Sample Personality Disorders Research Paper. Browse other research paper examples and check the list of research paper topics for more inspiration. iResearchNet offers academic assignment help for students all over the world: writing from scratch, editing, proofreading, problem solving, from essays to dissertations, from humanities to STEM. We offer full confidentiality, safe payment, originality, and money-back guarantee. Secure your academic success with our risk-free services.
The American Psychiatric Association (APA) includes 10 personality disorders in their Diagnostic and Statistical Manual of Mental Disorders–Fourth Edition (DSM-IV; APA, 1994, 2000): paranoid, schizoid, schizotypal, antisocial, borderline, histrionic, narcissistic, avoidant, dependent, and obsessive-compulsive. We discuss each of these personality disorders individually later in this research paper. The 10 officially recognized personality disorders are further organized into three clusters based on descriptive similarities: Cluster A (odd-eccentric) includes paranoid, schizoid, and schizotypal; Cluster B (dramatic-erraticemotional) includes antisocial, borderline, histrionic, and narcissistic; and Cluster C (anxious-fearful) includes avoidant, dependent, and obsessive-compulsive. Two additional personality disorders (passive-aggressive and depressive) are provided within an appendix to DSM-IV for diagnoses that are not yet officially recognized. DSMIV also includes the diagnosis of personality disorder not otherwise specified (PDNOS), a diagnosis clinicians can provide when they believe that a personality disorder is present but the symptomatology of the patient is not adequately represented by one of the 10 officially recognized diagnoses.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
“Personality traits are enduring patterns of perceiving, relating to, and thinking about the environment and oneself that are exhibited in a wide range of social and personal contexts” (APA, 2000, p. 686). It is when “personality traits are inflexible and maladaptive and cause significant functional impairment or subjective distress [that] they constitute personality disorders” (APA, 2000, p. 686). DSM-IV (1994, 2000) provides a formal and general definition of personality disorder that is particularly important to consider when using the PDNOS diagnosis. Table 6.1 presents these general diagnostic criteria.
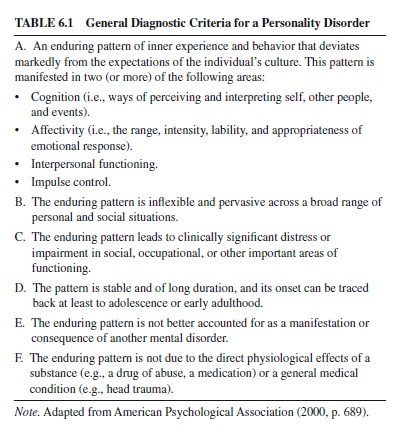
The general diagnostic criteria are concerned primarily with documenting that the symptomatology concerns personality functioning (i.e., an enduring pattern of inner experience that is pervasive across a broad range of personal and social functioning) rather than another domain of psychopathology (e.g., mood or anxiety disorder). However, we want to highlight here three of the general diagnostic criteria.
First, it is stated in DSM-IV that a personality disorder “leads to clinically significant distress or impairment in social, occupational, or other important areas of functioning” (APA, 2000, p. 689). A difficulty many clinicians have with personality disorder (and other mental disorder) diagnosis is the absence of any definition or guidelines for what is meant by a clinically significant impairment (Spitzer & Wakefield, 1999; Widiger & Corbitt, 1994). DSM-IV states only that it is “an inherently difficult clinical judgment” (APA, 2000, p. 8).
DSM-III through DSM-IV have provided specific rules for when enough features of a specific personality disorder, such as schizoid or borderline, are present in order for it to be diagnosed, but the rationale for these diagnostic thresholds are unexplained and do not appear to bear a relationship to the presence of a clinically significant level of impairment (Widiger & Corbitt, 1994). In the absence of any guidelines or rationale for the diagnostic thresholds, it is not surprising to find substantial variation in the diagnostic thresholds across each edition. For example, Morey (1988) reported an 800% increase in the number of persons beyond the threshold for a schizoid diagnosis in DSM-III-R as compared to DSM-III and a 350% increase for the narcissistic diagnosis. Some of this shift in prevalence might have been intentional (Widiger, Frances, Spitzer, & Williams, 1988), but much of it was unanticipated (Blashfield, Blum, & Pfohl, 1992). An important focus of future research and DSM-V will be the development of a clearer distinction between the presence and absence of a mental disorder (Spitzer & Wakefield, 1999; Widiger, 2001).
A second point of emphasis with respect to the general definition of personality disorder is that personality disorder symptomatology is stable over time and of long duration. The onset of a personality disorder must be traceable back to adolescence or early adulthood. Temporal stability is fundamental to the concept of personality and to the diagnosis of personality disorders (Tickle, Heatherton, & Wittenberg, 2001). However, the extent to which this fundamental component of personality is in fact assessed by researchers and clinicians is unclear. Clinicians and researchers tend to emphasize current symptomatology, and they may do so at the neglect of determining whether the symptomatology has in fact been present throughout much of a person’s life; this at times contributes to overdiagnosis and to a failure to adequately distinguish personality disorders and other mental disorders.
Finally, the symptoms of a personality disorder are said in the general definition to deviate from the expectations of one’s culture. The purpose of this DSM-IV cultural deviation requirement is to decrease the likelihood that clinicians will impose the expectations of their own culture onto a patient (Rogler, 1996). The DSM-IV cultural deviation requirement emphasizes that a behavior pattern that appears to be deviant from the perspective of one’s own culture might be quite normative and adaptive within another culture. Therefore, the expectations or norms within the clinician’s culture might not necessarily be relevant or applicable to a patient from a different cultural background. For example, “what is considered to be excessively inhibited in one culture may be courteously dignified within another” (Widiger, Mangine, Corbitt, Ellis, & Thomas, 1995, p. 212).
However, one should not infer from the cultural deviation requirement that a personality disorder is simply a deviation from a cultural norm. Optimal, healthy functioning does not necessarily involve adaptation to cultural expectations, nor does adaptation to cultural expectations necessarily ensure the absence of maladaptive personality traits (Wakefield, 1992). In fact, some of the personality disorders may represent—at least in part—excessive or exaggerated expressions of traits that a culture values or encourages, at least within some members of that culture (Alarcon, 1996; Rogler, 1996; Widiger & Spitzer, 1991). For example, it is usually adaptive to be confident but not to be arrogant, to be agreeable but not to be submissive, or to be conscientious but not to be perfectionistic.
Clinical Importance of Personality Disorders
The diagnosis of personality disorders can be quite difficult and even controversial. Nevertheless, the importance in assessing for the presence of personality disorders in clinical practice equals the difficulties of their diagnosis. A formal recognition by the American Psychiatric Association of the importance of personality classification to clinical diagnosis and treatment planning was demonstrated by the provision of a separate diagnostic axis (Axis II) devoted to personality disorders in DSM-III (APA, 1980; Frances, 1980). Personality disorders (along with mental retardation) continue to be placed on a separate axis for diagnosis in DSM-IV; all other mental disorders are diagnosed on Axis I (APA, 2000).
The valid, accurate assessment of personality disorders is important for several reasons. First, the existing large-scale studies that have assessed individuals for the full range of Axis I and Axis II disorders indicate that personality disorders are prevalent in both clinical and nonclinical populations (Mattia & Zimmerman, 2001). For example, Koenigsberg, Kaplan, Gilmore, and Cooper (1985) reported that 36% of over 2,000 psychiatric patients in their sample received a personality disorder diagnosis, whereas Zimmerman and Coryell (1989) reported that approximately 18% of a nonclinical, community sample received a personality disorder diagnosis. Prevalence rates of personality disorders are also substantial outside of the United States. For example, the World Health Organization (WHO) and Alcohol, Drug Abuse, Mental Health Administration (ADAMHA) Joint Program on the Diagnosis and Classification of Mental Disorders, Alcoholism, and Drug Abuse initiated the International Pilot Study of Personality Disorders (Loranger et al., 1994). The first report from a field trial evaluating 716 patients from 11 countries indicated that 51.1% of the patients met criteria for at least one DSM-III-R personality disorder.
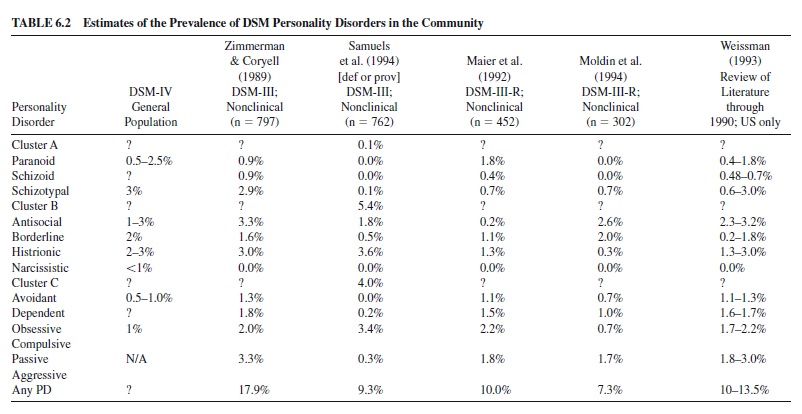
Although a number of large-scale, community epidemiological studies on Axis I disorders have been conducted, we know much less about the prevalence of personality disorders in the general population. Antisocial personality disorder was the only personality disorder included in the Epidemiological CatchmentArea (ECA) study (Robins & Regier, 1991) and the National Comorbidity Study (NCS; Kessler, 1999), from which most of our estimates on the prevalence of mental disorders in the community are drawn. Table 6.2 presents our best estimates of the prevalence of the full range of DSM personality disorders, drawn from the DSM-IV text (APA, 2000), several empirical studies (Maier, Lichtermann, Klinger, & Heun, 1992; Samuels, Nestadt, Romanoski, Folstein, & McHugh, 1994; Zimmerman & Coryell, 1989), and prior reviews (Lyons, 1995; Mattia & Zimmerman, 2001; Weissman, 1993). Across studies that used the DSM criteria to estimate the prevalence of current personality disorder (i.e., one or more diagnoses) the average estimate was 11.25% (range = 7.3–17.9%). For comparison, the past year prevalence estimates for major depressive episode were 3.7% (ECA) and 10.3% (NCS), for generalized anxiety disorder were 3.8% (ECA) and 3.1% (NCS), for alcohol use disorder were 6.3% (ECA) and 9.7% (NCS), and for drug use disorder were 1.2% (ECA) and 3.6% (NCS). Therefore, personality disorder does appear to be relatively prevalent in the community. The Cluster B disorders (especially antisocial, borderline, and histrionic) appear to be the most prevalent personality disorders.
Many studies have also documented that personality disorders are associated with significant social and occupational dysfunction, comorbid Axis I psychopathology, and even suicidal state (e.g., Bernstein et al., 1993; Daley, Burge, & Hammen, 2000; Johnson, Cohen, Brown, Smailes, & Bernstein, 1999; Trull, Useda, Conforti, & Doan, 1997), and these relations remain significant after controlling for Axis I disorder and demographic variables (e.g., age, gender). For example, one of the more well-validated personality disorders is the antisocial or psychopathic (Stoff, Breiling, & Maser, 1997). Persons who have met the diagnostic criteria for this personality disorder have been shown to be at significant risk for unemployment, impoverishment, injury, violent death, substance andalcoholabuse,incarceration,recidivism(paroleviolation), and significant relationship instability (Hart & Hare, 1997; L. N. Robins,Tipp, & Przybeck, 1991).
Maladaptive personality traits will be evident among many patients seeking treatment for an Axis I mental disorder. For example, Trull, Sher, Minks-Brown, Durbin, and Burr (2000) estimated that approximately 57% of patients with borderline personality disorder will meet criteria for one or more substance use disorders (primarily alcohol use disorder), whereas approximately 27% of those with one or more substance use disorders should also receive a borderline diagnosis.Thus, the comorbidity rates for the substance use and borderline personality disorder are quite substantial, and the presence of a personality disorder will often result in an increased utilization of mental health services (Bender et al., 2001).
Investigators have reported that a comorbid diagnosis of personality disorder in depressed, substance-abusing, and anxiety-disordered patients suggests poorer prognosis (Dolan-Sewell, Krueger, & Shea, 2001;Trull et al., 2000).Antisocial patients can be irresponsible, unreliable, or untrustworthy; paranoid patients can be mistrustful, accusatory, and suspicious; dependent patients can be excessively needy; passive-aggressive patients can be argumentative and oppositional; and borderline patients can be intensely manipulative and unstable (Sanderson & Clarkin, 1994; Stone, 1993). The manner and extent to which a patient’s personality facilitates and hinders clinical treatment—and the extent to and manner in which they result in clinically significant maladaptive functioning—should be a routine consideration of every clinician(Harkness&Lilienfeld,1997).“IntheDSM-III,then, personality not only attained a nosological status of prominence in its own right but was assigned a contextual role that made it fundamental to the understanding and interpretation of other psychopathologies” (Millon & Frances, 1987, p. ii).
In sum, the placement of personality disorders on a separate axis does have a meaningful rationale and justification, but the separate placement has also become controversial and perhaps misunderstood. Some have interpreted the placement on a separate axis to imply that personality disorders (along with mental retardation) are largely untreatable. Personality disorders are indeed among the most difficult of mental disorders to treat, in part because they involve pervasive and entrenched behavior patterns that have been present throughout much of a person’s life. In addition, people consider many of their personality traits to be integral to their sense of self, and they may even value particular aspects of their personality that a clinician considers to be important targets of treatment (Stone, 1993). Nevertheless, contrary to popular perception, personality disorders are not untreatable. Maladaptive personality traits are often the focus of clinical treatment (Beck, Freeman, & Associates, 1990; Linehan, 1993; Millon et al., 1996; Soloff, Siever, Cowdry, & Kocsis, 1994; Stone, 1993), and there is compelling empirical support to indicate that meaningful responsivity to treatment does occur (Perry, Banon, & Ianni, 1999; Sanislow & McGlashan, 1998). Treatment of a personality disorder is unlikely to result in the development of a fully healthy or ideal personality structure (whatever that may entail), but clinically and socially meaningful change to personality structure and functioning can occur.
Assessment of DSM-IV Personality Disorders
There are five methods commonly used for the assessment of personality disorders in research and general clinical practice: self-report inventories, unstructured clinical interviews, semistructured clinical interviews, projective techniques, and informant reports. Each of these methods is discussed briefly in turn.
First, several self-report inventories have been developed that include items that purportedly assess individual DSM-IV personality disorder criteria (e.g., the Personality Diagnostic Questionnaire–4; Hyler, 1994). However, because these instruments do not include appropriate time frames in their instructions (e.g., do not assess whether the diagnostic criteria were evident since young adulthood) and do not assess whether a clinically significant level of impairment or distress is associated with the endorsed personality disorder symptoms, self-report personality disorder inventories may be best suited for screening measures—not as diagnostic instruments. The prevalence rates obtained by these inventories tend to be dramatically higher than those estimated by interview measures of personality disorders and well beyond theoretical expectations for most of the personality disorders (Clark & Harrison, 2001; Kaye & Shea, 2000; Westen, 1997; Zimmerman, 1994). On the other hand, the tendency of selfreport inventories to err in the direction of overdiagnosis does make them suitable as screening measures. The administration of a self-report inventory prior to a clinical interview can save a considerable amount of interviewing time and alert the clinician to areas of personality dysfunction that might have otherwise not have been anticipated or noticed (Widiger, 2002). The generally preferred method of assessment in clinical practice is an unstructured clinical interview (Westen, 1997), whereas the preferred method within clinical research is the semistructured interview (Rogers, 1995; Zimmerman, 1994). Unstructured clinical interviews can be highly problematic because they are often idiosyncratic, less reliable, and more susceptible than are semistructured interviews to attributional errors, halo effects, and false assumptions, including gender biases (Garb, 1997; Widiger, 1998). Convergent validity data have been consistently weakest when one of the measures was an unstructured clinical interview (Widiger, 2002). A variety of studies have indicated that clinicians relying upon unstructured clinical interviews routinely fail to assess for the presence of the specified diagnostic criteria. One of the more compelling demonstrations of this failure was provided by Morey and Ochoa (1989). Morey and Ochoa provided 291 clinicians with the 166 DSM-III (APA, 1980) personality disorder diagnostic criteria and asked them to indicate, for one of their patients, which DSM-III personality disorder(s) were present and which of the 166 DSM-III personality disorder diagnostic criteria were present. Kappa for the agreement between their diagnoses and the diagnoses that would be given based upon their own assessment of the diagnostic criteria was poor, ranging from .11 (schizoid) to .58 (borderline), with a median kappa of only .25. These findings were subsequently replicated by Blashfield and Herkov (1996). “It appears that the actual diagnoses of clinicians do not adhere closely to the diagnoses suggested by the [diagnostic] criteria” (Blashfield & Herkov, 1996, p. 226).
Patients often meet the DSM-IV diagnostic criteria for more than one personality disorder, yet clinicians typically provide only one diagnosis to each patient (Gunderson, 1992). Clinicians tend to diagnose personality disorders hierarchically. After a patient is identified as having a particular personality disorder (e.g., borderline), clinicians often fail to assess whether additional personality traits are present (Herkov & Blashfield, 1995). Adler, Drake, and Teague (1990) provided 46 clinicians with case histories of a patient that met the DSM-III criteria for four personality disorders (i.e., histrionic, narcissistic, borderline, and dependent). “Despite the directive to consider each category separately . . . most clinicians assigned just one [personality disorder] diagnosis” (Adler et al., 1990, p. 127). Sixty-five percent of the clinicians provided only one diagnosis, 28% provided two, and none provided all four. Comorbidity among mental disorders is a pervasive phenomenon that can have substantial significance and importance to clinical treatment and outcome research(Clark,Watson,&Reynolds,1995;Sher&Trull,1996; Widiger & Clark, 2000), yet comorbidity may be grossly underrecognized in general clinical practice. Zimmerman and Mattia (1999b) compared the Axis I clinical diagnoses provided for 500 patients who were assessed with unstructured clinical interviews with the diagnoses provided by a semistructured interview. More than 90% of the patients receiving the unstructured clinical interview were provided with only oneAxis I diagnosis, whereas more than a third of the patients assessed with the semistructured interview were discovered to have met the diagnostic criteria for at least two additional Axis I disorders. Zimmerman and Mattia (1999a) also reported that clinicians diagnosed less than 1% of the patients with borderline personality disorder, whereas 14% were diagnosed with this disorder when a semistructured interview was used. Zimmerman and Mattia (1999a) then provided the clinicians with the additional information obtained by the more systematic semistructured interview. “Providing the results of [the] semistructured interview to clinicians prompts them to diagnose borderline personality disorder much more frequently” (Zimmerman & Mattia, 1999a, p. 1570). The rate of diagnosis increased from .4% to 9.2%.
The reluctance to use semistructured interviews in general clinical practice is understandable because they are constraining, may at times be impractical, and can appear to be superficial (Westen, 1997). However, they are particularly advisable when questions regarding the reliability or validity of an assessment are likely to be raised (Widiger, 2002). Semistructured interviews are helpful in ensuring that the interview will be systematic, comprehensive, replicable, and objective (Widiger & Coker, 2002). Diagnoses derived from the administration of a semistructured interview have often been used as the standard by which the validity of other measures are evaluated. Minimally, semistructured interviews are useful in providing to the clinician a set of useful suggestions for a variety of possible inquiries to use for the assessment of each diagnostic criterion.
Several semistructured interviews for the assessment of DSM-IV personality disorders are available (Clark & Harrison, 2001; Kaye & Shea, 2000; Widiger, 2002; Widiger & Coker, 2002; Zimmerman, 1994). Regrettably, there have been only a few studies concerned with their convergent validity.This limited research has suggested questionable validity with respect to agreement for the presence of categorical diagnoses but acceptable to good convergent validity with respect to the assessment of the extent to which respective personality disorder symptomatology are present (e.g., Skodol, Oldham, Rosnick, Kellman, & Hyler, 1991).
A potential disadvantage of self-report inventories and semistructured interviews is their emphasis on self-report (Bornstein, 1995; Westen, 1997). Personality disorders are characterized in part by distortions in self-image and selfpresentation, which may not be assessed adequately simply by asking respondents if they have each diagnostic criterion. However, it is important to emphasize that neither self-report inventories nor semistructured interviews rely upon accurate self-report. Semistructured interviews include many openended questions, indirect inquiries, and observations of the respondents’manner of relating to the interviewer. Interviewers administering a semistructured interview do not simply record respondents’ answers to queries, but are instead using their clinical expertise to rate each diagnostic criterion based in part on direct, indirect, and open-ended questions that have been found by experienced investigators to be effective for assessing whether a particular diagnostic criterion is present.
Projective tests are less dependent on the ability or willingness of a person to provide an accurate self-description (Bornstein, 1995), but there is currently only limited empirical support for the use of projective techniques for the assessment of the DSM-IV personality disorders. Supportive research has been reported for the assessment of histrionic, narcissistic, antisocial, and borderline personality traits (e.g., Blais, Hilsenroth, & Fowler, 1998; Hilsenroth, Handler, & Blais, 1996), but no projective test currently provides a systematic or comprehensive assessment of the DSM-IV personality disorders. There is also disagreement concerning the extent of the empirical support for projective tests (Acklin, 1999; Archer, 1999; Garb, 1999; Weiner, 1999; Wood & Lilienfeld, 1999).
An underutilized method of personality disorder assessment is informant report (Clark, Livesley, & Morey, 1997). Informants (e.g., family members, close friends) can provide an historical perspective on an individual’s personality functioning and thus may lack the significant personality or Axis I pathology that can complicate a patient’s self-description. Selfand informant assessments of personality disorder symptomatology often fail to agree, and it is not yet certain which perspective should be considered to be more valid (Bernstein et al., 1997; Riso, Klein, Anderson, Ouimette, & Lizardi, 1994; Widiger, 2002; Zimmerman, 1994). Relatives and close friends will not know everything about a person that would be necessary to provide a valid description, they may have their own axes to grind, and they may have false assumptions or expectations concerning the identified target. Nevertheless, informant reports of personality disorder features remains a promising method that deserves more research attention. Oltmanns and his colleagues have been conducting a particularly creative and intriguing investigation of the agreement and disagreement between self-descriptions and peer nominations of air force recruits (Oltmanns,Turkheimer, & Strauss, 1998).
The DSM-IV Personality Disorders
Up to this point, we have reviewed the definition of personality disorder, its clinical importance, and its assessment. In the following sections we describe briefly each of the 10 personality disorders included in DSM-IV.
Paranoid Personality Disorder
Description
Paranoid personality disorder (PPD) is characterized by an allpervasive distrust and suspiciousness of others (Miller, Useda, Trull, Burr, & Minks-Brown, 2001). To receive a DSM-IV PPD diagnosis, one must exhibit at least four of seven diagnostic criteria that are—for the most part—indicators of a suspicious interpersonal style and a tendency to read malevolent intentions into what are truly innocuous or neutral interactions or events (APA, 1994, 2000).As one might guess, individuals with PPD are rather difficult to get along with, and they are likely to be argumentative, hostile, and overly sarcastic. They may blame others for their own difficulties and misfortunes and are unlikely to be able to work collaboratively or closely with others. They might maintain a steady employment but will often be difficult coworkers because they tend to be rigid, controlling, critical, blaming, and prejudicial. They might become involved in lengthy, acrimonious, and litigious disputes that are difficult if not impossible to resolve.
Epidemiology
DSM-IV estimates that only 0.5–2.5% of the general population qualify for a PPD diagnosis, and epidemiological studies of community samples (see Table 6.2) support this estimate. Although PPD may be more prevalent in clinical samples, it is unlikely that PPD will be the patient’s presenting problem. The available studies indicate that more men than women are diagnosed with PPD (Corbitt & Widiger, 1995; Miller et al., 2001). There are no strong empirical data to suggest that members of certain racial or ethnic groups are more likely to receive a PPD diagnosis. In fact, DSM-IV cautions against overinterpreting anger and frustration in response to perceived neglect or guardedness sometimes exhibited by individuals from other cultures or backgrounds.
Etiology
There is little research to indicate a direct inheritance of PPD (McGuffin & Thapar, 1992; Nigg & Goldsmith, 1994). There has been research to indicate a genetic contribution to the development of paranoid personality traits, if these traits are conceptualized as being on a continuum with general personality functioning (Jang, McCrae, Angleitner, Reimann, & Livesley, 1998; Livesley, Jang, & Vernon, 1998; Nigg & Goldsmith, 1994). There is some support for a genetic relationship of PPD with schizophrenia and delusional disorder (persecutory type), but these findings have not always been replicated and the positive results may have been due in part to the overlap of PPD with the schizotypal personality disorder (Miller et al., 2001; Siever, 1992).
There has been speculation on the neurophysiology that might underlie the personality disorders within the oddeccentric cluster (Cloninger, 1998; Siever & Davis, 1991) but research has been confined largely to the schizotypal personality disorder. There has been little consideration given to the neurophysiological concomitants of nonpsychotic paranoid personality traits.
Attention has been given to cognitive and interpersonal models for the development of paranoid personality traits. Paranoid beliefs may have a self-perpetuating tendency due to the focus on signs of and evidence for malicious intentions (Beck et al., 1990). From this perspective, the pathology of PPD would be inherent to the irrationality of the belief systems and would be sustained by biased information processing. There might also be an underlying motivation or need to perceive threats in others and to externalize blame that help to sustain the accusations and distortions (Stone, 1993).
There are few systematic studies on psychosocial contributions to the development of PPD. There are retrospective data indicating that persons with this personality disorder considered their parents to be excessively critical, rejecting, withholding, and at times even abusive (e.g., Modestin, Oberson, & Erni, 1998; Norden, Klein, Donaldson, Pepper, & Klein, 1995); however, the retrospective nature of these studies is problematic (paranoid persons might not be providing accurate descriptions of prior relationships) and the childhood experiences that have been identified are not specific to this personality disorder (Miller et al., 2001). There are presently no prospective longitudinal studies that have explored the development of paranoid personality traits.
Premorbid traits of PPD that might be evident prior to adolescence include isolation, hypersensitivity, hypervigilance, social anxiety, peculiar thoughts, and idiosyncratic fantasies (APA, 1994, 2000). As children, they may appear odd and peculiar to their peers and may not have achieved to their capacity in school. Mistrust and suspicion is often evident in members of minority groups, immigrants, refugees, and other groups for whom such distrust is often a realistic and appropriate response to their social environment. It is conceivable that a comparably sustained experience through childhood and adolescence could contribute to the development of excessive paranoid beliefs that are eventually applied inflexibly and inappropriately to a wide variety of persons, but it can be very difficult to determine what is excessive or unrealistic suspicion and mistrust within a member of an oppressed minority (Alarcon & Foulks, 1996; Whaley, 1997). Paranoid suspiciousness could in fact be more closely associated with prejudicial attitudes, wherein a particular group in society becomes the inappropriate target of one’s anger, blame, and resentment.
Schizoid Personality Disorder
Description
Schizoid personality disorder (SZPD) is characterized by social detachment and isolation as well as by restricted emotional experience and expression (APA, 2000; Miller et al., 2001). Individuals with this personality disorder not only choose to be by themselves, but they also have little interest in establishing or maintaining interpersonal relationships. In addition, SZPD individuals show little emotional expression and may not even appear to experience much pleasure, joy, or sadness. They have few friendships. Those that do occur are likely to have been initiated by the other person. They will have had few sexual relationships and may never marry. Relationships will fail to the extent to which the other person desires or needs emotional support, warmth, and intimacy. Persons with SZPD may do well within an occupation as long as substantial social interaction is not required. They would prefer to work in isolation. They may eventually find employment and a relationship that is relatively comfortable or tolerable to them, but they could also drift from one job to another and remain isolated throughout much of their lives. If they do eventually become parents, they have considerable difficulty providing warmth and emotional support and may appear neglectful, detached, and disinterested.
Epidemiology
SZPD, as diagnosed by DSM-IV, does appear to be relatively uncommon in both clinical and nonclinical settings. Estimates of this disorder in the general population have been less than 1% (see Table 6.2). Over the years, the definition of SZPD has become more restricted, and many of the features once associated with this disorder prior to DSM-III (APA, 1980) are now part of the criterion sets of other disorders (e.g., avoidant and schizotypal; Miller et al., 2001). DSM-IV states that SZPD is diagnosed more frequently in men than in women; however, the empirical findings are mixed (Corbitt & Widiger, 1995). It is also important to caution against overdiagnosing SZPD in individuals from other cultures or minority ethnic backgrounds. Such individuals may appear somewhat introverted or isolated, as well as emotionally aloof, simply because they are being interviewed or observed by someone from another culture or because their culture is not, on average, as affiliative or emotionally expressive as the majority cultures in the United States.
Etiology
There is little research to indicate a direct inheritance of SZPD (McGuffin & Thapar, 1992; Nigg & Goldsmith, 1994). A substantial amount of research has supported the heritability for the general personality dimension of introversion (Jang & Vernon, 2001; Plomin & Caspi, 1999), and SZPD does appear to be essentially equivalent to the social withdrawal and anhedonia evident within extreme introversion (Trull, 1992; Trull et al., 1998). A genetic association with schizophrenia has at times been reported, but this association might be explained by the overlap of SZPD with schizotypal personality traits (Fulton & Winokur, 1993; Miller et al., 2001; Siever, 1992).
Psychosocial models for the etiology of SZPD are lacking. It is possible that a sustained history of isolation during infancy and childhood, with an encouragement or modeling by parental figures of interpersonal withdrawal, social indifference, and emotional detachment could contribute to the development of schizoid personality traits, but there is no systematic research to support this hypothesis. Persons with SZPD are likely to have been socially isolated and withdrawn as children. They may not have been accepted well by their peers and may have even been the brunt of some ostracism (APA, 1994, 2000). However, systematic research on the childhood development of SZPD is lacking (Bernstein & Travaglini, 1999; Milleretal., 2001). The central pathology of SZPD might be anhedonic deficits, or an excessively low ability to experience positive affectivity (Rothbart & Ahadi, 1994; Siever, 1992). A fundamental distinction of schizophrenic symptomatology is between positive and negative symptoms. Positive symptoms include hallucinations, delusions, inappropriate affect, and loose associations; negative symptoms include flattened affect, alogia, and avolition. SZPD may represent subthreshold negative symptoms, comparable to the subthreshold positive symptoms (cognitive-perceptual aberrations) that predominate schizotypal PD.
Schizotypal Personality Disorder
Description
Schizotypal personality disorder (STPD) is characterized by a pervasive pattern of interpersonal deficits, cognitive and perceptual aberrations, and behavioral eccentricities (APA, 2000; Miller et al., 2001). Persons with STPD exhibit excessive social anxiety that is related to paranoid fears. They also appear odd, eccentric, or peculiar in their behavior or appearance, display inappropriate or constricted affect, and have few (if any) friends or confidants outside of their immediate family. Also striking are the STPD individual’s unusual ideas, beliefs, and communication. Those with this personality disorder tend to misinterpret or overpersonalize events, to hold unusual ideas that influence behavior (e.g., telepathy, clairvoyance), and to have difficulty being understood by others. They may drift toward esoteric, fringe groups that support their magical thinking and aberrant beliefs. These activities can provide structure for some persons with STPD, but they can also contribute to a further loosening and deterioration if there is an encouragement of psychotic-like or dissociative experiences.
Persons with STPD are most likely to seek treatment for anxiety or mood disorders rather than seek treatment for the symptoms specific to STPD. Individuals with STPD may experience transient psychotic episodes especially in response to stress. However, these episodes are relatively brief (i.e., lasting a few minutes to a few hours) and are typically of insufficient duration to warrant an Axis I psychotic diagnosis. Only a small proportion of persons with STPD develop schizophrenia, but many may eventually develop a major depression. The symptomatology of STPD does not appear to remit with age (Siever, 1992). The course appears to be relatively stable, with some proportion of schizotypal persons remaining marginally employed, withdrawn, and transient though much of their lives.
Epidemiology
Although DSM-IV reports that STPD may occur in up to 3% of the population, most estimates using structured diagnostic interviews to assess STPD are lower and closer to 1% (see Table 6.2). STPD appears to be slightly more common in men. Little is known about the prevalence of this disorder in nonwestern cultures.
Etiology
There is empirical support for a genetic association of STPD with schizophrenia (McGuffin & Thapar, 1992; Nigg & Goldsmith, 1994), which is consistent with the fact that the diagnostic criteria for STPD were obtained from studies of the biological relatives of persons with schizophrenia (Miller et al., 2001). A predominant model for the psychopathology of STPD is deficits or defects in the attention and selection processes that organize a person’s cognitive-perceptual evaluation of and relatedness to his or her environment (Siever & Davis, 1991). These deficits may lead to discomfort within social situations, misperceptions and suspicions, and to a coping strategy of social isolation. Correlates of central nervous system dysfunction seen in persons with schizoprenia have been observed in laboratory tests of persons with STPD, including performance on tests of visual and auditory attention (e.g., backward masking and sensory gating tests) and smooth pursuit eye movement that might be associated with dysregulation along dopaminergic pathways (Siever, 1992). As children, persons with STPD are likely to have been notably isolated. They may have appeared peculiar and odd to their peers, and may have been teased or ostracized. Achievement in school was likely to have been impaired, and they may have been heavily involved in esoteric fantasies and peculiar games—particularly those that do not involve peers (APA, 1994, 2000). Empirical support for the childhood development of STPD, however, is limited.
Antisocial Personality Disorder
Description
Antisocial personality disorder (ASPD) is characterized by a pattern of behavior that reflects an extreme disregard for and violation of the rights of others. The DSM-IV diagnostic criteria for ASPD include deceitfulness, impulsivity, irritabilityaggressiveness, acts of criminality, and irresponsibility (APA, 2000). Persons with ASPD often commit reckless acts that neglect to consider the safety of others, and they lack remorse for the harm they have inflicted. Additional features of ASPD not included within the DSM-IV diagnostic criteria include arrogance, superficial charm, exploitativeness, and a lack of empathy (Hare, 1991; Sutker & Allain, 2001). Persons with ASPD are unlikely to maintain steady employment. Some persons with ASPD can obtain professional and criminal success for periods of time, as long as their exploitations, violations, deceptions, and manipulations are not discovered. Their success, however, may at some point unravel, due in part to their impulsivity, negligence, and lack of foresight. A similar pattern may occur within their social and sexual relationships. They may at first appear to be quite successful socially, as they can be charming, fun, and engaging, but many of their relationships will eventually fail as a result of their lack of empathy, fidelity, and responsibility, as well as episodes of abuse, exploitation, and angry hostility.
ASPD is evident in childhood in the form of a conduct disorder (e.g., aggression toward persons and animals, destruction of property, deceitfulness or theft, and serious violations of laws and rules). Evidence of conduct disorder before the age of 15 is in fact required for the DSM-IV diagnosis of ASPD (APA, 2000). However, it is important to emphasize that not all children with conduct disorder will meet the criteria for ASPD as an adult. A continuation into adulthood is more likely to occur if multiple delinquent behaviors are evident before the age of 10 (Hinshaw, 1994).
Epidemiology
It is estimated that the prevalence rate for ASPD is about 3% in men and about 1% in women (L. N. Robins et al., 1991). High rates of this personality disorder are seen in substance abuse treatment settings and in forensic settings. Up to 50% of males within prison settings meet the DSM-IV criteria for ASPD, but this could be due in part to a lack of adequate specificity of the diagnostic criteria within prison settings (Hare, 1991). Although ASPD is more common among those from lower socioeconomic classes and those in urban settings, the direction of the causality for this relationship is unclear. This correlation may reflect that persons with ASPD migrate to urban settings and become more socially or economically impoverished or that economic impoverishment contributes to the development of antisocial traits.
Etiology
There is considerable support from twin, family, and adoption studies for a genetic contribution to the etiology of the criminal, delinquent tendencies of persons with ASPD (McGuffin & Thapar, 1992; Nigg & Goldsmith, 1994; Stoff et al., 1997; Sutker & Allain, 2001). The genetic disposition can be more evident in females with ASPD due in part to a greater social pressure on females against the development of aggressive, exploitative, and criminal behavior.
Abnormally low levels of anxiousness, constraint, and arousal have been implicated in the development of ASPD. Research has suggested that individuals with ASPD demonstrate a hyporeactive electrodermal response to stress that is associated with a commonly studied domain of normal personality functioning—neuroticism or negative affectivity (Patrick, 1994). These findings are consistent with developmental research concerned with the interaction of parenting and temperament (e.g., low anxiousness and low inhibition) on the development of a moral conscience (Kochanska, 1991). From this perspective, the pathology of psychopathy might not be a deficit that is qualitatively distinct from general personality functioning (Widiger & Lynam, 1998). “The observed absence of startle potentiation in psychopaths . . . may reflect a temperamental deficit in the capacity for negative affect” (Patrick, 1994, p. 425).
Activities that the average person would find stimulating might be found by psychopathic persons to be dull, impelling them perhaps to engage in risky, reckless, prohibited, and impulsive activities. Abnormally low levels of arousal would also minimize feelings of anxiety, guilt, or remorse and help resist aversive conditioning. The development of normal levels of guilt, conscience, and shame may require a degree of distress-proneness (neuroticism or negative affectivity) and attentional self-regulation (constraint). Normal levels of anxiousness promote the internalization of conscience (the introjection of the family’s moral values) by associating distress and anxiety with wrongdoing, and the temperament of selfregulation helps modulate impulses into a socially acceptable manner (Kochanska, 1991).
There are also substantial data to support the contribution of family, peer, and other environmental factors, although no single environmental factor appears to be specific to its development (Stoff et al., 1997; Sutker & Allain, 2001). Modeling of exploitative, abusive, and aggressive behavior by parental figures and peers; excessively harsh, lenient, or erratic discipline; and a tough, harsh environment in which feelings of empathy and warmth are discouraged (if not punished) and tough-mindedness, aggressiveness, and exploitation are encouraged (if not rewarded) have all been associated with the development of ASPD. For example, ASPD in some cases could be the result of an interaction of early experiences of physical or sexual abuse, exposure to aggressive parental models, and erratic discipline that develop a view of the world as a hostile environment, which is further affirmed over time through selective attention on cues for antagonism, encouragement and modeling of aggression by peers, and the immediate benefits that result from aggressive behavior (Dodge & Schwartz, 1997; Farrington, 1997).
Borderline Personality Disorder
Description
Borderline personality disorder (BPD) is characterized by a pattern of impulsivity and instability in affect, interpersonal relationships, and self-image. According to DSM-IV, at least five of nine criteria must be present for a BPD diagnosis (APA, 2000). Table 6.3 provides these diagnostic criteria for BPD. As can be seen from Table 6.3, those diagnosed with BPD frequently experience strong, intense negative emotions and are prone to suicidal threats, gestures, or attempts. They are unsure of their self-image as well as their own views of other people. They harbor intense abandonment fears and feelings of emptiness. Stressful situations may invoke transient paranoid ideation or dissociation. Associated features include a propensity for engaging in self-defeating behavior (e.g., making a bad decision that destroys a good relationship), high rates of mood or substance use disorders, and premature death from suicide. Approximately 3–10% will have committed suicide by the age of 30 (Gunderson, 2001).
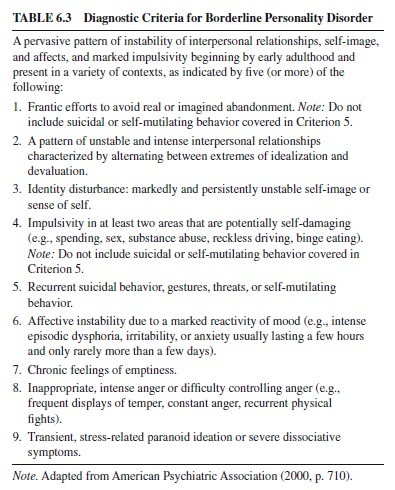
Epidemiology
It is estimated that approximately 2% of the general population meets diagnostic criteria for BPD. BPD is the most frequently diagnosed personality disorder in both inpatient and outpatient settings (Adams, Bernat, & Luscher, 2001; Gunderson, 2001). It is believed that more women than men meet the criteria for BPD, but this belief is based primarily on clinical studies. It is important to distinguish BPD symptoms, which are chronic and pervasive, from borderline behaviors that may be exhibited for short periods of time in adolescence. Studies that have followed over time children and adolescents who initially received a BPD diagnosis find that only a small percentage still have a BPD diagnosis years later. This finding raises the possibility that BPD may be overdiagnosed in children and adolescents.
Etiology
There are studies to suggest a genetic disposition specific to BPD, but research has also suggested an association with mood and impulse disorders (McGuffin & Thapar, 1992; Nigg & Goldsmith, 1994). There is also empirical support for a childhood history of physical abuse, sexual abuse, or both, as well as parental conflict, loss, and neglect (Gunderson, 2001; Johnson et al., 1999; Silk, Lee, Hill, & Lohr, 1995; Zanarini, 2000). It appears that past traumatic events are important in many if not most cases of BPD, contributing to the development of malevolent perceptions of others (Ornduff, 2000) and a comorbidity with posttraumatic stress, mood, and dissociative disorders. BPD may involve the interaction of a genetic disposition for lack of mood and impulse control with an evolving series of intense and unstable relationships (Bartholomew, Kwong, & Hart, 2001; Paris, 2001). Linehan (1993) hypothesizes that persons with a borderline personality disorder failed to learn important and useful skills for regulating emotional arousal and tolerating emotional distress; they learned instead that drug abuse, promiscuity, and selfinjurious behavior produce temporary relief from stress.
There are numerous theories regarding the pathogenic mechanisms of BPD; most concern expectations of abandonment, separation, exploitative abuse, or any combination of these (Gunderson, 2001). Persons with BPD have usually had quite intense, disturbed, or abusive relationships with the significant persons of their lives, including their parents. They continue to expect and may even recreate unstable and intense relationships throughout their adult lives. Persons with BPD may require numerous hospitalizations due to their lack of affect and impulse control, psychotic-like and dissociative symptomatology, and risk of suicide (Stone, 2001). Minor problems quickly become crises as the intensity of affect and impulsivity contribute to disastrous life decisions. They are at a high risk for developing depressive, substance-related, bulimic, and posttraumatic stress disorders (Adams et al., 2001). The potential for suicide is increased with a comorbid mood and substance-related disorder.
Histrionic Personality Disorder
Description
Histrionic personality disorder (HPD) is characterized by pervasive and excessive emotionality and attention seeking (Widiger & Bornstein, 2001). The DSM-IV criteria for HPD include actions and behaviors that serve to place one in the center of attention, behavior that is provocative or inappropriately intimate, fleeting and superficial emotional expression, and suggestibility (APA, 2000). Persons with HPD tend to experience difficulty both in romantic relationships and in friendships. They have trouble balancing their strong needs for attention and intimacy with the reality of the situation. It is often difficult for those with HPD to delay gratification, and they are prone to act impulsively. Persons with this disorder are said to have a pathologic need to be loved, desired, and involved with others on an intimate basis, and they use a variety of means to get this involvement (Horowitz, 1991). They use their physical appearance to draw attention to themselves, they are melodramatically emotional, and they are inappropriately seductive. They may even perceive a relationship as being more intimate than is really the case, in part because of their need for romantic fantasy.
Epidemiology
As indicated in Table 6.2, about 2–3% of the general population is believed to meet criteria for an HPD diagnosis. HPD is more prevalent among women, but it is important to keep cultural, gender, and age norms in mind when judging whether a given behavioral feature is indicative of HPD. The diagnostic criteria for HPD resemble closely stereotypic femininity, and clinicians at times overdiagnose HPD in women (Widiger, 1998). Cultural groups also differ in their degrees of emotional expression. It is only when the degree of emotional expression is excessive (within a cultural group) and causes distress or impairment that it should be considered symptomatic of HPD. HPD is likely to be diagnosed in some cultural groups more than in others. For example, the disorder might be seen less frequently in Asian cultures, in which overt sexual seductiveness is less frequent (Johnson, 1993) and more frequently within Hispanic and Latin American cultures, in which more overt and uninhibited sexuality is evident (Padilla, 1995). It can be difficult to determine when or how adjustments to the diagnostic criteria should be made within these different cultural contexts because the DSM-IV criteria may also reflect biases or assumptions regarding seductiveness that are not shared within other societies (Alarcon, 1996; Rogler, 1996).
Etiology
There has been little research on the etiology of HPD. There is some limited support for the heritability of histrionic personality traits, but there has not yet been a familial aggregation, twin, or adoption study of this disorder (Jang & Vernon, 2001; McGuffin & Thapar, 1992; Nigg & Goldsmith, 1994). There are data to suggest that HPD is a constellation of maladaptive variants of common personality traits within the broad domains of neuroticism and extraversion (Trull, 1992; Trull et al., 1998). For example, normal extraversion includes the dispositions to be outgoing, talkative, and affectionate; to be convivial, to have many friends, and to seek social contact; to be energetic, fast-paced, and vigorous; to be flashy, seek stimulation, and take risks; and to be high-spirited (Costa & McCrae, 1992). Traits of extraversion are for the most part desirable and adaptive, but persons who are at the most extreme variants of these traits are likely to be histrionic and experience a number of maladaptive consequences (Trull, 1992). To the extent that HPD does indeed include maladaptively extreme variants of the personality traits of extraversion, there would be support for its heritability (Jang et al., 1998; Nigg & Goldsmith, 1994).
A variety of parent-child relationships may contribute to the development of HPD (Bornstein, 1999). Histrionic needs may develop in part through an overly eroticized parent-child relationship. For example, a father might repeatedly indicate through a variety of verbal and nonverbal communications that his love and attention for a daughter are largely contingent upon her being attractive, desirable, and provocative to him. Her sense of self-worth and meaning might be dependent in large part on how he relates to her, and she might then value herself primarily in terms of how she is valued by men (Millon et al., 1996; Stone, 1993). Empirical support for this developmental model of HPD, however, is lacking.
Neurochemical models of the disorder have emphasized a hyperresponsiveness of the noradrenergic system. This dysregulation in catecholamine functioning may contribute to a pronounced emotional reactivity to signs of rejection (Klein, 1999). There may be a naturally occurring neurochemical mechanism for the regulation of mood in response to signs of social applause and rejection. This regulatory mechanism would be helpful sociobiologically in making a person appropriately responsive to cues of social interest, but excessive responsivity of the noradrenergic system might also result in oversensitivity to attention and rejection.
Narcissistic Personality Disorder
Description
Narcissistic personality disorder (NPD) is characterized by grandiosity, a need for admiration, and a lack of empathy for others (APA, 2000; Widiger & Bornstein, 2001). Persons with NPD tend to have an exaggerated sense of selfimportance and to believe that they are so unique that they can only be understood by similarly special people. These self-views lead to interpersonal behaviors that prove to be problematic—arrogance, exploitativeness, and a sense of entitlement. Despite the veneer of high self-confidence and self-esteem, those with NPD are quite vulnerable to real or perceived threats to their status. Therefore, it is not uncommon to seerage or counterattacks.As might be expected, NPD individuals tend to have serial friendships, which end when others discontinue their willingness to express admiration or envy. NPD individuals’ intolerance of criticism or perceived defeat may keep them from high levels of achievement.
Epidemiology
According to estimates (see Table 6.2), NPD seems relatively rare in the general population (i.e., less than 1%). NPD is also among the least frequently diagnosed personality disorders within clinical settings (Widiger & Bornstein, 2001). This personality disorder does appear to be more prevalent among men, but systematic epidemiological studies have not been conducted. It is important not to mistake an idealism that is characteristic of adolescents and young adults (e.g., stating a strong belief that one will become a surgeon) with the traits and behaviors of NPD. It is only when such beliefs are excessive (i.e., extremely unrealistic) and cause significant distress or impairment that we see them as indicative of NPD.
Cross-cultural studies of narcissism and narcissistic personality disorder would be of interest. NPD is the only DSM-IV personality disorder that is not given official recognition with in the WHO’s (1992) international nomenclature. Some theorists have in fact suggested that NPD is distinctly cultural, arguing that pathological narcissism is the manifestation of a modern, Western society that has become overly self-centered and materialistic, coupled with a decreasing importance of familial (interpersonal) bonds (Cooper & Ronningstam, 1992).
Etiology
There has not yet been a familial aggregation, twin, or adoption study of NPD (McGuffin & Thapar, 1992). The predominant models for the etiology of narcissism have been largely social learning or psychodynamic. One model proposes that narcissism develops through an excessive idealization by parental figures, which is then incorporated by the child into his or her self-image (Millon et al., 1996). Narcissism may also develop through unempathic, neglectful, inconsistent, or even devaluing parental figures who have failed to adequately mirror a child’s natural need for idealization (Cooper & Ronningstam, 1992). The child may find that the attention, interest, and perceived love of a parent are contingent largely on achievements or successes. They may fail to perceive the parents as valuing or loving them for their own sake but may instead recognize that the love and attention are largely conditional on successful accomplishments (Widiger & Bornstein, 2001).They might then develop the belief that their own feelings of self-worth are dependent upon a continued recognition of their achievements and successes by others. Conflicts and deficits with respect to self-esteem do appear to be central to the pathology of the disorder (Stone, 1993). Narcissistic persons continually seek and obtain signs and symbols of recognition to compensate for conscious or perhaps even unconscious feelings of inadequacy. Empirical support for the validity of hypotheses concerning narcissistic pathology are being provided by social-psychological (as well as clinical) research. Rhodewalt, Madrian, and Cheney (1998), for example, indicated how narcissism is more highly correlated with instability in selfesteem than with simply a consistently high self-confidence. Narcissism is perhaps a maladaptive process of regulating or protecting a fragile self-esteem in part through gaining the approval and admiration of others (Raskin, Novacek, & Hogan, 1991). Baumeister and his colleagues have been exploring the contribution of narcissistic conflicts to the occurrence of aggressive, violent behavior (Baumeister, Smart, & Boden, 1996; Bushman & Baumeister, 1998). They demonstrated empirically, for example, that neither low nor high self-esteem was predictive of reacting aggressively to threat. It was instead a combination of vulnerable self-esteem and injurious insult.
Avoidant Personality Disorder
Description
Avoidant personality disorder (AVPD) is characterized by a pervasive pattern of timidity, inhibition, feelings of inadequacy, and social hypersensitivity (APA, 2000; Bernstein & Travaglini, 1999). Those with AVPD for the most part avoid situations (occupational or otherwise) that require significant interpersonal contact. Therefore, they are seen as shy or loners. This interpersonal stance seems driven by the belief that they are inept, unappealing, or inferior. AVPD individuals are afraid of being embarrassed or rejected by others. They only become involved with others in situations in which they feel certain they will be accepted or liked. AVPD individuals want close relationships, but their fears keep them from initiating and maintaining contacts. Associated features of AVPD include hypervigilance (especially in social situations), low self-esteem, and a proneness both to anxiety disorders and to mood disorders.
Occupational success may not be significantly impaired as long as there is little demand for public performance. Through a job or career, persons with AVPD may in fact find considerable gratification and esteem that they are unable to find within their relationships. The job can serve as a distraction from intense feelings of loneliness. Their avoidance of social situations impairs their ability to develop adequate social skills, and their impaired social skills then further handicap their efforts to develop relationships. However, they may eventually develop an intimate relationship to which they often cling dependently. Persons with AVPD are prone to mood and anxiety disorders—particularly depression and social phobia.
Epidemiology
Timidity, shyness, social insecurity, and other features of AVPD are not uncommon problems, and AVPD is one of the more prevalent personality disorders within clinical settings (Mattia & Zimmerman, 2001). However, AVPD may be diagnosed in only 1% of the general population (see Table 6.2). It appears to occur equally among males and females, with some studies reporting more males and others reporting more females.
Etiology
AVPD appears to be an extreme variant of the general personality traits of introversion and neuroticism (Trull, 1992; Trull et al., 1998), both of which have substantial heritability (Jang & Vernon, 2001; Plomin & Caspi, 1999). Most children and adolescents have many experiences of interpersonal embarrassment, rejection, or humiliation, but these experiences are particularly devastating to the person who is already lacking in self-confidence and is temperamentally anxious and introverted (Rothbart & Ahadi, 1994). Persons with AVPD will have been shy, timid, and anxious as children. Many will have been diagnosed with a social phobia. Adolescence will have been a particularly difficult developmental period, due to the importance at this time of attractiveness, dating, and popularity.
AVPD may involve elevated peripheral sympathetic activity and adrenocortical responsiveness, resulting in excessive autonomic arousal, fearfulness, and inhibition. Just as ASPD may involve deficits in the functioning of a behavioral inhibition system, AVPD may involve excessive functioning of this same system. The pathology of AVPD, however, may also be more psychological than neurochemical; the timidity, shyness, and insecurity may be a natural result of a cumulative history of denigrating, embarrassing, and devaluing experiences. UnderlyingAVPD may be excessive self-consciousness, feelings of inadequacy or inferiority, and irrational cognitive schemas that perpetuate introverted, avoidant behavior (Beck et al., 1990).
Dependent Personality Disorder
Description
Dependent personality disorder (DPD) is characterized by a pervasive, excessive need to be cared for, leading to submissiveness, clinging behavior, and fears of separation (APA, 2000; Widiger & Bornstein, 2001). DPD individuals tend to give their lives over to others—they ask for advice and guidance about even the smallest of decisions, exude helplessness, and readily abdicate responsibility for most areas of their lives. They are so fearful that others may reject or leave them that they do not express disagreements and may even volunteer to do unpleasant, demeaning tasks in order to gain nurturance and approval. As might be expected, DPD individuals are prone to low self-esteem, self-doubt, and selfderogation, leading to mood and anxiety disorders. Their neediness and desperation often prevents them from carefully selecting a person who will in fact be protective and supportive. They often choose their partners indiscriminately and become quickly attached to persons who are unreliable, unempathic, and even exploitative or abusive. They might feel that either they deserve an inadequate partner or may even select an inadequate partner to try to work through or resolve their long-standing interpersonal conflicts and feelings of inadequacy (Stone, 1993).
Epidemiology
DPD appears to be among the more prevalent of the personality disorders in clinical settings. However, the rate of DPD in the general population does not appear to be very high (see Table 6.2). Most studies that have been conducted report higher prevalence rates of DPD in women than in men (Corbitt & Widiger, 1995). The prevalence and diagnosis of dependent personality disorder may also vary across cultures (Foulks, 1996) because there are profound differences in the extent to which societies encourage and value dependencyrelated behaviors. Many Western societies do appear to place more emphasis and value upon expressions of autonomy and self-reliance and might then be prone to overdiagnose the disorder (Bornstein, 1992). In some cultures, such as the Japanese or Indian cultures, interpersonal connectedness and interdependency are more highly valued, and what is considered dependency within the American culture might not be considered pathological within another culture.
Etiology
O’Neill and Kendler (1998) reported the results of a longitudinal study of 2,230 twins who had been administered a measure of interpersonal dependency. The results suggested a modest genetic influence and a large specific environmental contribution. DPD may represent an interaction of an anxious, fearful temperament with an insecure attachment to an inconsistent or unreliable parental figure (McGuffin & Thapar, 1992). Dependent persons may turn to a parental figure to provide a reassurance and sense of security that they are unable to generate for themselves. This empirically supported etiological model (Rothbart & Ahadi, 1994) is consistent with current object relations theory in which dependent personality traits are considered to be an internalization of the mental representation of the self as weak and ineffectual, contributing to a disposition to look to others to provide protection and support, to become preoccupied with fears of abandonment, and to develop feelings of helplessness and insecurity (Blatt, Cornell, & Eshkol, 1993; Bornstein, 1992). In an intriguing cross-generational laboratory study, Thompson and Zuroff (1998) demonstrated how dependent mothers tended to reward mediocre over excellent performances by their daughters.
A number of studies have documented a relationship between the dependent person’s weak and ineffectual self-image, excessive need to please others, and a variety of interpersonal problems (Bornstein, 1999). For example, Santor and Zuroff (1997) demonstrated how dependent persons were excessively concerned with maintaining interpersonal relatedness, adopting the responses of friends, and minimizing disagreement. Studies have also indicated that dependent personality traits provide a vulnerability to the development of clinically significant episodes of depression—particularly in response to interpersonal rejection or loss (Blatt & Zuroff, 1992). Methodological concerns have been raised with respect to this research (Coyne & Whiffen, 1995; Widiger, Verheul, & van den Brink, 1999), but there does appear to be a sufficient number of replicated, well-designed prospective studies to support the hypothesis that dependency does provide a vulnerability to episodesofdepression(C. J.Robins,Hayes,Block,Kramer,& Villena, 1995). For example, Hammen et al. (1995) obtained 6-month and 12-month follow-up assessments of 129 high school senior women. They conducted multiple regression analyses to predict depression on the basis of dependency cognitions, prior interpersonal stress, and the interaction between them, controlling for initial levels of depression. All of the young women experienced stressful life events during this period of their lives, including moving away from home, separation from an important relationship, and loss of a romantic partner, but most of them did not become depressed. “Itwasthe women with cognitions about relationships representing concerns about rejection or untrustworthiness of others who were especially challenged by normative changes” (Hammen et al., 1995, p. 441).
Obsessive-Compulsive Personality Disorder
Description
Obsessive-compulsive personality disorder (OCPD) is characterized by a preoccupation with orderliness, perfectionism, and control (APA, 2000; McCann, 1999). OCPD individuals tend to be rigid, stubborn, and perfectionistic to the point of impairment (e.g., tasks never get completed). Their preoccupation with rules, details, and morality cause them trouble both at work and outside of work. They are seen as inflexible and miserly and may be described by others as control freaks and workaholics. Other features of this personality disorder include hoarding, indecisiveness, reluctance to delegate tasks, being devoid of affection, ruminative, and prone to outbursts of anger. OCPD individuals often have comorbid anxiety disorders or mood disorders.
Many persons with OCPD obtain good to excellent success within a job or career. They can be excellent workers to the point of excess, sacrificing their social and leisure activities, marriage, and family for their job. Relationships with a spouse and children are likely to be strained due to their tendency to be detached and uninvolved but also authoritarian and domineering. A spouse may complain of a lack of affection, tenderness, and warmth. Relationships with colleagues at work may be equally strained by the excessive perfectionism, domination, indecision, worrying, and anger. Jobs that require flexibility, openness, creativity, or diplomacy may be particularly difficult (McCann, 1999). Persons with OCPD may be prone to various anxiety and physical disorders that are secondary to their worrying, indecision, and stress. Those with concomitant traits of angry hostility may be prone to cardiovascular disorders. Mood disorders may not develop until the person recognizes the sacrifices that have been made by their devotion to work and productivity, which may at times not occur until middle age. However, most experience early employment or career difficulties and even failures that may result in depression.
Epidemiology
OCPD is characteristic of about 2% of the general population (see Table 6.2). It is believed that rates of OCPD in men are about twice those found in women. Clinicians must be careful not to overdiagnose OCPD. A number of individuals are conscientious, devoted to their work, very organized, and have perfectionistic tendencies. However, it is only when these features are associated with significant distress or impairment that they can be considered indicators of OCPD.
Etiology
A variety of studies have indicated heritability for the trait of obsessiveness (Nigg & Goldsmith, 1994). OCPD may also relate to the general personality trait of constraint or conscientiousness (Trull, 1992; Trull et al., 1998) and the childhood temperament of attentional self-regulation, both of which have demonstrated substantial heritability (Plomin & Caspi, 1990). As children, some persons with OCPD may have appeared to be relatively well-behaved, responsible, and conscientious. However, they may have also been overly serious, rigid, and constrained (Rothbart & Ahadi, 1994).
Early psychoanalytic theories regarding OCPD concerned issues of unconscious guilt or shame. A variety of underlying conflicts have subsequently been proposed, including a need to maintain an illusion of infallibility to defend against feelings of insecurity, an identification with authoritarian parents, or an excessive, rigid control of feelings and impulses (McCann, 1999; Oldham & Frosch, 1991). Any or all of the aforementioned conflicts may in fact be important for a particular person with OCPD. OCPD involves an extreme variant of traits that are highly valued within most cultures (i.e., conscientiousness). Some persons may exaggerate cultural expectations as a result of excessive demands or pressures by parental figures. However, there have been few systematic studies on the developmental history or etiology of OCPD.
Future Directions in Personality Disorder Research
Personality disorders were placed on a separate axis in DSM-III in recognition of their unique importance to clinical practice (Frances, 1980; Spitzer, Williams, & Skodol, 1980). The placement on a separate axis may have also in turn contributed to an increased interest in the study of personality disorders by clinicians and researchers. Prior to DSM-III, only ASPD received much systematic empirical research. Since DSM-III was published, BPD (Gunderson, 2001) and STPD (Siever, 1992) have received a considerable amount of attention by researchers. Researchers have also been turning their attention to the dependent and narcissistic personality disorders (Bornstein, 1992, 1999; Bushman & Baumeister, 1998). Regrettably, very little attention has been given to the others, outside of their inclusion within broad, nonspecific studies in which all of the personality disorders are considered without much attention to hypotheses that are specific to individual personality disorders (e.g., Johnson et al., 1999; Modestin et al., 1998; Norden et al., 1995).
In this last section, we would like to highlight what we view to be important future directions in personality disorder research. We emphasize in particular research concerning the childhood, developmental precursors to adult personality disorder and their biological mechanisms. We also suggest that a better understanding of the DSM-IV personality disorders will be achieved when their conceptualization is integrated within more general models of personality functioning. A considerable amount of research has been devoted to the study of general personality functioning, and the science of personality disorders may progress to the extent that it incorporates this knowledge.
Childhood Development of Maladaptive Personality Traits
One of the more remarkable gaps in knowledge is the childhood antecedents for personality disorders (Widiger & Clark, 2000). Included in DSM-III (APA, 1980) were four childhood antecedents of the personality disorders: identity disorder as an antecedent of BPD, avoidant disorder as an antecedent of AVPD, oppositional defiant disorder for passive-aggressive personality disorder, and conduct disorder for ASPD. Only the childhood antecedents for ASPD are still included within the diagnostic manual. Empirical support for the childhood antecedents of ASPD are so compelling that evidence of their presence is required for its diagnosis (APA, 2000), yet there are almost no data on the childhood antecedents for most of the other personality disorders.
Prospective longitudinal studies from childhood into adulthood are needed to document empirically how maladaptive personality traits develop, sustain, alter, or remit in their presentation across the life span (Caspi, 1998; Sher & Trull, 1996; Widiger & Sankis, 2000). For example, Trull, Useda, Conforti, and Doan (1997) and Lenzenweger, Loranger, Korfine, and Neff (1997) are conducting prospective longitudinal studies of DSM-IV personality disorder symptomatology in young adults who have not yet developed a clinically significant psychopathology but are presumably at risk for doing so. Trull et al. identified from a sample of 1,700 college students persons who presented with a sufficient number of borderline personality traits to consider them to represent premorbid cases. “These initial studies . . . mark an important step in identifying young adults with significant levels of borderline features who may go on to experience significant dysfunction in later years” (Trull et al., 1997, p. 308). Lenzenweger et al. likewise identified 708 college students from a sample 1,646 who provided sufficiently elevated scores on a measure of personality disorder symptomatology to consider them to be at risk for future mental disorders. “Clearly, the prospective study of these particular subjects, currently under way through the Longitudinal Study of Personality Disorders, will shed light on their long-term social and occupational functioning and their mental health” (Lenzenweger et al., 1997, p. 350).
Ideally, the personality dispositions studied in adulthood would have conceptually meaningful and empirically valid relationships to the behavior patterns and temperaments that are of interest in current developmental research. We referred to some of this research in our discussion of individual personality disorders (e.g., ASPD, AVPD, and DPD). For example, there has been substantial research on the contributions of sexual and psychological abuse to the etiology of BPD (Zanarini, 2000). Linehan (1993) has hypothesized that BPD is the result of a heritable temperament of emotional instability interacting with a severely invalidating (e.g., abusive) environment. However, the broad BPD diagnostic category may not capture well the specific traits that are especially vulnerable or responsive to abusive experiences. Progress in the understanding of the development of BPD might be obtained by an integration of BPD research with existing developmental studies on the interaction between parenting, temperament, and attachment (Bartholomew et al., 2001).
Research has indicated that much of the phenomenology of BPD can be understood as extreme variants of a general domain of personality functioning described as neuroticism or negative affectivity (Trull, 1992; Trull et al., 1998). Neuroticism is a domain of personality functioning along which all persons vary, including persons diagnosed with a personality disorder (Widiger & Costa, 1994), and much of the BPD symptomatologycanbeunderstoodasfacetsofneuroticism— specifically, angry hostility, vulnerability, impulsivity, anxiousness, depression, and impulsivity (Clarkin, Hull, Cantor, & Sanderson, 1993). Persons who are the very highest levels of angry hostility, vulnerability, impulsivity, anxiousness, and depression would be diagnosed with BPD. Although they are generally critical of this conceptualization of BPD, Morey and Zanarini (2000) did report obtaining better temporal stability over a 4-year period for neuroticism in comparison to the symptomatology of BPD. They suggested that BPD is perhaps “a disorder that waxes and wanes in severity over time, whereas neuroticism reflects a putatively stable trait configuration” (Morey & Zanarini, 2000, p. 737). “From this perspective, [neuroticism] could indicate a temperamental vulnerability to a disorder that is then triggered by developmental events (such as childhood neglect or abuse), resulting in functional levels that may be quite variable in response to situational elements even while the underlying traits remain relatively stable” (Morey & Zanarini, 2000, p. 737).
Biological Mechanisms of Maladaptive Personality Traits
We have left the decade of the brain to perhaps enter a decade of the brain disease (Hyman, 1998). The emphasis being given to neurophysiological models of psychopathology can be to the detriment of adequate attention to cognitive, interpersonal, and other psychosocial models of etiology and pathology (Gunderson, 2001; Miller, 1996; Widiger & Sankis, 2000). Nevertheless, there is also much that is neurophysiological in psychopathology and the progress that has been made in understanding biogenetic and neurophysiological etiologies and pathologies has been remarkable (Kandel, 1998). Regrettably, there has been comparably little progress in understanding the neurophysiology of most of the personality disorders.
Biogenetic and heritability research has been confined largely to ASPD, BPD, and STPD, with very little research specific to the narcissistic, obsessive-compulsive and other personality disorders (McGuffin & Thapar, 1992; Nigg & Goldsmith, 1992). On the other hand, there has been a considerable amount of biogenetic and heritability research on general personality functioning (Plomin & Caspi, 1999). Progress in understanding the biogenetics of the DSM-IV personality disorders might be obtained through a consideration of the biogenetic research of general personality functioning—as we suggested previously in our discussion of some of the individual personality disorders (e.g., AVPD, DPD, and HPD).
An important area of future research is the clarification of the physiological substrates of maladaptive personality traits (Cloninger, 1998; Depue & Lenzenweger, 2001). For example, clinical studies have suggested that low serotonergic (5-hydroxytryptamine or 5HT) activity might be related to angry, hostile, and aggressive behavior. This research has included personality disordered populations (e.g., antisocial and borderline) but “one of the most remarkable aspects of this literature is the general consistency of these findings across different study samples and using various assessments of 5HT function” (Coccaro, 1998, p. 2). In other words, the 5HT findings have not been specific to any particular mental disorder; rather, they are associated instead with more fundamental dimensions of impulsivity and aggression that cut across diagnostic categories.
The anatomy and physiology of humans is quite similar to that of nonhuman animals, and research on the neurobiology of animal behavior can contribute to an understanding of the neurophysiology of human personality functioning. For example, the personality domain of extraversion (positive emotionality) is quite analogous to the search, foraging, and approach system studied in various animal species, at times more globally referred to as a behavioral facilitation system (BFS). Depue (1996) and his colleagues are exploring the neurobiology of the personality domains of positive affectivity (extraversion), negative affectivity (neuroticism), and constraint (conscientiousness) through pharmacological challenge studies.
“One of the more exciting directions for genetic research on personality involves the use of molecular genetic techniques to identify some of the specific genes responsible for genetic influence on personality” (Plomin & Caspi, 1999, p. 261). This research may ultimately lead to an understanding of the causal pathways from cells to social systems that will elucidate how genes affect the development of personality disorders (Hyman, 1998). Support for hypotheses concerning domains of personality functioning that are hypothesized to underlie the DSM-IV personality disorders have been obtained (e.g., Osher, Hamer, & Benjamin, 2000). For example, individuals with the long-repeat DRD4 allele are thought to be dopamine deficient and to seek novelty to increase dopamine release (Cloninger, 1998). However, failures to replicate these findings have also occurred (e.g., Hamer, Greenberg, Sabol, & Murphy, 1999; Herbst, Zonderman, McCrae, & Costa, 2000). One possible reason for replication failures is that the effect sizes for broad personality dispositions provided by single genes is quite small, but other methodological concerns need to be addressed as well (Ordway, 2000; Hamer et al., 1999; Plomin & Caspi, 1999).
Integration With General Models of Personality Functioning
It is apparent from our discussion of developmental and biogenetic research that we feel that progress in the understanding of the DSM-IV personality disorders will be obtained by an integration of the APA (2000) personality disorders with our current understanding of general personality functioning (Trull, 2000; Widiger & Costa, 1994). Much of what we know about normal personality functioning should provide a strong empirical, scientific basis for what could be known about abnormal personality functioning.
A variety of studies and methodologies have raised compelling concerns regarding the validity of the DSM-IV categorical model of personality disorder, and the existing research suggests that the maladaptive personality traits that constitute the DSM-IV personality disorders might be better understood as maladaptive variants of common personality traits (Clark et al., 1997; Livesley, 1998;Trull, 2000;Widiger, 1993). Alternative dimensional models for the personality disorders have been proposed, including the 15-factor model of Clark (1993), the interpersonal circumplex (Wiggins & Pincus, 1989), the seven-factor model of Cloninger (1998), the 18-factor model of Livesley (1998), and the five-factor model (Widiger & Costa, 1994).
The five-factor model (FFM) of personality was derived originally from studies of the English language to identify the domains of personality functioning most important in describing the personality traits of oneself and other persons. This lexical research has emphasized five broad domains of personality, identified as extraversion (surgency or positive affectivity), agreeableness, conscientiousness (or constraint), neuroticism (negative affectivity), and openness (intellect or unconventionality; John & Srivastava, 1999). Each of these five domains can be further differentiated into underlying facets or components. Costa and McCrae (1992) have proposed six facets within each domain. For example, they suggest that the domain of agreeableness (vs. antagonism) can be usefully differentiated into more specific facets of trust (vs. mistrust, skepticism), straightforwardness (vs. deception, manipulation), altruism (vs. egocentrism, exploitation), compliance (vs. oppositionalism, aggression), modesty (vs. arrogance), and tendermindedness (vs. toughmindedness, callousness). Table 6.4 provides an abbreviated description of the 30 facets of the FFM.
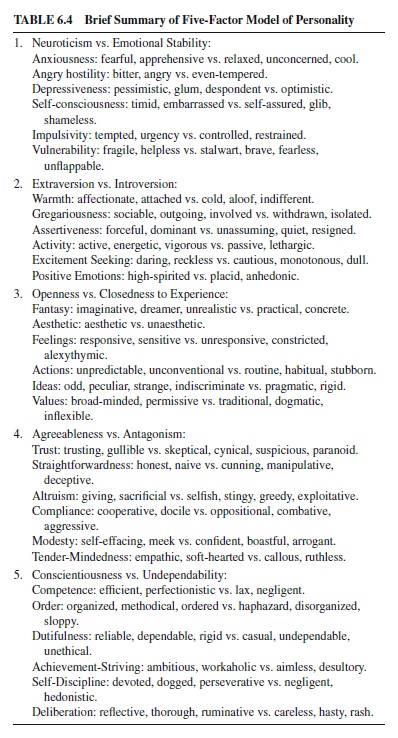
Empirical support for the construct validity of the FFM is extensive both at the domain and at the facet levels, including convergent and discriminant validation across self, peer, and spouse ratings, temporal stability, cross-cultural replication, and heritability (John & Srivastava, 1999; McCrae & Costa, 1999). The FFM has been used successfully as a model for integrating a broad and diverse array of personality research in such fields as industrial and organizational psychology and behavioral medicine. There does appear to be sufficient empirical support for the FFM to consider it for use as a possible dimensional model of personality disorder (Widiger & Costa, 1994).
Widiger, Trull, Clarkin, Sanderson, and Costa (1994) indicated how each of the DSM-III-R personality disorders could be understood in terms of the 30 facets of the FFM identified by Costa and McCrae (1992). These descriptions were updated for DSM-IV byTrull and Widiger (1997), and they informed some of our earlier discussions of individual personality disorders. For example, the normal domain of conscientiousness concerns a person’s degree of organization, persistence, order, and achievement orientation (Costa & McCrae, 1992). Conscientious persons tend to be organized, reliable, hard-working, self-disciplined, businesslike, and punctual. Persons who are overly conscientious will be excessively devoted to work, perfectionistic, and preoccupied with organization, rules, and details, resembling quite closely OCPD. AVPD is likewise readily understood as being simply maladaptively extreme variants of self-consciousness, anxiousness, and vulnerability facets of neuroticism, coupled with facets of introversion (Trull, 1992).
Wiggins and Pincus (1989) were the first to provide published data concerned with the relationship of the FFM to the APA (1980, 1987) personality disorder symptomatology. Since that original effort, more than 50 additional published studies have indicated a close relationship between the FFM and personality disorder symptomatology (Widiger & Costa, 2002). These studies, using a variety of measures and populations, have supported the hypothesis that each of the DSM-IV personality disorders could be readily understood as maladaptive variants of the personality traits included within the FFM (e.g., Ball, Tennen, Poling, Kranlem, & Rousanville, 1997; O’Connor & Dyce, 1998; Trull, 1992; Trull, Widiger, & Burr, 2001). The future of FFM personality disorder research will include a reproduction of the theoretical, nomological network surrounding the DSM-IV personality disorders, indicating how the etiology, pathology, and treatment of personality disorders can be best understood when the personality disorders are conceptualized as maladaptive variants of common personality traits.
Bibliography:
- Acklin, M. V. (1999). Behavioral science foundations of the Rorschach test: Research and clinical applications. Assessment, 6, 319–324.
- Adams, H. E., Bernat, J. A., & Luscher, K. A. (2001). Borderline personality disorder: An overview. In P. B. Sutker & H. E. Adams (Eds.), Comprehensive handbook of psychopathology (3rd ed., pp. 491–508). New York: Plenum.
- Adler, D. A., Drake, R. E., & Teague, G. B. (1990). Clinicians’practices in personality assessment: Does gender influence the use of DSM-III Axis II? Comprehensive Psychiatry, 31, 125–133.
- Alarcon, R. D. (1996). Personality disorders and culture in DSM-IV: A critique. Journal of Personality Disorders, 10, 260–270.
- Alarcon, R. D., & Foulks, E. F. (1996). Cultural factors and personality disorders. In T. A.Widiger, A. J. Frances, H. A. Pincus, R. Ross, M. B. First, & W. Davis (Eds.), DSM-IV Sourcebook (Vol. 3, pp. 975–982). Washington, DC: American Psychiatric Association.
- (1980).Diagnosticandstatistical manual of mental disorders (3rd ed.). Washington, DC: Author.
- American Psychiatric Association. (1987). Diagnostic and statistical manual of mental disorders (3rd ed., Rev. ed.). Washington, DC: Author.
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author.
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text revision). Washington, DC: Author.
- Archer, R. (1999). Some observations on the debate currently surrounding the Rorschach. Assessment, 6, 309–311.
- Ball, S. A., Tennen, H., Poling, J. C., Kranler, H. R., & Rousanville, B. J. (1997). Personality, temperament, and character dimensions in substance abusers. Journal of Abnormal Psychology, 106, 545–553.
- Bartholomew, K., Kwong, M. J., & Hart, S. D. (2001). Attachment. In W. J. Livesley (Ed.), Handbook of personality (pp. 196–230). New York: Guilford.
- Baumeister, R. F., Smart, L., & Boden, J. M. (1996). Relation of threatened egoism to violence and aggression: The dark side of high self-esteem. Psychological Review, 103, 5–33.
- Beck, A. T., Freeman, A., & Associates. (1990). Cognitive therapy of personality disorders. New York: Guilford.
- Bender, D. S., Dolan, R. T., Skodol, A. E., Sanislow, C. A., Dyck, R., McGlashan, T. H., Shea, M. T., Zanarini, M. C., Oldham, J. M., & Gunderson, J. G. (2001). Treatment utilization by patients with personality disorders. American Journal of Psychiatry, 158, 295–302.
- Bernstein, D. P., Cohen, P., Velez, C. N., Schwab-Stone, M., Siever, L., & Shinsato, L. (1993). Prevalence and stability of the DSMIII-R personality disorders in a community-based survey of adolescents. American Journal of Psychiatry, 150, 1237–1243.
- Bernstein, D. P., Kasapis, C., Bergman, A., Weld, E., Mitropoulou, V., Horvath, T., Klar, H., Silverman, J., & Siever, L. J. (1997). Assessing Axis II disorders by informant interview. Journal of Personality Disorders, 11, 158–167.
- Bernstein, D. P., & Travaglini, L. (1999). Schizoid and avoidant personality disorders. In T. Millon, P. H. Blaney, & R. D. Davis (Eds.), Oxford textbook of psychopathology (pp. 523–534). New York: Oxford University Press.
- Black, D. W., Noyes, R., Pfohl, B., Goldstein, R. B., & Blum, N. (1993). Personality disorder in obsessive-compulsive volunteers, well comparison subjects, and their first degree relatives. American Journal of Psychiatry, 150, 1226–1232.
- Blais, M. A., Hilsenroth, M. J., & Fowler, J. C. (1998). Rorschach correlates of the DSM-IV histrionic personality. Journal of Personality Assessment, 70, 355–364.
- Blashfield, R. K., Blum, N., & Pfohl, B. (1992). The effects of changing Axis II diagnostic criteria. Comprehensive Psychiatry, 33, 245–252.
- Blashfield, R. K., & Herkov, M. J. (1996). Investigating clinician adherence to diagnosis by criteria: A replication of Morey and Ochoa (1989). Journal of Personality Disorders, 10, 219– 228.
- Blatt, S. J., Cornell, C. E., & Eshkol, E. (1993). Personality style, differential vulnerability, and clinical course in immunological and cardiovascular disease. Clinical Psychology Review, 13, 421–450.
- Blatt, S. J., & Zuroff, D. (1992). Interpersonal relatedness and selfdefinition: Two prototypes for depression. Clinical Psychology Review, 12, 527–562.
- Bornstein, R. F. (1992). The dependent personality: Developmental, social, and clinical perspectives. Psychological Bulletin, 112, 3–23.
- Bornstein, R. F. (1995). Sex differences in objective and projective dependency tests: A meta-analytic review. Assessment, 2, 319–331.
- Bornstein, R. F. (1999). Dependent and histrionic personality disorders. In T. Millon, P. Blaney, & R. Davis (Eds.), Oxford textbook of psychopathology (pp. 535–554). Oxford, England: Oxford University Press.
- Bushman, B. J., & Baumeister, R. F. (1998). Threatened egotism, narcissism, self-esteem, and direct and displaced aggression: Does self-love or self-hate lead to violence? Journal of Personality and Social Psychology, 75, 219–229.
- Caspi, A. (1998). Personality development across the life course. In W. Damon & N. Eisenberg (Eds.), Handbook of child psychology: Vol. 3. Social, emotional, and personality development (pp. 311–388). New York: Wiley.
- Clark, L. A. (1993). Manual for the Schedule for Nonadaptive and Adaptive Personality. Minneapolis: University of Minnesota Press.
- Clark, L. A., & Harrison, J. A. (2001). Assessment instruments. In W. J. Livesley (Ed.), Handbook of personality disorders (pp. 277–306). New York: Guilford.
- Clark, L. A., Livesley, W. J., & Morey, L. (1997). Personality disorder assessment: The challenge of construct validity. Journal of Personality Disorders, 11, 205–231.
- Clark, L.A., Watson, D., & Reynolds, S. (1995). Diagnosis and classification of psychopathology: Challenges to the current system andfuturedirections.AnnualReviewofPsychology,46,121–153.
- Clarkin, J. F., Hull, J. W., Cantor, J., & Sanderson, C. (1993). Borderline personality disorder and personality traits: A comparison of SCID-II BPD and NEO-PI. Psychological Assessment, 5, 472–476.
- Cloninger, C. R. (1998). The genetics and psychobiology of the seven-factor model of personality. In K. R. Silk (Ed.), Biology of personality disorders (pp. 63–92). Washington, DC: American Psychiatric Press.
- Coccaro, E. F. (1998). Neurotransmitter function in personality disorders. In K. Silk (Ed.), Biology of personality disorders (pp. 1–25). Washington, DC: American Psychiatric Press.
- Cooper, A. M., & Ronningstam, E. (1992). Narcissistic personality disorder. In A. Tasman & M. B. Riba (Eds.), Review of psychiatry (Vol. 11, pp. 80–97). Washington, DC: American Psychiatric Press.
- Corbitt, E. M., & Widiger, T. A. (1995). Sex differences among the personality disorders: An exploration of the data. Clinical Psychology: Science and Practice, 2, 225–238.
- Costa, P. T., Jr., & McCrae, R. R. (1992). Revised NEO-Personality Inventory (NEO-PI-R) and NEO Five Factor Inventory (FFI) manual. Odessa, FL: Psychological Assessment Resources.
- Coyne, J. C., & Whiffen, V. E. (1995). Issues in personality as diathesis for depression: The case of sociotropy-dependency and autonomy-self-criticism. Psychological Bulletin, 118, 358–378.
- Daley,S.E.,Burge,D.,&Hammen,C.(2000).Borderlinepersonality disorder symptoms as predictors of 4-year romantic relationship dysfunction in young women: Addressing issues of specificity. Journal ofAbnormal Psychology, 109, 451–460.
- Depue, R. A. (1996). A neurobiological framework for the structure of personality and emotion: Implications for personality disorders. In J. F. Clarkin & M. F. Lenzenweger (Eds.), Major theories of personality disorder (pp. 347–390). New York:
- Depue, R. A., & Lenzenweger, M. F. (2001). A neurobehavioral dimensional model. In W. J. Livesley (Ed.), Handbook of personality disorders (pp. 136–176). New York: Guilford.
- Dodge, K. A., & Schwartz, D. (1997). Social information processing mechanisms in aggressive behavior. In D. M. Stoff, J. Breiling, & J. D. Maser (Eds.), Handbook of antisocial behavior (pp. 171– 180). New York: Wiley.
- Dolan-Sewell, R. G., Krueger, R. F., & Shea, M. T. (2001). Cooccurrence with syndrome disorders. In W. J. Livesley (Ed.), Handbook of personality disorders (pp. 84–104). New York: Guilford.
- Farrington, D. P. (1997). Acritical analysis of research on the development of antisocial behavior from birth to adulthood. In D. M. Stoff, J. Breiling, & J. D. Maser (Eds.), Handbook of antisocial behavior (pp. 234–241). New York: Wiley.
- Foulks, E. F. (1996). Culture and personality disorders. In J. E. Mezzich, A. Kleinman, H. Fabrega, & D. L. Parron (Eds.), Culture and psychiatric diagnosis. A DSM-IV perspective (pp. 243– 252). Washington, DC: American Psychiatric Press.
- Frances, A. J. (1980). The DSM-III personality disorders section: A commentary. American Journal of Psychiatry, 137, 1050–1054.
- Fulton, M., & Winokur, G. (1993). A comparative study of paranoid and schizoid personality disorders. American Journal of Psychiatry, 150, 1363–1367.
- Garb, H. N. (1997). Race bias, social class bias, and gender bias in clinical judgment. Clinical Psychology: Science and Practice, 4, 99–120.
- Garb, H. N. (1999). Call for a moratorium on the use of the Rorschach inkblot test in clinical and forensic settings. Assessment, 6, 313–315.
- Gunderson, J. G. (1992). Diagnostic controversies. In A. Tasman & M. B. Riba (Eds.), Review of psychiatry (Vol. 11, pp. 9–24). Washington, DC: American Psychiatric Press.
- Gunderson, J. G. (2001). Borderline personality disorder. A clinical guide. Washington, DC: American Psychiatric Press.
- Hamer, D. H., Greenberg, B. D., Sabol, S. Z., & Murphy, D. L. (1999). Role of the serotonin transporter gene in temperament and character. Journal of Personality Disorders, 13, 312–328.
- Hammen, C. L., Burge, D., Daley, S. E., Davila, J., Paley, B., & Rudolph, K. D. (1995). Interpersonal attachment cognitions and predictions of symptomatic responses to interpersonal stress. Journal of Abnormal Psychology, 104, 436–443.
- Hare, R. D. (1991). The Revised Psychopathy Checklist. Toronto, Ontario, Canada: Multi-Health Systems.
- Harkness, A. R., & Lilienfeld, S. O. (1997). Individual differences science for treatment planning: Personality traits. Psychological Assessment, 9, 349–360.
- Hart, S. D., & Hare, R. D. (1997). Psychopathy: Assessment and association with criminal conduct. In D. M. Stoff, J. Breiling, & J. D. Maser (Eds.), Handbook of antisocial behavior (pp. 22–35). New York: Wiley.
- Herbst, J. H., Zonderman, A. B., McCrae, R. R., & Costa, P. T. (2000). Do the dimensions of the Temperament and Character Inventory map a simple genetic architecture? Evidence from molecular genetics and factor analysis. American Journal of Psychiatry, 157, 1285–1290.
- Herkov, M. J., & Blashfield, R. K. (1995). Clinicians’ diagnoses of personality disorder: Evidence of a hierarchical structure. Journal of Personality Assessment, 65, 313–321.
- Hilsenroth, M. J., Handler, L., & Blais, M. A. (1996). Assessment of narcissistic personality disorder: A multi-method review. Clinical Psychology Review, 16, 655–683.
- Hinshaw, S. P. (1994). Conduct disorder in childhood: Conceptualization, diagnosis, comorbidity, and risk status for antisocial functioning in adulthood. In D. C. Fowles, P. B. Sutker, & S. H. Goodman (Eds.), Progress in experimental personality and psychopathology research (Vol. 15, pp. 3–44). New York: Springer.
- Horowitz, M. J. (1991). Hysterical personality style and the histrionic personality disorder. Northvale, NJ: Jason Aronson.
- Hyler, S. E. (1994). Personality Diagnostic Questionnaire-4 (PDQ-4) [Unpublished test]. New York: New York State Psychiatric Institute.
- Hyman, S. E. (1998). NIMH during the tenure of Director Steven E. Hyman, M.D. (1996-present): The now and future of NIMH. American Journal of Psychiatry, 155(Suppl.), 36–40.
- Jang, K. L., McCrae, R. R., Angleitner, A., Riemann, R., & Livesley, W. J. (1998). Heritability of facet-level traits in a cross-cultural twin sample: Support for a hierarchical model of personality. Journal of Personality and Social Psychology, 74, 1556–1565.
- Jang, K. L., & Vernon, P. A. (2001). Genetics. In W. J. Livesley (Ed.), Handbook of personality disorders (pp. 177–195). New York: Guilford.
- John, O. P., & Srivastava, S. (1999). The Big Five trait taxonomy: History, measurement, and theoretical perspectives. In L. A. Pervin & O. P. John (Eds.), Handbook of personality. Theory and research (2nd ed., pp. 102–138). New York: Guilford.
- Johnson, F. F. (1993). Dependency and Japanese socialization. New York: New York University Press.
- Johnson, J. G., Cohen, P., Brown, J., Smailes, E. M., & Bernstein, D. P. (1999). Childhood maltreatment increases risk for personality disorders during early adulthood. American Journal of Psychiatry, 56, 600–606.
- Kandel, E. R. (1998). A new intellectual framework for psychiatry. American Journal of Psychiatry, 155, 457–469.
- Kaye, A. L., & Shea, M. T. (2000). Personality disorders, personality traits, and defense mechanisms measures. In H. A. Pincus, A. J. Rush, M. B. First, & L. E. McQueen (Eds.), Handbook of psychiatric measures (pp. 713–750). Washington, DC: American Psychiatric Association.
- Kessler, R. C. (1999). The World Health Organization International Consortium in psychiatric epidemiology. Initial work and future directions: The NAPE lecture. Acta Psychiatrica Scandinavica, 99, 2–9.
- Klein, D. F. (1999). Harmful dysfunction, disorder, disease, illness, and evolution. Journal of Abnormal Psychology, 108, 421–429.
- Kochanska, G. (1991). Socialization and temperament in the development of guilt and conscience. Child Development, 62, 1379– 1392.
- Koenigsberg, H. W., Kaplan, R. D., Gilmore, M. M., & Cooper, A. M. (1985). The relationship between syndrome and personality disorder in DSM-III: Experience with 2,462 patients. American Journal of Psychiatry, 142, 207–212.
- Lenzenweger, M. F., Loranger, A. W., Korfine, L., & Neff, C. (1997). Detecting personality disorders in a nonclinical population. Archives of General Psychiatry, 54, 345–351.
- Linehan, M. M. (1993). Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press.
- Livesley, W. J. (1998). Suggestions for a framework for an empirically based classification of personality disorder. Canadian Journal of Psychiatry, 43, 137–147.
- Livesley, W. J., Jang, K. L., & Vernon, P. A. (1998). Phenotypic and genetic structure of traits delineating personality disorder. Archives of General Psychiatry, 55, 941–948.
- Loranger,A.W.,Sartorius,N.,Andreoli,A.,Berger,P.,Buchheim,P., Channabasavanna, S. M., et al. (1994). The International Personality Disorder Examination. The World Health Organization/ Alcohol, DrugAbuse, and Mental HealthAdministration international pilot study of personality disorders. Archives of General Psychiatry, 51, 215–224.
- Lyons, M. J. (1995). Epidemiology of personality disorders. In M. T. Tsuang, M. Tohen, & G. E. P. Zahner (Eds.), Textbook in psychiatric epidemiology. New York: Wiley-Liss.
- Maier, W., Lichtermann, D., Klinger, T., & Heun, R. (1992). Prevalences of personality disorders (DSM-III-R) in the community. Journal of Personality Disorders, 6, 187–196.
- Mattia, J. I., & Zimmerman, M. (2001). Epidemiology. In W. J. Livesley (Ed.), Handbook of personality disorders (pp. 107– 123). New York: Guilford.
- McCann, J. T. (1999). Obsessive-compulsive and negativistic personality disorders. In T. Millon, P. Blaney, & R. Davis (Eds.), Oxford textbook of psychopathology (pp. 585–604). Oxford, England: Oxford University Press.
- McCrae, R. R., & Costa, P. T. (1999). A five-factor theory of personality. In L. A. Pervin & O. P. John (Eds.), Handbook of personality (2nd ed., pp. 139–153). New York: Guilford.
- McGuffin, P., & Thapar, A. (1992). The genetics of personality disorder. British Journal of Psychiatry, 160, 12–23.
- Miller, G. A. (1996). How we think about cognition, emotion, and biology in psychopathology. Psychophysiology, 33, 615–628.
- Miller, M. B., Useda, J. D., Trull, T. J., Burr, R. M., & Minks-Brown, (2001). Paranoid, schizoid, and schizotypal personality disorders. In P. B. Sutker & H. E. Adams (Eds.), Comprehensive handbook of psychopathology (3rd ed., pp. 535–558). NewYork: Plenum.
- Millon, T., Davis, R. D., Millon, C. M., Wenger, A. W., Van Zuilen, M. H., Fuchs, M., & Millon, R. B. (1996). Disorders of personality: DSM-IV and beyond. New York: Wiley.
- Millon, T., & Frances, A. J. (1987). Editorial. Journal of Personality Disorders, 1, i-iii.
- Modestin, J., Oberson, B., & Erni, T. (1998). Possible antecedents of DSM-III-R personality disorders. Acta Psychiatrica Scandinavica, 97, 260–266.
- Morey, L. C. (1988). Personality disorders in DSM-III and DSM-III-R: Convergence, coverage, and internal consistency. American Journal of Psychiatry, 145, 573–577.
- Morey, L. C., & Ochoa, E. (1989). An investigation of adherence to diagnostic criteria: Clinical diagnosis of the DSM-III personality disorders. Journal of Personality Disorders, 3, 180–192.
- Morey, L. C, & Zanarini, M. C. (2000). Borderline personality: Traits and disorder. Journal of Abnormal Psychology, 109, 733– 737.
- Nigg, J. T., & Goldsmith, H. H. (1994). Genetics of personality disorders: Perspectives from personality and psychopathology research. Psychological Bulletin, 115, 346–380.
- Norden, K. A., Klein, D. N., Donaldson, S. K., Pepper, C. M., & Klein, L. M. (1995). Reports of the early home environment in DSM-III-R personality disorders. Journal of Personality Disorders, 9, 213–223.
- O’Connor, B. P., & Dyce, J. A. (1998). A test of models of personality disorder configuration. Journal of Abnormal Psychology, 107, 3–16.
- Oldham, J. M., & Frosch, W. A. (1991). Compulsive personality disorder. In R. Michels (Ed.), Psychiatry (Vol. 1, pp. 1–8). Philadelphia: Lippincott.
- Oltmanns, T. F., Turkheimer, E., & Strauss, M. E. (1998). Peer assessment of personality traits and pathology. Assessment, 5, 53–65.
- O’Neill, F. A., & Kendler, K. S. (1998). Longitudinal study of interpersonal dependency in female twins. British Journal of Psychiatry, 172, 154–158.
- Ordway, G. A. (2000). Searching for the chicken’s egg in transporter gene polymorphism. Archives of General Psychiatry, 57, 739– 740.
- Ornduff, S. R. (2000). Childhood maltreatment and malevolence: Quantitative research findings. Clinical Psychology Review, 20, 991–1018.
- Osher, Y., Hamer, D., & Benjamin, J. (2000). Association and linkage of anxiety-related traits with a functional polymorphism of the serotonin transporter gene regulatory region in Israeli sibling pairs. Molecular Psychiatry, 5, 216–219.
- Padilla, A. M. (1995). Hispanic psychology: Critical issues in theory and research. Newbury Park, CA: Sage.
- Paris, J. (2001). Psychosocial adversity. In W. J. Livesley (Ed.), Handbook of personality disorders (pp. 231–241). New York: Guilford.
- Patrick, C. J. (1994). Emotion and psychopathy: Startling new insights. Psychophysiology, 31, 415–428.
- Perry, J. C., Banon, E., & Ianni, F. (1999). Effectiveness of psychotherapy for personality disorders. American Journal of Psychiatry, 156, 1312–1321.
- Plomin, R., & Caspi, A. (1999). Behavioral genetics and personality. In L. Pervin & O. John (Eds.), Handbook of personality (2nd ed., pp. 251–276). New York: Guilford.
- Raskin, R., Novacek, J., & Hogan, R. (1991). Narcissistic selfesteem management. Journal of Personality and Social Psychology, 60, 911–918.
- Rhodewalt, F., Madrian, J. C., & Cheney, S. (1998). Narcissism, self-knowledge, organization, and emotional reactivity: The effect of daily experience on self-esteem and affect. Personality and Social Psychology Bulletin, 24, 75–87.
- Riso, L. P., Klein, D. N., Anderson, R. L., Ouimette, P. C., & Lizardi, H. (1994). Concordance between patients and informants on the Personality Disorder Examination. American Journal of Psychiatry, 151, 568–573.
- Robins, C. J., Hayes, A. H., Block, P., Kramer, R. J., & Villena, M. (1995). Interpersonal and achievement concerns and the depressive vulnerability and symptom specificity hypothesis: A prospective study. Cognitive Therapy and Research, 19, 1–20.
- Robins, L. N., & Regier, D. A. (Eds.). (1991). Psychiatric disorders in America. New York : Free Press.
- Robins,L.N.,Tipp,J.,&Przybeck,T.(1991).Antisocialpersonality. In L. N. Robins & D. A. Regier (Eds.), Psychiatric disorders in America. The epidemiologic catchment area study (pp. 258–290). NewYork: Free Press.
- Rogers, R. (1995). Diagnostic and structured interviewing. A handbook for psychologists. Odessa, FL: Psychological Assessment Resources.
- Rogler, L. H. (1996). Framing research on culture in psychiatric diagnosis: The case of the DSM-IV. Psychiatry, 59, 145–155.
- Rothbart, M. K., & Ahadi, S. A. (1994). Temperament and the development of personality. Journal of Abnormal Psychology, 103, 55–66.
- Samuels, J. F., Nestadt, G., Romanoski, A. J., Folstein, M. F., & McHugh, P. R. (1994). DSM-III personality disorders in the community. American Journal of Psychiatry, 151, 1055– 1062.
- Sanderson, C., & Clarkin, J. F. (1994). Use of the NEO-PI personality dimensions in differential treatment planning. In P. T. Costa & T. A. Widiger (Eds.), Personality disorders and the five-factor model of personality (pp. 219–235). Washington, DC: American Psychological Association.
- Sanislow, C. A., & McGlashan, T. H. (1998). Treatment outcome of personality disorders. Canadian Journal of Psychiatry, 43, 237–250.
- Santor, D. A., & Zuroff, D. C. (1997). Interpersonal responses to threats of status and interpersonal relatedness: Effects of dependency and self-criticism. British Journal of Clinical Psychology, 36, 521–541.
- Sher, K. J., & Trull, T. J. (1996). Methodological issues in psychopathology research. Annual Review of Psychology, 47, 371–400.
- Siever, L. J. (1992). Schizophrenia spectrum disorders. In A. Tasman & M. B. Riba (Eds.), Review of psychiatry (Vol. 11, pp. 25–42). Washington, DC: American Psychiatric Press.
- Siever, L. J., & Davis, K. L. (1991). A psychobiological perspective on the personality disorders. American Journal of Psychiatry, 148, 1647–1658.
- Silk, K. S., Lee, S., Hill, E. M., & Lohr, N. E. (1995). Borderline personality disorder symptoms and severity of sexual abuse. American Journal of Psychiatry, 152, 1059–1064.
- Skodol, A. E., Oldham, J. M., Rosnick, L., Kellman, H. D., & Hyler, S. E. (1991). Diagnosis of DSM-III-R personality disorders: A comparison of two structured interviews. International Journal of Methods in Psychiatric Research, 1, 13–26.
- Soloff, P. H., Siever, L., Cowdry, R., & Kocsis, J. H. (1994). Evaluation of pharmacologic treatment in personality disorders. In R. F. Prien & D. S. Robinson (Eds.), Clinical evaluation of psychotropic drugs: Principles and guidelines (pp. 651–673). New York: Raven.
- Spitzer, R. L., & Wakefield, J. C. (1999). The DSM-IV diagnostic criterion for clinical significance: Does it help solve the false positives problem? American Journal of Psychiatry, 156, 1856– 1864.
- Spitzer, R. L., Williams, J. B. W., & Skodol, A. E. (1980). DSM-III: The major achievements and an overview. American Journal of Psychiatry, 137, 151–164.
- Stoff, D. M., Breiling, J., & Maser, J. D. (Eds.). (1997). Handbook of antisocial behavior. New York: Wiley.
- Stone, M. H. (1993). Abnormalities of personality: Within and beyond the realm of treatment. New York: Norton.
- Stone, M. H. (2001). Natural history and long-term outcome. In W. J. Livesley (Ed.), Handbook of personality disorders (pp. 259–273). New York: Guilford.
- Sutker, P. B., & Allain, A. N. (2001). Antisocial personality disorder. In P. B. Sutker & H. E. Adams (Eds.), Comprehensive handbook of psychopathology (3rd ed., pp. 445–490). New York: Plenum.
- Thompson, S., & Zuroff, D. C. (1998). Dependent and self-critical mothers’ responses to adolescent autonomy and competence. Personality and Individual Differences, 24, 311–324.
- Tickle, J. F., Heatherton, T. F., & Wittenberg, L. G. (2001). Can personality change? In W. J. Livesley (Ed.), Handbook of personality disorders (pp. 242–258). New York: Guilford.
- Trull, T. J. (1992). DSM-III-R personality disorders and the fivefactor model of personality: An empirical comparison. Journal of Abnormal Psychology, 101, 553–560.
- Trull, T. J. (2000). Dimensional models of personality disorder. Current Opinion in Psychiatry, 13, 179–184.
- Trull, T. J., Sher, K. J., Minks-Brown, C., Durbin, J., & Burr, R. (2000). Borderline personality disorder and substance use disorders: A review and integration. Clinical Psychology Review, 20, 235–254.
- Trull, T. J., Useda, D., Conforti, K., & Doan, B.-T. (1997). Borderline personality disorder features in nonclinical young adults: 2. Two-year outcome. Journal of Abnormal Psychology, 106, 307–314.
- Trull, T. J., & Widiger, T. A. (1997). Structured Interview for the five-factor model of personality. Odessa, FL: Psychological Assessment Resources.
- Trull, T. J., Widiger, T. A., & Burr, R. (2001). Astructured interview for the assessment of the five-factor model of personality: 2. Facet-level relations to the Axis II personality disorders. Journal of Personality, 69, 175–198.
- Trull, T. J., Widiger, T. A., Useda, J. D., Holcomb, J., Doan, B.-T., Axelrod, S. R., Stern, B. L., & Gershuny, B. S. (1998). A structured interview for the assessment of the five-factor model of personality. Psychological Assessment, 10, 229–240.
- Wakefield, J. C. (1992). Disorder as harmful dysfunction: Aconceptual critique of DSM-III-R’s definition of mental disorder. Psychological Review, 99, 232–247.
- Weiner, I. B. (1999). What the Rorschach can do for you: Incremental validity in clinical applications. Assessment, 6, 327–338.
- Weissman, M. M. (1993). The epidemiology of personality disorders: A 1990 update. Journal of Personality Disorders, 7, 44– 62.
- Westen, D. (1997). Divergences between clinical and research methods for assessing personality disorders: Implications for research and the evolution of Axis II. American Journal of Psychiatry, 154, 895–903.
- Whaley, A. (1997). Ethnicity/race, paranoia, and psychiatric diagnosis: Clinician bias versus sociocultural differences. Journal of Psychopathology and Behavorial Assessment, 19, 1–20.
- Widiger, T. A. (1993). The DSM-III-R categorical personality disorder diagnoses: A critique and an alternative. Psychological Inquiry, 4, 75–90.
- Widiger, T. A. (1998). Sex biases in the diagnosis of personality disorders. Journal of Personality Disorders, 12, 95–118.
- Widiger, T. A. (2001). Official classification systems. In W. J. Livesley (Ed.), Handbook of personality disorders (pp. 60–83). New York: Guilford.
- Widiger, T. A. (2002). Personality disorders. In M. M. Antony & D. H. Barlow (Eds.), Handbook of assessment, treatment planning, and outcome (pp. 453–480). New York: Guilford.
- Widiger, T. A., & Bornstein, R. F. (2001). Histrionic, dependent, and narcissistic personality disorders. In P. B. Sutker & H. E. Adams (Eds.), Comprehensive handbook of psychopathology (3rd ed., pp. 509–531). New York: Plenum.
- Widiger, T. A., & Clark, L. A. (2000). Toward DSM-V and the classification of psychopathology. Psychological Bulletin, 126, 946–963.
- Widiger, T. A., & Coker, L. A. (2002). Assessing personality disorders. In J. N. Butcher (Ed.), Clinical personality assessment. Practical approaches (2nd ed., pp. 407–434). New York: Oxford University Press.
- Widiger, T. A., & Corbitt, E. (1994). Normal versus abnormal personality from the perspective of the In S. Strack & M. Lorr (Eds.), Differentiating normal and abnormal personality (pp. 158–175). New York: Springer.
- Widiger, T. A., & Costa, P. T. (1994). Personality and personality disorders. Journal of Abnormal Psychology, 103, 78–91.
- Widiger, T. A., & Costa, P. T. (in press). Five factor model personality disorder research. In P. T. Costa & T. A. Widiger (Eds.), Personality disorders and the five factor model of personality (2nd ed.). Washington, DC: American Psychological Association.
- Widiger, T., Frances, A., Spitzer, R., & Williams, J. (1988). The DSM-III-R personality disorders: An overview. American Journal of Psychiatry, 145, 786–795.
- Widiger, T. A., & Lynam, D. R. (1998). Psychopathy from the perspective of the five-factor model of personality. In T. Millon, E. Simonsen, & M. Birket-Smith (Eds.), Psychopathy: antisocial, criminal, and violent behaviors (pp. 171–187). New York: Guilford.
- Widiger, T. A., Mangine, S., Corbitt, E. M., Ellis, C. G., & Thomas, G. V. (1995). Personality Disorder Interview-IV: A semistructured interview for the assessment of personality disorders. Odessa, FL: Psychological Assessment Resources.
- Widiger, T. A., & Sankis, L. (2000). Adult psychopathology: Issues and controversies. Annual Review of Psychology, 51, 377–404.
- Widiger, T. A., & Spitzer, R. L. (1991). Sex bias in the diagnosis of personality disorders: Conceptual and methodological issues. Clinical Psychology Review, 11, 1–22.
- Widiger, T. A., Trull, T. J., Clarkin, J. F., Sanderson, C., & Costa, P. T., Jr. (1994). Adescription of the DSM-III-R and DSM-IV personality disorders with the five-factor model of personality. In P. T. Costa & T. A. Widiger (Eds.), Personality disorders and the five-factor model of personality (pp. 41–56). Washington, DC: American Psychological Association.
- Widiger, T. A., Verheul, R., & van den Brink, W. (1999). Personality and psychopathology. In L. Pervin & O. John (Eds.), Handbook of personality (2nd ed., pp. 347–366). New York: Guilford.
- Wiggins, J. S., & Pincus, A. (1989). Conceptions of personality disorder and dimensions of personality. Psychological Assessment, 1, 305–316.
- Wood, J. M., & Lilienfeld, S. O. (1999). The Rorschach inkblot test: A case of overstatement? Assessment, 6, 341–349.
- World Health Organization. (1992). The ICD-10 classification of mental and behavioural disorders. Clinical descriptions and diagnostic guidelines. Geneva, Switzerland: Author.
- Zanarini, M. C. (2000). Childhood experiences associated with the development of borderline personality disorder. Psychiatric Clinics of North America, 23, 89–101.
- Zimmerman, M. (1994). Diagnosing personality disorders: Areview of issues and research methods. Archives of General Psychiatry, 51, 225–245.
- Zimmerman, M., & Coryell, W. H. (1989). DSM-III personality disorder diagnoses in a nonpatient sample. Archives of General Psychiatry, 46, 682–689.
- Zimmerman, M., & Mattia, J. I. (1999a). Differences between clinical and research practices in diagnosing borderline personality disorder. American Journal of Psychiatry, 156, 1570–1574.
- Zimmerman, M., & Mattia, J. I. (1999b). Psychiatric diagnosis in clinical practice: Is comorbidity being missed? Comprehensive Psychiatry, 40, 182–191.




