View sample Social Support And Health Research Paper. Browse other social sciences research paper examples and check the list of research paper topics for more inspiration. If you need a religion research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our research paper writing service for professional assistance. We offer high-quality assignments for reasonable rates.
The concept of social support as an important factor in health and illness is not new. ‘Friendship is a basic human need along with food, shelter, and clothing. We naturally desire to love other human beings and to be loved by them. A totally loveless life—a life without friends of any sort—is a life deprived of much needed good.’ These thoughts were expressed by Aristotle, 350 years BC (Alcalay 1983). During and toward the end of the Middle Ages the concept was even addressed as a possible remedy for illness. In 1599 Paracelsus, a pharmacist and natural scientist, actually prescribed ‘love as the best possible cure for several diseases.’ That love and affection ‘influence life and death in both animals and humans’ was further observed by a Russian ethologist (Kropotkin 1908).
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
In this research paper some of the empirical evidence that ‘love and affection influence life and death’ will be reviewed. The distinctions between social networks and social support are explained; the definition, concepts, and functions of social support are further described; and their impact on health and disease are demonstrated and discussed. With a focus on coronary heart disease (CHD), the most common cause of death among men and women in the developed world, the hazards of lack of social support are disentangled, and differences and similarities in men and women are discussed. Finally, implications for therapeutic interventions are considered.
Systematic and conclusive empirical studies of social support and health, however, did not begin until the 1970s, when this field emerged as a new area of research, making a bold link between people’s social ties and social networks on the one hand and population morbidity and mortality on the other. In the pioneering work by Berkman and Syme on residents of Alameda County, California, modern epidemiological tools were applied to demonstrate what had long been sensed to be true: social ties are protective against ill health.
Soon a number of population-based studies mainly from the USA and Scandinavia confirmed the findings of Berkman and Syme. These findings were systematically interpreted and discussed by House et al. (1988) who concluded that the impact of lack of social ties was similar to that of smoking. With such emphasis and visibility of the concept, a new research field was established.
A general definition of social support was agreed upon, which was broad enough to incorporate most of the research traditions in the field: ‘Social support is the resource provided by other persons. By viewing social support in terms of resources—potentially useful information or things—we allow for the possibility that support may have negative as well as positive effects on health and well-being’ (Cohen and Syme 1985).
Soon, however, researchers began to ask why and how social ties might influence mortality and morbidity; in particular investigators were focusing on the function and contents of social ties and their assessment (Cohen and Syme 1985). On the one hand, large epidemiological studies of populations typically would find that mortality increased with a decreasing number and frequency of social contacts. On the other hand, the more sophisticated measures of social context, social anchorage, social environment, and social support were limited to specific indicators of disease such as blood pressure in smaller selected groups of persons or patients. Thus two types of research traditions developed within this area—social network epidemiology and social support psychology. Attempts to unite these traditions have not always been successful. Where the first type of research mostly examined all causes of mortality or general well-being as end-points, the latter has looked more closely at specific disease end-points, such as cardiovascular disease. The latter has become a model for research on social support and disease, and will be the focus here, because heart diseases are common, develop gradually, and are found in all populations.
Coronary heart disease (CHD) is the most common of cardiovascular diseases and the most common cause of death in highly developed and industrialized countries, and it is rapidly increasing in developing nations of the third world. In many countries it is also the most common cause of hospitalizations and an important factor in work absenteeism. The clinical manifestations of CHD are dependent on the extent of underlying atherosclerotic changes of the coronary arteries. With more advanced atherosclerosis, the risk of an acute myocardial infarction (AMI) or sudden cardiac death (SCD) is increased. The occurrence of both atherosclerosis and clinical manifestations of CHD increases with increasing age, in men as in women.
Below the age of 65, clinical manifestations of CHD, including myocardial infarction and sudden death are rare in women. In particular before menopause at age 50, women seem to be protected. Women are also relatively spared in the following decade, between 50 and 60 years of age. By the age of 60, sex differences are beginning to vanish. This may be one of the reasons why research on CHD has been so remarkably focused on men in their middle ages, under age 65. Most research on coronary risk factors and factors that are protective of CHD has been carried out on middle-aged men. Therefore knowledge about heart disease in women is less evidence-based than that of men. This is particularly true as concerns the psychosocial influences on heart disease and its risk factors.
1. The Social Environment And The Heart
Lifestyle and daily habits—the way we live in the broadest sense—strongly influence the atherosclerotic process. If we smoke, lead a sedentary life, eat too much fat and too little fiber, the risk of premature atherosclerosis and early heart disease is increased. It is also well known that many social environments may enhance or prevent the improvement of lifestyle and behavioral risk factors. Therefore, psychosocial influences, including the concepts of stress and social support should be recognized as relevant, both in cardiology and in general health care.
Support from social networks may help the individual to deal with stress in many ways. Network members may provide help to recognize and evaluate stressors in the environment, and they may also be helpful in identifying solutions to overcome the stressor (information/appraisal support). This means that they may provide tools to improve problemoriented coping, and thereby enhance stress reduction. Network members may also provide emotional support that may counteract the individual’s feeling of loneliness and hopelessness, and thus help him or her to deal more efficiently with problems. Supportive actions may also relieve stress by reducing tension and anxiety, and counteracting depressive reactions (emotional support). Furthermore, supportive actions may also be helpful as they provide practical help (tangible support). Therefore, the empirical evidence of social support effects may be found at various stages of the pathogenic processes leading to heart disease. An epidemiological as well as a behavioral and psychophysiological view of the relationship is scientifically sound.
2. Social Support And Cardiovascular Health In Men
Large epidemiologic studies of social support and social networks have mainly focused on mortality as an endpoint. Scarce networks and few contacts are generally found to increase mortality risk. The incidence of acute cardiac events such as myocardial infarction or sudden cardiac death, however, has rarely been investigated in relation to social support. Furthermore, the most commonly studied aspect of social support is marital status. In men, marriage or cohabiting seems to improve cardiovascular health and to decrease mortality (Case et al. 1992). In women, as we shall see below, the picture is more complex.
Several large-scale epidemiological studies have been conducted in Sweden and Scandinavia. Scandinavian countries have a relatively homogenous, easily assessed population, living under good material conditions, where poverty, in its concrete sense, is rare. This does not mean that loneliness and lack of social support are irrelevant. In contrast, where the basic physical needs are met and a decent standard of living provided by public or governmental services, social ties and relations with other people tend to become diminished. In addition, the cold and dark climate, characteristic of these countries, does not promote social interaction, but rather may prevent naturally occurring social encounters.
In one of the early population-based studies of risk factors for CHD, the study of 50-year-old men born in Gothenburg (men born in 1913, in 1923, and in 1933), the impact of poor social networks and lack of social support was first assessed. Scarce social ties and social isolation increased both total and cardiovascular mortality (Welin et al. 1985). In further studies of men born in 1914 in the city of Malmo in south Sweden this observation was confirmed. The provision of satisfactory social ties and adequate social and psychological anchorage was essential to good health and longevity in men (Hanson 1989).
In a subsequent assessment of the Gothenburg study group, a random sample of 776 men, who were found healthy on initial examination, were followed for incidence of AMI and death from CHD. Lack of social support, as measured by the Interview Schedule for Social Interaction (ISSI), an instrument which was modified for population based studies in our laboratory, was found to be an independent predictor of AMI and death from CHD, including sudden cardiac death. This instrument is also described in Rosengren et al. (1993). These effects were maintained even after controlling for the effects of standard cardiovascular risk factors (hypertension, hyperlipidemia, smoking, diabetes, lack of exercise, etc.). The effect of lack of support was comparable in magnitude to that of smoking (Rosengren et al. 1993).
All other risk factors, including elevated cholesterol, or fibrinogen levels, hypertension or obesity were less strong predictors. When smokers and non-smokers were analyzed separately, risk gradients between men with high and men with low support were similar in magnitude. Male smokers with little social support were at highest risk for CHD whereas male nonsmokers with large networks and good support were at lowest risk (7.1 percent vs. 0.8 percent) (Rosengren et al. 1993). These and other studies have demonstrated that lack of social support and its various functions are predictors of disease incidence, and exert an effect that is independent of physiological and lifestyle risk factors.
However, once signs and symptoms of chronic disease have occurred one would expect them to override the impact of ‘soft’ risk factors such as social support. Therefore the study of patients suffering from chronic disease, such as coronary disease, is crucial.
In an early landmark study of over two thousand male survivors of acute myocardial infarction, Ruberman et al. (1984) showed that, even in the presence of clinical coronary disease, social isolation and stress contributed significantly to the increase in mortality risk. These risk factors were more common in men with low education. This early finding of a social gradient in health and disease has subsequently been frequently discussed and confirmed in both populationand patient-based studies (Haan et al. 1987).
In general, findings in men support the notion that one way in which the health hazards of social disadvantage are expressed is through the lack of adequate social networks and support. In order to provide appraisal and tangible support in times of hardships, men with high education and high job positions usually have a vast network of friends and acquaintances from professional and other organizations or groups, which they can draw upon for help in difficult situations. In low job positions, networks are known to be smaller and less effective; also social activities and social interactions are known to be more centered on family and family members. Therefore, the specific functions of information and concrete practical help, which are unevenly distributed across social strata and found to be crucial for maintenance of good health (Hanson 1989) may explain why cardiovascular health and health in general is better in higher social classes.
3. Social Support And Emotions
Social supports are provided to the individual by his/her social environment in an ongoing interactive process. This interactive process depends not only on the availability of supportive structures, but also on individual personal characteristics, such as the coronary prone behavior and/or emotional reactive patterns, such as depressive and anxious feelings. Whether the individual is able to receive and to provide social supports makes a difference for health outcomes. This includes the frequently studied coronary prone and hostile behaviors, which particularly in men were predictive of new incidence of coronary attacks (Brummett et al. 1998).
If considered in the presence of supporting social structures some of these findings are intuitively easier to understand. In a Swedish study of 150 male cardiac patients who were followed for ten years, evidence of such interactive effects on disease risk was found, in addition to clinical cardiac prognostic factors. The psychosocial factors assessed in these patients included social integration and social support as well as the Type A behavior pattern, using the original Structured Interview procedure. In accordance with other studies at the time, Type A behavior was not found to worsen prognosis in cardiac patients (Ragland and Brand 1988): 24 percent of men with Type A as compared to 22 percent of men with Type B died from CHD during follow-up. In contrast, social isolation was a prominent risk factor for poor prognosis. Men who said they practically never engaged in social activities with others for leisure were defined as socially isolated. They had about three times the mortality risk of men who said they were socially active at least once a month (Orth-Gomer et al. 1988). The worst prognosis, however, was found in Type A men who were socially isolated, their ten-year mortality risk being 69 percent, whereas, in socially active men, the behavior type made no difference (21 percent in type B and 17 percent in Type A men) (Orth-Gomer et al. 1988).
These results suggest that investigating either social environmental or individual behavioral factors alone is insufficient. Instead an attempt to integrate social and physical environment with individual psycho- logical reactions appears to be more meaningful. Such models have been successfully applied and tested. An important example is the role of depressive reactions and their relation to outcome in patients with coronary disease.
In several patient-based studies it has been have shown that depressed symptoms and feelings increase mortality risk in patients post AMI (Barefoot et al. 1996, Frasure-Smith et al. 1995). These depressive reactions are tied into a social context that is much influenced by the individual and collective capacity for coping with stressors (Holahan et al. 1995). Such coping capacity will in its turn depend on the provision of social supports. Therefore the more recent studies of psychosocial factors in women have been conceptualized taking these integrative aspects into consideration.
4. Social Support In Relation To CHD In Women
Women have rarely been studied in regard to psychosocial factors and CHD. This is true for both social contextual factors, such as stress and social support, and the more individually based aspects of depression, coping, mastery, etc. It is interesting to note that many studies of coronary risk profiles did include women— but usually in too small numbers to be conclusive about their risk profile or about gender differences. Nevertheless findings are often generalized to both men and women.
This was one of several reasons for initiating the Stockholm Female Coronary Risk Study (FemCor-Risk Study). This is a community-based case-control study, comprising 300 women below age 65, who were admitted to the coronary care units with acute coronary syndromes in greater Stockholm during a three-year period. Women with CHD were compared to a random sample of 300 age-matched women from the normal population, obtained via the official census registry of the same area. Psychosocial and biological risk factors were examined using interview, survey, psychosocial, and physical examination techniques. The core study objectives were:
(a) To examine psychosocial risk factor effects on CHD in women;
(b) To examine psychosocial determinants of life- style and the psychobiological mechanisms involved;
(c) To describe protective factors and mechanisms which buffer against noxious psychosocial influences. Several different strategies for analyses of the results have been applied, including case-control comparison, cross-sectional analyses among healthy women, prospective follow-up of women with cardiac disease, etc.
Lack of social support and social isolation was found to be one of the major stressors identified in this study group. As the sick role and the biological disease process itself may influence both social activities and social support in most people, we relied on follow-up rather than cross-sectional comparisons. Case-control comparisons were used to adjust for risk factors such as education, occupation, etc. Separate analyses of underlying coronary artery disease were undertaken, with patients being examined with quantitative coronary angiography (QCA).
QCA was carried out in 131 of the original 292 patients, based on available space at the angiographic laboratory. Patients who did and did not undergo angiography were compared, but differences in coronary risk factor profile were not found. Measures of severity (presence and number of stenoses greater than 50 percent) and measures of extent (number of stenoses greater than 20 percent) of coronary artery disease were evaluated.
After adjustment for age alone, lack of social support was associated with both measures. After adjustment for lifestyle and physiological risk factors, the risk ratio for stenosis greater than 50 percent in women with poor as compared to strong social support was 2.5 (Orth-Gomer et al. 1998). Women with poor social support also had a greater number of less hazardous stenoses, obstructing the coronary lumen by only 20 percent. After multivariate control for all other risk factors, however, this association was of only borderline significance. These associations were not explained by severity of anginal symptoms, selfrated subjective health status, or other clinical indicators of poor prognosis.
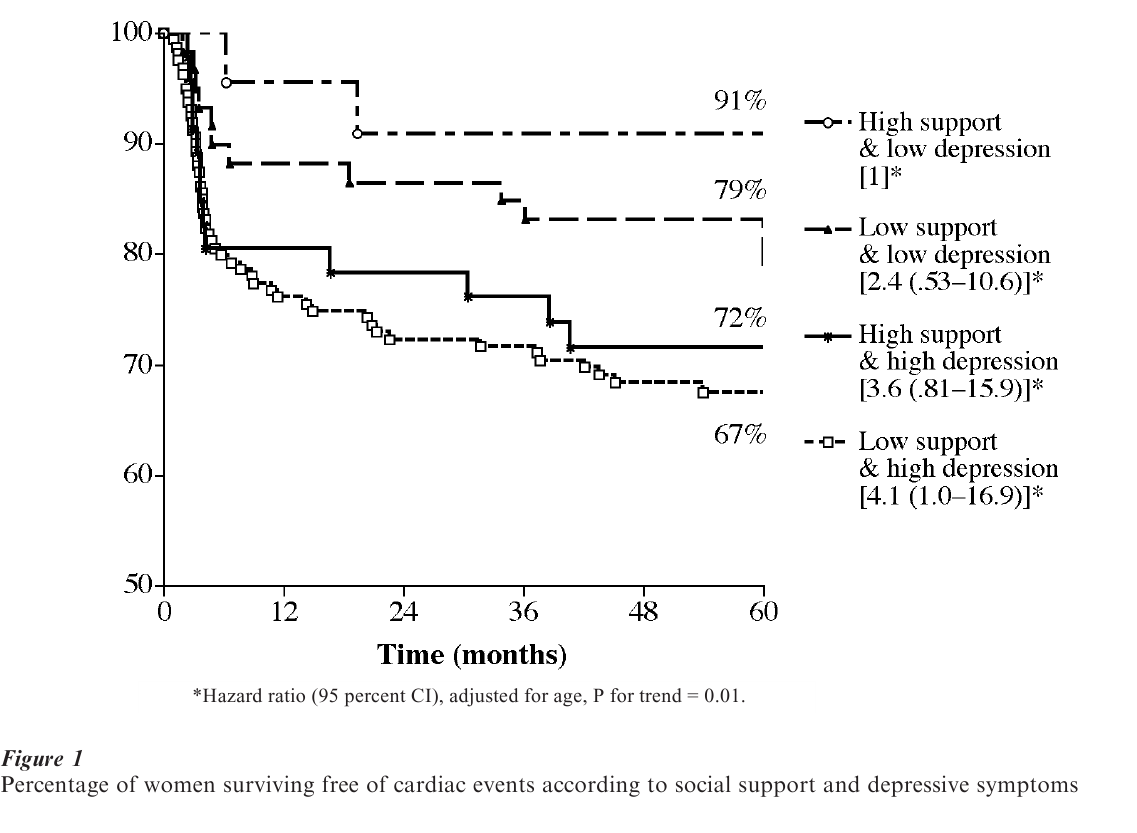
Subsequently, the impact of social isolation and depressed affect was examined in a five-year follow-up of recurrent events in all women patients (Horsten et al. 2000). They were followed for a median of five years after admission for the acute coronary event. By means of the centralized healthcare system in Sweden, complete follow-up information for recurrent events (hospitalizations and deaths) was obtained (Alfredsson et al. 1997). A total of 81 patients (27 percent) either died from cardiovascular causes or had a recurrent AMI or a revascularization procedure.
Women patients, who at initial examination showed signs of depressed affect (two or more symptoms of depression as measured by a short instrument by Pearlin et al. 1981) had twice the risk of recurrent events as compared to women who were not depressed. When social isolation was added to the model a further increase in risk was noted. As shown in Fig. 1, 33 percent of those who showed both depressed affect and social isolation had new events as compared to 9 percent of those who were free from both these problems, an almost fourfold difference. Prognostic risk factors including age, menopausal status, diagnosis at index event, symptoms of heart failure, diabetes, systolic blood pressure, smoking, body mass index, exercise, total cholesterol, triglycerides, HDL, therapy of beta-blockers, or ACE-inhibitors did not explain the effects of psychosocial determinants (Horsten et al. 2000).
5. Work Stress, Family Stress, And CHD In Women
Psychosocial stress at work has been consistently studied and shown to increase the risk of CHD (Karasek and Theorell 1990). Using the concept of high demand and low control presented by Karasek and Theorell an increased CHD risk ratio of about two has been found in men workers. Although women have not been as extensively studied, it is suggested that they have about the same CHD incidence rates associated with work stress as men do (Schnall et al. 1994).
When analyzing the contribution of high demand and low control in the case-control comparison of the FemCorRisk Study an odds ratio of about two was found. A further—and stronger—source of stress was family problems. Based on the concept presented by Frankenhaeuser et al. (1989), exposure to both stressors at work and those that originate from outside work was analyzed in a structured interview procedure. The predictive values of the two different work stress measures were almost identical. In the case- control comparison the odds ratio for work stress was 2.3 whereas that for family stress originating from a dyadic relationship was 2.9. In addition both work stress and family stress were associated with low SES. As expected, women with unskilled jobs had lower control over their jobs, but they also had increased family stress, in particular from separations.
Furthermore the effects of these stressors on eventfree survival in women with CHD were examined. The risk of a recurrent event in women patients with severe marital stress as compared to no or little stress was 2.8 after control for age, menopausal status, family history of CHD, symptoms of chest pain and heart failure, diabetes, smoking, and levels of triglycerides and HDL cholesterol. The actuarial five-year probability of being free from cardiac recurrent events in women without marital stress was 85 percent. In women with severe marital problems it was 65 percent (OrthGomer et al. 2000).
This effect was modified by individual capacity to cope with stressors, as assessed by a short instrument describing degree of mastery, obtained from Pearlin et al. (1981). This self-rated scale attempts to quantify the extent to which the individual perceives that he she can deal with and master problems and stressors in everyday life.
In women patients with poor mastery the experience of severe marital stress increased the risk of recurrent events by a factor of eight. In women with good mastery there was no significant effect of marital stress on risk of recurrences. Furthermore, the ability to master or cope with problems was related to socioeconomic status (women with low SES having poorer mastery scores), depressive symptoms, and social isolation (Wamala 2001).
These findings may be summarized as follows: women patients who experienced marital stress, when assessed after an acute coronary event, had a worsened prognosis if they also had a low education or an unskilled job, if they had depressive symptoms, if they were socially isolated, and poor at mastering difficulties and problems of everyday life. Numbers in subgroups were too small to analyze risk ratios in these different categories, but it is probable that all these factors are interrelated and overlap. This knowledge can be used to implement and improve preventive measures aimed at secondary prevention in women. Such interventions are ongoing, both in the US (ENRICHD) and in Sweden (Healthier Female Hearts in Stockholm).
6. Gender Differences In Cardiovascular Effects
To our knowledge, the harmful effects of family stress, depressed affect, poor mastery, and social isolation have not been investigated in a similar way in men. However, in an earlier study of Swedish men with CHD, the question was asked which life domain had generated the most severe stress experiences, work, family, education, or other. A majority of men (80 percent) ascribed their worst stress periods to the work situation, and only 10 percent to the family and spousal problems. This apparent gender difference is further supported by recent data from two large surveys of men and women of the general population in Massachusetts (Shumaker and Hill 1991).
When asked which person was the most important provider of social support, men were more than twice as likely to name their spouse, whereas women were most likely to name a friend or relative, usually female, as their primary supporter. In addition, women were more likely than men to report that they give more than they receive in dyadic relationships. In the FemCorRisk Study, 89 percent of the women said they were their spouse’s closest confidants, whereas only 75 percent of women named their spouse as their closest confidant. In contrast to previous studies in men, being married or cohabiting did not in itself provide any extra protection from cardiovascular ill health. Instead, for these women, the strain from a problematic spousal relationship significantly contributed to a poor prognosis over and above the effect of clinical cardiac predictors.
Therefore, the determinants, the protective health effects, and the mechanisms of social support may differ profoundly between men and women. Consequently they need to be separately conceptualized, examined, measured and analyzed, and implemented for use in clinical and community-based interventions and preventive efforts. In both men and women, however, the protective effects of social support and the health hazards of social isolation are strong and complex. Further research on processes and pathways as well as methods to implement this knowledge in preventive efforts is highly needed.
Bibliography:
- Alcalay R 1983 . In: Alcalay R (ed.) Ethics. Elsevier, Amsterdam, pp. 71–88
- Alfredsson L, Hammar N, Hodell A, Spetz C-L, Akesson L-O, Kahan T, Ysberg A-S 1997 Vardering av diagnoskvaliteten for akut hjartinfarkt vivtre svenska lan 1995 [Validation of the quality of diagnosis for acute myocardial infarction in three Swedish districts]. Socialstyrelsen 84–8
- Barefoot J C, Helms M J, Mark D B, Blumenthal J A, Califf R M, Haney T L, O’Connor C M, Siegler I G, Williams R B 1996 Depression and long-term mortality risk in patients with coronary artery disease. American Journal of Cardiology 78: 613–17
- Brummett B H, Babyak M A, Barefoot J C, Bosworth H B, Clapp-Channing N E, Siegler I C, Williams R B, Mark D B 1998 Social support and hostility as predictors of depressive symptoms in cardiac patients one month following hospitalization: A prospective study. Psychosomatic Medicine 60: 707–13
- Case B R, Moss A J, Case N 1992 Living alone after myocardial infarction. Journal of the American Medical Association 267: 520–4
- Cohen S, Syme S L 1985 Social Support and Health. Academic Press, New York
- Frankenhaeuser M, Lundberg U, Fredriksson M, Melin B, Tuomisto M, Myrsten A-L, Hedman M, Bergman-Losman B, Wallin L 1989 Stress on and off the job as related to sex and occupational status in white-collar workers. Journal of Organizational Behavior 10: 321–46
- Frasure-Smith N, Lesperance F, Talajic M 1995 Depression and 18-month prognosis after myocardial infarction. Circulation 91: 999–1005
- Haan M, Kaplan G A, Camacho T 1987 Poverty and health: Prospective evidence from the Alameda County Study. American Journal of Epidemiology 125: 989–98
- Hanson B S 1989 Social network and social support influence mortality in elderly men. The prospective population study of ‘Men born in 1914’ Malmo, Sweden. American Journal of Epidemiology 130(1): 100–11
- Holahan C J, Holahan C K, Moos R H, Brennan P L 1995 Social support, coping, and depressive symptoms in a latemiddle-aged sample of patients reporting cardiac illness. Health Psychology 14: 152–63
- Horsten M, Mittleman M, Wamala S P, Schenck-Gustafsson K, Orth-Gomer K 2000 Social isolation and depression in relation to prognosis of coronary heart disease in women. European Heart Journal 21: 1072–80
- House J S, Landis K R, Umberson D 1988 Social relationships and health. Science 241: 540–5
- Karasek R, Theorell T 1990 Healthy Work: Stress, Productivity, and the Reconstruction of Working Life. Basic Books, New York
- Kropotkin P 1908 Gegenseitige Hilfe in der Tierund Menschen-welt. Thomas, Leipzig, Germany
- Orth-Gomer K, Horsten, M, Wamala S P, Mittleman M A, Kirkeeide R, Svane B, Ryden L, Schenck-Gustafsson K 1998 Social relations and extent and severity of coronary artery disease. The Stockholm Female coronary risk study. European Heart Journal 19: 1648–56
- Orth-Gomer K, Unden A-L, Edwards M-E 1988 Social isolation and mortality in ischemic heart disease. A 10-year follow-up study of 150 middle-aged men. Acta Medica Scandinavica 224: 205–15
- Orth-Gomer K, Wamala S P, Horsten M, Schenck-Gustafsson K, Schneiderman N, Mittleman M A 2000 Marital stress worsens prognosis in women with coronary heart disease. The Stockholm female coronary risk study. Journal of the American Medical Association 284(23): 3008–14
- Paracelsus [Theophrastus Bombastus von Hohenheim] 1599 Labyrinthus medicorum errantium. Hanoviae
- Pearlin L L, Menagham E G, Lieberman M A, Mullan J T 1981 The stress process. Journal for Health Social Behavior 22: 337–56
- Ragland D R, Brand R J 1988 Type A behavior and mortality from coronary heart disease. New England Journal of Medicine 318: 65–9
- Rosengren A, Orth-Gomer K, Wedel H, Wilhelmsen L 1993 Stressful life events, social support, and mortality in men born in 1933. British Medical Journal 307: 1102–5
- Ruberman W, Weinblatt E, Goldberg J D 1984 Psychosocial influences on mortality after myocardial infarction. New England Journal of Medicine 311: 552–9
- Schnall P L, Landsbergis P A, Baker D 1994 Job strain and cardiovascular disease. Annual Review of Public Health 15: 381–411
- Shumaker S A, Hill D R 1991 Gender differences in social support and physical health. Health Psychology 10: 102–11
- Wamala, S P 2001 Stora sociala skillnader bakom dvinnors risk for kranskarlssjukdom. Okvalificerat jobb och slitningar i familjen avgorande faktorer [Large social inequalities in coronary heart disease risk among women. Low occupational status and family stress are crucial factors]. Lakartidningen [Journal of the Swedish Medical Association] 98(3): 177–81
- Welin L, Svardsudd K, Ander-Perciva S, Tibblin G, Tibblin B, Larsson B, Wilhelmsen L 1985 Prospective study of social influences on mortality. The study of men born in 1913 and 1923. The Lancet I : 915–8
- Williams R B, Barefoot J C, Califf R M, Haney T L, Saunders W B, Pryor D B, Hlatky M A, Siegler I C, Mark D B 1992 Prognostic importance of social and economic resources among medically treated patients with angiographically documented coronary artery disease. Journal of the American Medical Association 267: 520–4




