J., & Johnston, C. (1996). Family relational problems: Their place in the study of psychopathology. Journal of Emotional and Behavioral Disorders, 4, 240–254.
- Mash, E. J., & Terdal, L. G. (1997a). Assessment of child and family disturbance: A behavioral-systems approach. In E. J. Mash & L. G. Terdal (Eds.), Assessment of childhood disorders (3rd ed., pp. 3–68). New York: Guilford Press.
- Mash, E. J., & Terdal, L. G. (Eds.). (1997b). Assessment of childhood disorders. New York: Guilford.
- Mash, E. J., & Wolfe, D. A. (2002). Abnormal child psychology (2nd ed.). Belmont, CA: Wadsworth.
- Masten, A. (2001). Ordinary magic: Resilience processes in development. American Psychologist, 56, 227–238.
- McCall, R. B., & Groark, C. J. (2000). The future of applied child development research and public policy. Child Development, 71, 197–204.
- McClure, E. B., Brennan, P. A., Hammen, C., & Le Brocque, R. M. (2001). Parental anxiety disorders, child anxiety disorders, and the perceived parent-child relationship in an Australian high-risk sample. Journal of Abnormal Child Psychology, 29, 1–10.
- McDermott, P. A., & Weiss, R. V. (1995). A normative typology of healthy, subclinical, and clinical behavior styles among American children and adolescents. Psychological Assessment, 7, 162–170.
- McGee, R., & Feehan, M. (1991). Are girls with problems of inattention underrecognized? Journal of Psychopathology and Behavioral Assessment, 13, 187–198.
- McLeod, J. D., & Nonnemaker, J. M. (2000). Poverty and child emotional and behavioral problems: Racial/ethnic differences in processes and effects. Journal of Health and Social Behavior, 41, 137–161.
- McMahon, R. J., & Estes, A. M. (1997). Conduct problems. In E. J. Mash & L. G. Terdal (Eds.), Assessment of childhood disorders (3rd ed., pp. 130–193). New York: Guilford Press.
- Melnick, S. M., & Hinshaw, S. P. (2000). Emotion regulation and parenting in AD/HD and comparison boys: Linkages with social behaviors and peer preference. Journal of Abnormal Child Psychology, 28, 73–86.
- Mesman, J., & Koot, H. M. (2000). Child-reported depression and anxiety in preadolescence: I. Associations with parent- and teacher-reported problems. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 1371–1378.
- Mick, E., Santangelo, S. L., Wypij, D., & Biederman, J. (2000). Impact of maternal depression on ratings of comorbid depression in adolescents with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 314–319.
- Milberger, S., Biederman, J., Faraone, S. V., Chen, L., & Jones, J. (1996). Is maternal smoking during pregnancy a risk factor for attention deficit hyperactivity disorder in children? American Journal of Psychiatry, 153, 1138–1142.
- Milberger, S., Biederman, J., Faraone, S. V., Guite, J., & Tsuang, M. T. (1997). Pregnancy, delivery and infancy complications and attention deficit hyperactivity disorder: Issues of gene environment interaction. Biological Psychiatry, 41, 65–75.
- Mischel, W. (1968). Personality and assessment. New York: Wiley.
- Muris, P., & Merckelbach, H. (2000). How serious are common childhood fears? II. The parent’s point of view. Behaviour Research and Therapy, 38, 813–818.
- Muris, P., Merckelbach, H., & Damsma, E. (2000). Threat perception in nonreferred socially anxious children. Journal of Clinical Child Psychology, 29, 348–359.
- Nada-Raja, S., Langley, J. D., McGee, R., Williams, S. M., Begg, D.J.,&Reeder,A.I.(1997).Inattentiveandhyperactivebehaviors and driving offences in adolescence. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 515–522.
- Neal, A. M., & Turner, S. M. (1991). Anxiety disorders research with African Americans: Current status. Psychological Bulletin, 109, 400–410.
- Offord, D. R., Boyle, M. H., Szatmari, P., Rae-Grant, N. I., Links, P. S., Cadman, D. T., Byles, J. A., Crawford, J. W., Blum, H. M., Byrne, C., Thomas, H., & Woodward, C. A. (1987). Ontario Child Health Study: II. Six-month prevalence of disorder and rates of service utilization. Archives of General Psychiatry, 44, 832–836.
- Ollendick, T. H., & King, N. J. (1994). Diagnosis, assessment, and treatment of internalizing problems in children: The role of longitudinal data. Journal of Consulting and Clinical Psychology, 62, 918–927.
- Ollendick, T. H., Mattis, S. G., & King, N. J. (1994). Panic in children and adolescents: Areview. Journal of Child Psychology and Psychiatry, 35, 113–134.
- Ollendick, T. H., Yang, B., King, N. J., Dong, Q., & Akande, A. (1996). Fears in American, Australian, Chinese, and Nigerian children and adolescents: A cross-cultural study. Journal of Child Psychology and Psychiatry, 37, 213–220.
- Olweus, D. (1979). Stability of aggressive reaction patterns in males: A review. Psychological Bulletin, 86, 852–875.
- Pauls, D. L. (1991). Genetic factors in the expression of attentiondeficit hyperactivity disorder. Journal of Child and Adolescent Psychopharmacology, 1, 353–360.
- Pennington,B.F.,&Ozonoff,S.(1991).Aneuroscientificperspective on continuity and discontinuity in developmental psychopathology. In D. Cicchetti & S. L. Toth (Eds.), Rochester symposium on developmental psychopathology: Vol. 3. Models and integrations (pp. 117–159). NewYork: University of Rochester Press.
- Pennington, B. F., & Ozonoff, S. (1996). Executive functions and developmental psychopathology. Journal of Child Psychology and Psychiatry, 37, 51–87.
- Perrin, S., Smith, P., & Yule, W. (2000). Practitioner review: The assessment and treatment of post-traumatic stress disorder in children and adolescents. Journal of Child Psychology and Psychiatry, 41, 277–289.
- Peterson, B. S., Pine, D. S., Cohen, P., & Brook, J. S. (2001). Prospective, longitudinal study of tic, obsessive-compulsive, and attention-deficit/hyperactivity disorders in an epidemiological sample. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 685–695.
- Phares, V., & Compas, B. (1992). The role of fathers in child and adolescent psychopathology: Make room for daddy. Psychological Bulletin, 111, 387–412.
- Piacentini, J., & Graae, F. (1997). Childhood OCD. In E. Hollander & D. Stein (Eds.), Obsessive-compulsive disorders: Diagnosis, etiology, treatment (pp. 23–46). New York: Marcel Dekker.
- Pine, D. S. (1997). Childhood anxiety disorders. Current Opinions in Pediatrics, 9, 329–338.
- Pine, D. S., Cohen, E., Cohen, P., & Brook, J. S. (2000). Social phobia and the persistence of conduct problems. Journal of Child Psychology and Psychiatry, 41, 657–665.
- Pine, D. S., & Grun, J. (1999). Childhood anxiety: Integrating developmental psychopathology and affective neuroscience. Journal of Child and Adolescent Psychopharmacology, 9, 1–12.
- Pliszka, S. R. (1992). Comorbidity of attention-deficit hyperactivity disorder and overanxious disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 197–203.
- Plomin, R. (1995). Genetics and children’s experiences in the family. Journal of Child Psychology and Psychiatry, 36, 33–38.
- Plomin, R., & Rutter, M. (1998). Child development, molecular genetics, and what to do with genes once they are found. Child Development, 69, 1223–1242.
- Prior, M., Smart, D., Sanson, A., & Oberklaid, F. (2000). Does shyinhibited temperament in childhood lead to anxiety problems in adolescence. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 461–468.
- Pynoos, R. S., Frederick, C., Nader, K., Arroyo, W., Steinberg, A., Eth, S., Nunez, F., & Fairbanks, L. (1987). Life threat and posttraumatic stress in school-age children. Archives of General Psychiatry, 44, 1057–1063.
- Quay, H. C. (1997). Inhibition and attention deficit hyperactivity disorder. Journal of Abnormal Child Psychology, 25, 7–13.
- Quist, J. F., & Kennedy, J. L. (2001). Genetics of childhood disorders: XXIII. ADHD, part 7: The serotonin system. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 253–256.
- Rapee, R. M. (1997). Potential role of childrearing practices in the development of anxiety and depression. Clinical Psychology Review, 17, 47–67.
- Rapport, M., & Chung, K. (2000). Attention deficit hyperactivity disorder. In M. Hersen & R. T. Ammerman (Eds.), Advanced abnormal child psychology (2nd ed., pp. 413–440). Mahwah, NJ: Erlbaum.
- Richters, J. E., & Cicchetti, D. (1993). Mark Twain meets DSM-III-R: Conduct disorder, development, and the concept of harmful dysfunction. Development and Psychopathology, 5, 5–29.
- Rie, H. E. (1971). Historical perspective of concepts of child psychopathology. In H. E. Rie (Ed.), Perspectives in child psychopathology (pp. 3–50). Chicago: Aldine-Atherton.
- Roberts, R. E., Attkisson, C. C., & Rosenblatt, A. (1998). Prevalence of psychopathology among children and adolescents. American Journal of Psychiatry, 155, 715–725.
- Rosenbaum, J. F., Biederman, J., Hirshfeld, D. R., Bolduc, E. A., Faraone, S. V., Kagan, J., Snidman, N., & Reznick, J. S. (1991). Further evidence of an association between behavioral inhibition and anxiety disorders: Results from a family study of children from a non-clinical sample. Journal of Psychiatric Research, 25, 49–65.
- Routh, D. K. (1990). Taxonomy in developmental psychopathology: Consider the source. In M. Lewis & S. M. Miller (Eds.), Handbook of developmental psychopathology (pp. 53–62). New York: Plenum.
- Rucklidge, J. J., & Tannock, R. (2001). Psychiatric, psychosocial, and cognitive functioning of female adolescents with ADHD. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 530–540.
- Rutter, M. (2000a). Genetic studies of autism: From the 1970s into the millennium. Journal of Abnormal Child Psychology, 28, 3–14.
- Rutter, M. (2000b). Psychosocial influences: Critiques, findings, and research needs. Development and Psychopathology, 12, 375– 405.
- Rutter,M.,&Sroufe,L.A.(2000).Developmentalpsychopathology: Concepts and challenges. Developmental and Psychopathology, 12, 265–296.
- Sallee, R., & Greenawald, J. (1995). Neurobiology. In J. S. March (Ed.), Anxiety disorders in children and adolescents (pp. 3–34). New York: Guilford Press.
- Sameroff, A. J., Lewis, M., & Miller, S. M. (Eds.). (2000). Handbook of developmental psychopathology (2nd ed.). New York: Kluwer Academic.
- Schachar, R., & Tannock, R. (1995). Test of four hypotheses for the comorbidity of attention-deficit hyperactivity disorder and conduct disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 34, 639–648.
- Schopler, E., Mesibov, G. B., & Kunce, L. J. (Eds.). (1998). Asperger syndrome or high-functioning autism? New York: Plenum.
- Schwartz, C. E., Snidman, N., & Kagan, J. (1999). Adolescent social anxiety as an outcome of inhibited temperament in childhood. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 1008–1015.
- Seidman, L. J., Biederman, J., Faraone, S. V., & Weber, W. (1997). A pilot study of neuropsychological function in girls with ADHD. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 366–373.
- Seligman, L. D., & Ollendick, T. H. (1998). Comorbidity of anxiety and depression in children and adolescents: An integrative review. Clinical Child and Family Psychology Review, 1,
- Semrud-Clikeman, M., Biederman, J., Sprich-Buckminster, S., Lehman, B. K., Faraone, S. V., & Norman, D. (1992). Comorbidity between ADHD and learning disability: A review and report in a clinically referred sample. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 439–448.
- Semrud-Clikeman, M., Steingard, R. J., Filipek, P., Biederman, J., Bekken, K., & Renshaw, P. F. (2000). Using MRI to examine brain-behavior relationships in males with attention deficit disorder with hyperactivity. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 477–484.
- Shadish, W. R., Matt, G. E., Navarro, A. M., & Phillips, G. (2000). The effects of psychological therapies under clinically representative conditions: A meta-analysis. Psychological Bulletin, 126, 512–529.
- Shadish, W. R., Matt, G. E., Navarro, A. M., Siegle, G., CritsChristoph, P., Hazelrigg, M. D., Jorm, A. F., Lyons, L. C., Nietzel, M. T., Prout, H. T., Robinson, L., Smith, M. L., Svartberg, M., & Weiss, B. (1997). Evidence that therapy works in clinically representative conditions. Journal of Consulting and Clinical Psychology, 65, 355–365.
- Shaffer, D., Fisher, P., Dulcan, M. K., Davies, M., Piacentini, J., Schwab-Stone, M. E., Lahey, B. B., Bourdon, K., Jensen, P. S., Bird, H. R., Canino, G., & Regier, D. A. (1996). The NIMH Diagnostic Inverview Schedule for Children Version 2.3 (DISC2.3): Description, acceptability, prevalence rates, and performance in the MECA study. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 865–877.
- Silk, J. S., Nath, S. R., Siegel, L. R., & Kendall, P. C. (2000). Conceptualizing mental disorders in children: Where have we been and where are we going? Development and Psychopathology, 12, 713–735.
- Silverman, I. W., & Ragusa, D. M. (1992). Child and maternal correlates of impulse control in 24-month-old children. Genetic, Social, and General Psychology Monographs, 116, 435–473.
- Silverthorn, P., Frick, P. J., Kuper, K., & Ott, J. (1996). Attention deficit hyperactivity disorder and sex: A test of two etiological models to explain the male predominance. Journal of Clinical Child Psychology, 25, 52–59.
- Siqueland, L., Kendall, P. C., & Steinberg, L. (1996). Perceived family environment and observed family interaction styles. Journal of Clinical Child Psychology, 25, 225–237.
- Sonuga-Barke, E. J. S., Daley, D., Thompson, M., Laver-Bradbury, C., & Weeks, A. (2001). Parent-based therapies for preschool attention-deficit/hyperactivity disorder: A randomized, controlled trial with a community sample. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 402–408.
- Southam-Gerow, M. A., & Kendall, P. C. (2000). A preliminary study of the emotion understanding of youths referred for treatment of anxiety disorders. Journal of Clinical Child Psychology, 29, 319–327.
- Spitzer, R. L., Davies, M., & Barkley, R. A. (1990). The DSM-III-R fieldtrialofdisruptivebehaviordisorders.JournaloftheAmerican Academy of Child andAdolescent Psychiatry, 29, 690–697.
- State, M. W., Lombroso, P. J., Pauls, D. L., & Leckman, J. F. (2000). The genetics of childhood psychiatric disorders: A decade of progress. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 946–962.
- Stein, M. A., Szumoski, E., Blondis, T. A., & Roizen, N. J. (1995). Adaptive skills dysfunction in ADD and ADHD children. Journal of Child Psychology and Psychiatry, 36, 663–670.
- Stevenson, J. (1992). Evidence for a genetic etiology in hyperactivity in children. Behavior Genetics, 22, 337–343.
- Stodgell, C. J., Ingram, J. L., & Hyman, S. L. (2000). The role of candidate genes in unraveling the genetics of autism. International Review of Research in Mental Retardation, 23, 57–82.
- Strauss, C. C., Lahey, B. B., Frick, P., Frame, C. L, & Hynd, G. W. (1988). Peer social status of children with anxiety disorders. Journal of Consulting and Clinical Psychology, 56, 137–141.
- Strauss, C. C., & Last, C. G. (1993). Social and simple phobias in children. Journal of Anxiety Disorders, 7, 141–152.
- Strauss, C. C., Last, C. G., Hersen, M., & Kazdin, A. E. (1988). Association between anxiety and depression in children and adolescents with anxiety disorders. Journal of Abnormal Child Psychology, 16, 57–68.
- Strauss, C. C., Lease, C. A., Kazdin, A. E., Dulcan, M. J., & Last, C. G. (1989). Multimethod assessment of the social competence of children with anxiety disorders. Journal of Clinical Child Psychology, 18, 184–189.
- Strauss, C. C., Lease, C. A., Last, C. G., & Francis, G. (1988). Overanxious disorder: An examination of developmental differences. Journal of Abnormal Child Psychology, 16, 433–443.
- Streissguth, A. P., Bookstein, F. L., Sampson, P. D., & Barr, H. M. (1995). Attention: Prenatal alcohol and continuities of vigilance and attentional problems from 4 through 14 years. Development and Psychopathology, 7, 419–446.
- Swedo, S. E., Rapoport, J. L., Leonard, H., Lenane, M., & Cheslow, D. (1989). Obsessive-compulsive disorder in children and adolescents: Clinical phenomenology of 70 consecutive cases. Archives of General Psychiatry, 46, 335–341.
- Szatmari, P. (1992). The epidemiology of attention-deficit hyperactivity disorders. In G. Weiss (Ed.), Child and adolescent psychiatric clinics of North America: Attention-deficit hyperactivity disorder (pp. 361–372). Philadelphia: Saunders.
- Tanguay, P. E. (2000). Pervasive developmental disorders: A 10year review. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 1079–1095.
- Tannock, R. (1998). Attention deficit hyperactivity disorder: Advances in cognitive, neurobiological, and genetic research. Journal of Child Psychology and Psychiatry, 39, 65–99.
- Tannock, R. (2000). Attention-deficit/hyperactivity disorder with anxietydisorders.InT.E.Brown(Ed.),Attentiondeficitdisorders and comorbidities in children, adolescents and adults (pp. 125– 170). Washington, DC:American Psychiatric Press.
- Taylor, E. (1995). Dysfunctions of attention. In D. Cicchetti & D. J. Cohen(Eds.),Developmentalpsychopathology:Riskdisorder,and adaptation (Vol. 2, pp. 243–273). New York: Wiley-Interscience.
- Taylor, E. (1999). Developmental neuropsychology of attention deficit and impulsiveness. Development and Psychopathology, 11, 607–628.
- Tolan, P. H., & Thomas, P. (1995). The implications of age of onset for delinquency risk: II. Longitudinal evidence. Journal of Abnormal Child Psychology, 23, 157–181.
- Treadwell,K.H.,Flannery-Schroeder,E.C.,&Kendall,P.C.(1994). Ethnicity and gender in a sample of clinic-referred anxious children: Adaptive functioning, diagnostic status, and treatment outcome. Journal of Anxiety Disorders, 9, 373–384.
- Treadwell, K. H., & Kendall, P. C. (1996). Self-talk in youth with anxiety disorders: States of mind, content specificity, and treatment outcome. Journal of Consulting and Clinical Psychology, 64, 941–950.
- Tremblay, R. E., Masse, B., Perron, D., LeBlanc, M., Schwartzman, A., & Ledingham, J. E. (1992). Early disruptive behavior, poor school achievement, delinquent behavior, and delinquent personality: Longitudinal analyses. Journal of Consulting and Clinical Psychology, 60, 64–72.
- Turner, S. M., Beidel, D. C., & Wolff, P. L. (1996). Is behavioral inhibition related to the anxiety disorders? Clinical Psychology Review, 16, 157–172.
- S. Department of Health and Human Services. (2000, November). Healthy people 2010: Understanding and improving health (2nd ed.). Washington, DC: U.S. Government Printing Office.
- S. Public Health Service. (2001a). Report of the surgeon general’s conference on children’s mental health: A national action agenda. Washington, DC: Department of Health and Human Services.
- S. Public Health Service. (2001b). Youth violence: Report from the surgeon general. Washington, DC: Department of Health and Human Services.
- van den Oord, E. J. C. G., Boomsma, D. I., & Verhulst, F. C. (1994). A study of problem behaviors in 10- to 15-year-old biologically related and unrelated international adoptees. Behavior Genetics, 24, 193–205.
- Vasey, M. W., El-Hag, N., & Daleiden, E. L. (1996). Anxiety and the processing of emotionally threatening stimuli: Distinctive patterns of selective attention among high- and low-test anxious children. Child Development, 67, 1173–1185.
- Vasey, M. W., & Ollendick, T. H. (2000). Anxiety. In A. J. Sameroff &M.L.Lewis(Eds.),Handbookofdevelopmentalpsychopathology (2nd ed., pp. 511–529). NewYork: KluwerAcademic.
- Velez, C. N., Johnson, J., & Cohen, P. (1989). A longitudinal analysis of selected risk factors for childhood psychopathology. Journal of the American Academy of Child and Adolescent Psychiatry, 28, 861–864.
- Volkmar, F. R., & Klin, A. (1998). Asperger syndrome and nonverbal learning disabilities. In E. Schopler, G. B. Mesibov, & L. J. Kunce (Eds.), Asperger syndrome or high-functioning autism? (pp. 107–121). New York: Plenum.
- Volkmar, F. R., & Klin, A. (2000). Asperger’s Disorder and higher functioning autism: Same or different? International Review of Research in Mental Retardation, 23, 83–111.
- Weiss, B., Catron, T., Harris, V., & Phung, T. M. (1999). The effectiveness of traditional child psychotherapy. Journal of Consulting and Clinical Psychology, 67, 82–94.
- Weiss, G., & Hechtman, L. T. (1993). Hyperactive children grown up: ADHD in children, adolescents, and adults (2nd ed.). New York: Guilford Press.
- Weissman, M. M., McAvay, G., Goldstein, R. B., Nunes, E. V., Verdeli, H., & Wickramaratne, P. J. (1999). Risk/protective factors among addicted mothers’ offspring: A replication study. American Journal of Drug and Alcohol Abuse, 25, 661–679.
- Weisz, J. R. (1998). Empirically supported treatments for children and adolescents: Efficacy, problems, and prospects. In K. S. Dobson & K. D. Craig (Eds.), Empirically supported therapies: Best practice in professional psychology (pp. 66–92). Newbury Park, CA: Sage.
- Weisz, J. R. (2000a). Lab-clinic differences and what we can do about them: I. The clinic-based treatment development model. Clinical Child Psychology Newsletter, 15(1), 1–3, 10–11.
- Weisz, J. R. (2000b). Lab-clinic differences and what we can do about them: II. Linking research and practice to enhance our public interest. Clinical Child Psychology Newsletter, 15(3), 1–4, 9.
- Weisz, J. R. (2000c). Lab-clinic differences and what we can do about them: III. National policy matters. Clinical Child Psychology Newsletter, 15(3), 1–3, 6, 10.
- Weisz, J. R., Donenberg, G. R., Han, S. S., & Weiss, B. (1995). Bridging the gap between laboratory and clinic in child and adolescent psychotherapy. Journal of Consulting and Clinical Psychology, 63, 688–701.
- Weisz, J. R., & Weiss, B. (1993). Effects of psychotherapy with children and adolescents. Newbury Park, CA: Sage.
- Werner, E. E. (1995). Resilience in development. Current Directions in Psychological Science, 4, 81–85.
- Werry, J. S. (2001). Pharmacological treatments of autism, attention deficit hyperactivity disorder, oppositional defiant disorder, and depression in children and youth—commentary. Journal of Clinical Child Psychology, 30, 110–113.
- Whalen, C. K., & Henker, B. (1999). The child with attentiondeficit/hyperactivity disorder in family contexts. In H. C. Quay & A. E. Hogan (Eds.), Handbook of disruptive behavior disorders (pp. 139–155). New York: Kluwer Academic.
- Wilens, T. E., Biederman, J., Mick, E., Faraone, S. V., & Spencer, T. (1997). Attention deficit hyperactivity disorder (ADHD) is associated with early onset substance use disorders. Journal of Nervous and Mental Disease, 185, 475–482.
- Wilens, T. E., Biederman, J., & Spencer, T. (1994). Clonidine for sleep disturbances associated with attention-deficit hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 33, 424–426.
- Willcutt, E. G., Pennington, B. F., Chhabildas, N. A., Friedman, M. C., & Alexander, J. (1999). Psychiatric comorbidity associated with DSM-IV ADHD in a nonreferred sample of twins. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 1355–1362.
- Willis, T. J., & Lovaas, I. (1977). A behavioral approach to treating hyperactive children: The parent’s role. In J. B. Milichap (Ed.), Learning disabilities and related disorders (pp. 119–140). Chicago: Yearbook Medical.
- Winsberg, B. G., & Comings, D. E. (1999). Association of the dopamine transporter gene (DAT1) with poor methylphenidate response. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 1474–1477.
- Wolfe, D. A. (1999). Child abuse: Implications for child development and psychopathology. Thousand Oaks, CA: Sage.
- Zahn-Waxler, C. (1993). Warriors and worriers: Gender and psychopathology. Development and Psychopathology, 5, 79–89.
- Zahn-Waxler, C., Cole, P. M., Welsh, J. D., & Fox, N. A. (1995). Psychophysiological correlates of empathy and prosocial behaviors in preschool children with behavior problems. Development and Psychopathology, 7, 27–48.
- Zahn-Waxler, C., Klimes-Dougan, B., & Slattery, M. J. (2000). Internalizing problems of childhood and adolescence. Development and Psychopathology, 12, 443–466.
- Zametkin, A. J., Liebenauer, L. L., Fitzgerald, G. A., King, A. C., Minkunas, D. V., Herscovitz, P., Yamada, E. M., & Cohen, R. M. (1993). Brain metabolism in teenagers with attention-deficit hyperactivity disorder. Archives of General Psychiatry, 50, 333–340.




