View sample Sleep And Health Research Paper. Browse other research paper examples and check the list of research paper topics for more inspiration. If you need a religion research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our custom writing services for professional assistance. We offer high-quality assignments for reasonable rates.
1. Sleep Physiology
Sleep is a ubiquitous mammalian phenomenon which is associated with diminished responsiveness to external stimuli and a familiar and delightful sense of restoration under the circumstances of a normal night of sleep. The importance of sleep in daily living can easily be discerned when an individual has even a modest restriction in a normal night of sleep. This has been well documented to be associated with performance decrement and alterations in mood. The mysteries of sleep are many, and how it produces its restorative effects remain vague, but it is clear that it is at the core of mental and physical well being. Biological functioning cannot be thoroughly appreciated without integrating sleep and sleep biology into our understanding of waking biology. It is obvious now to the layman and professional sleep researcher both that sleeping behavior effects waking behavior, and waking behavior effects sleeping behavior.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
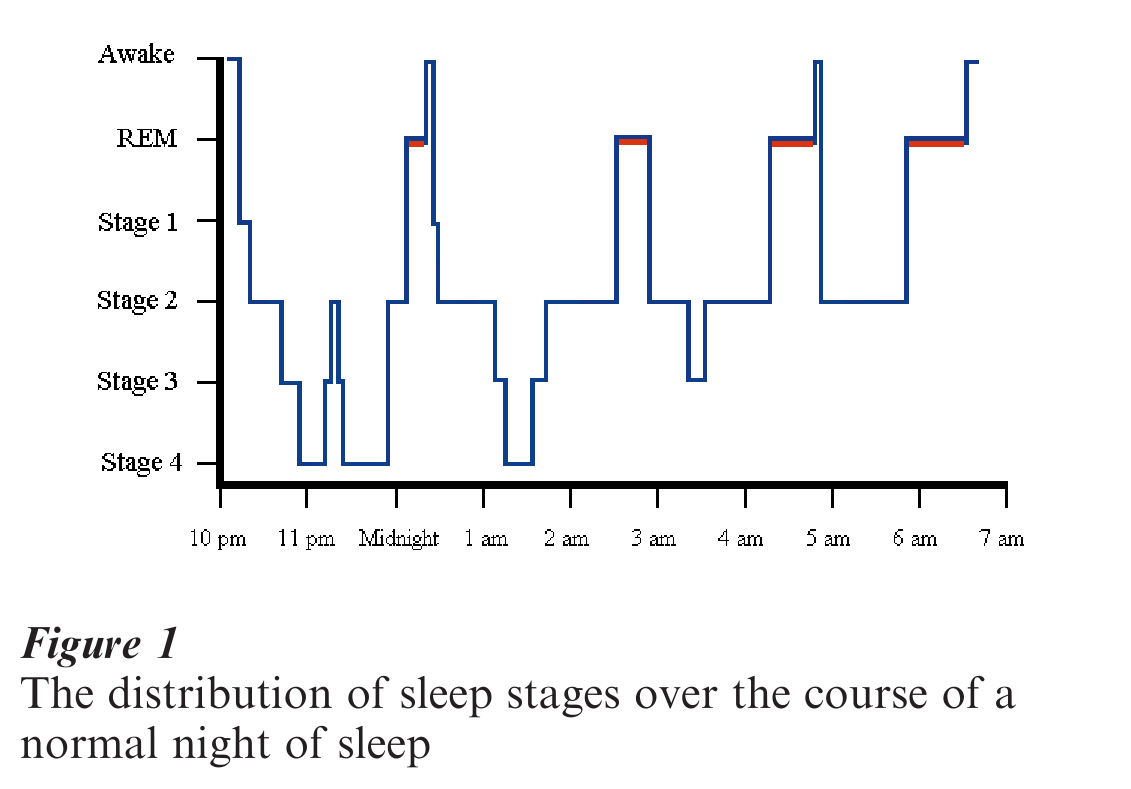
In the mid-1950s, some of the mysteries of sleep began to unravel by a series of discoveries by Nathaniel Kleitman, William Dement, and Eugene Aserinsky at the University of Chicago (Dement 1990). These individuals produced a series of studies which delineated the brain wave patterns associated with different stages of sleep, and the unique stage of sleep which was termed rapid eye movement (REM) sleep, shown to be associated with dreaming. These stages of sleep were determined by the concomitant recording of the electroencephalogram (EEG), electro-octulogram (EOG), and the electromyogram (EMG). The stages of sleep are characterized by a pattern of activity in each of these variables. Brain wave activity changes dramatically from waking to the deep stages of sleep (stages 3 and 4) with high voltage slow waves becoming increasingly dominant. These stages are distributed throughout the night in a well-defined pattern of activity associated with REM periods approximately every 90 minutes (Fig. 1). REM periods are interspersed with stages 2, 3, and 4 such that stages 3 and 4 are identified largely in the first third of the night, with relatively little noted in the last third of the night. REM sleep is accumulated with episodes occurring every 90 minutes as noted, but as the night progresses, the REM periods become progressively longer, thus producing very long REM periods in the last third of the sleeping interval. Thus, REM sleep is identified primarily in the last third of the night, with relatively little in the first third of the night (Carskadon and Dement 1994).
Of interest, is the fact that REM sleep is associated with some unique physiologic changes. Thermo-regulatory and respiratory functioning are markedly compromised during REM sleep. For example, the vasomotor mechanisms necessary to respond appropriately to increases and decreases in ambient temperature in order to maintain a normal core body temperature are suspended during REM sleep. This renders the mammalian organism poikilothermic, or cold blooded, during REM sleep. In addition, appropriate respiratory compensatory responses to both hypoxemia and hypercapnia are substantially blunted during REM sleep. These data combine to suggest that even under normal circumstances, REM sleep is a period of physiologic risk woven into the fabric of a normal night of sleep.
Other phenomena associated with REM sleep are of considerable interest. For example, it is known that REM sleep is associated with a skeletal muscle paralysis. This has been substantiated by the documentation of hyperpolarization of motor neurons during REM sleep in cats. In addition, REM sleep is generally associated with thematic dreaming, and it is felt that the inhibition of skeletal muscles prevents the ‘acting out’ of dreams. Also during each REM period penile tumescence occurs, resulting in a normal full erection in males (Carskaden and Dement 1994).
Non-REM (NREM) sleep, alternatively, is associated with a slowing of physiological processes to include heart rate, blood pressure, and general metabolic rate compared to the waking state. During the first episode of slow wave sleep (stages 3 and 4) there is a dramatic increase in the secretion of growth hormone. This has been shown to be specifically linked to the first episode of slow wave sleep, rather than a circadian phenomenon. No other hormone is quite so precisely identified with secretion during a specific stage of sleep.
2. Subjective Aspects Of Sleep
The quality of sleep, and the physiologic parameters which produce ‘good sleep’ or a feeling of restoration in the morning are not understood. Deprivation of REM sleep as opposed to non-REM sleep does not appear to differentially affect subsequent mood or performance. It is well established that older adults have characteristic alterations in their sleep patterns, i.e., a marked diminution in stages 3 and 4 sleep, which are quite characteristically associated with complaints of nonrestorative, or poor sleep. Determining the physiologic characteristics of the subjective elements of ‘good sleep’ is difficult in that it is well known that the subjective and physiologic aspects of sleep can be easily disassociated. It is not unusual, for example, for individuals with significant complaints of insomnia or poor sleep to have essentially normal physiological sleep patterns. Sleep is well known to be easily disturbed by mood and psychological state. Sleep is clearly disturbed by anxiety and in patients with generalized anxiety disorder. Characteristically this is associated with prolonged sleep onset latency and multiple awakenings subsequent to sleep onset. In addition, a well-recognized prodrome to a clinically significant depressive episode is an alteration in sleep pattern which includes an early onset of REM sleep and early morning awakenings with difficulty falling back to sleep. There are also data which document the fact that REM deprivation in depressed patients can produce a significant antidepressant effect.
Good sleep is commonly associated with good health and a sense of well being. Measures of overall functional status have been known to be significantly correlated with both subjective and objective measures of daytime sleepiness. Other studies have shown that sleep disordered breathing is associated with lower general health status, with appropriate controls for body mass index, age, smoking status, and a history of cardiovascular conditions. Even very mild degrees of sleep disordered breathing have been shown to be associated with subjective decrements in measures of health status which are comparable to those individuals with chronic disease such as diabetes, arthritis, and hypertension.
Complaints of poor sleep and/or insomnia, and daytime sleepiness and fatigue are common. A recent Gallop survey in the USA indicated that approximately one third of Americans have insomnia. Thirtysix percent of American adults indicated some type of sleep problem. Approximately 27 percent reported occasional insomnia, while 9 percent indicated that their sleep-related difficulty occurs on a regular, chronic basis. In a study of a large sample of Australian workers, the prevalence of a significant elevation in the Epworth Sleepiness Scale was just under 11 percent. These data were not related significantly to age, sex, obesity, or the use of hypnotic drugs. Perhaps the most common cause of daytime fatigue and sleepiness, aside from self-imposed sleep restriction, is obstructive sleep apnea. The sine qua non of this sleep disorder is persistent sonorous snoring. Snoring itself is the most obvious manifestation of an increase in upper airway resistance, and as it progresses to more significant levels, the upper airway gradually diminishes in cross-sectional diameter and may produce a complete occlusion. Sonorous snoring can exist as a purely social nuisance or it can be associated with multiple episodes of partial and complete upper airway obstruction during sleep associated with dangerously low levels of oxygen saturation. This sleep-related breathing disorder is also associated with complaints of daytime fatigue and sleepiness that may be only minimally obvious to some individuals, but can be quite severe and debilitating in others (Orr 1997).
3. Sleep Disorders
There are a variety of documented sleep disorders which have been described in a diagnostic manual which can be obtained through the American Academy of Sleep Medicine. This manual describes the diagnostic criteria of a plethora of sleep disorders ranging from disorders which manifest themselves primarily as symptoms, i.e., insomnia, narcolepsy, to physiologic disorders which can be defined only through a polygraphic sleep study such as sleep apnea, periodic limb movements during sleep, and nocturnal gastroesophageal reflux. The prevalence of these disorders varies from narcolepsy (5–7 cases per 10,000) to OSAS (2–4 cases per 100) to insomnia which may be as high as 25 percent of the general population who report occasional problems with this disorder. Space constraints do not permit a discussion of all of these disorders, therefore we will touch only on the most commonly encountered sleep disorders.
Clearly, sleep disorders have well-documented consequences with regard not only to health but to daytime functioning. Perhaps the most common of all relates to the behavioral consequences of sleep fragmentation or sleep restriction. Either as a result of anxiety, or a physiologic sleep disturbance, sleep restriction and sleep fragmentation can produce documentable declines in performance, and increases in daytime sleepiness. The effects of even minimal sleep restrictions are cumulative across nights, but the effects can be quickly reversed in a single night of normal sleep. Sleep restriction is commonly noted in shift workers; it is estimated that approximately 30 percent of the American work force works rotating shifts, or a permanent night shift. Even permanent night shift workers rarely obtain ‘normal’ sleep in the daytime, and complaints of inadequate or nonrestorative sleep are persistent in this group of workers. Studies have shown that accidents are 20 percent higher on the night shift, and 20 percent of night shift workers report falling asleep on the job. The demands of our increasingly complex technologic society have created a workforce that is under greater stress, obtaining less sleep, and clearly increasing prevalence of sleep complaints and sleep disorders.
An epidemiological study has estimated the prevalence of sleep disordered breathing (defined as five obstructive events per hour or greater) was 9 percent for women and 24 percent for men (Young et al. 1993). It was estimated that 2 percent of women and 4 percent of middle-aged men meet the minimal diagnostic criteria for sleep apnea, which includes five obstructive events per hour with the concomitant symptom of daytime sleepiness. Although, obstructive sleep apnea syndrome (OSAS) is felt to be a predominantly male phenomenon, the incidence rises sharply among postmenopausal women. Persistent, loud snoring, and the concomitant upper airway obstruction, has been shown to carry with it a variety of medical and behavioral risks. Various studies have shown that snoring is a significant predictor of hypertension, angina, and cerebral vascular accidents independent from other known risk factors. One study has shown in a multiple regression analysis that snoring was the only independent risk factor which differentiated stroke occurring during sleep and stroke occurring at other times of the day. Other studies have documented a higher mortality rate in patients with moderate to severe OSAS compared to those with a less severe manifestation of this disorder. Furthermore, other studies have shown that in individuals with curtailed life expectancy secondary to OSAS, the most common cause of death was myocardial infarction. Other studies have confirmed that more aggressive treatment of OSAS reduces the incidence of vascular mortality (Hla et al. 1994).
The issue of the relationship between snoring, OSAS, and hypertension is somewhat controversial. The frequent association of significant OSAS with male gender, and obesity make it difficult to determine the relative contribution of each variable to hypertension. One large population study of 836 males from a general medical practice in England revealed a significant correlation between overnight hypoxemia and systemic blood pressure, but this could not be determined to be independent of age, obesity, and alcohol consumption (Stradling and Crosby 1990). No significant relationship was found with snoring. Alternatively, another excellent study which actually utilized overnight polysomnography and 24-hour ambulatory blood pressure monitoring did find an association between hypertension and sleep apnea which is independent of obesity, age, and sex in a nonselected community based adult population (Hla et al. 1994). Clinically, it is recognized that appropriate treatment of OSAS will often result in a notable reduction in blood pressure, often independent of weight loss. In a recent National Institute of Health supported project on sleep and cardiovascular functioning, preliminary data have shown that 22 to 48 percent of hypertensive patients have been observed with significant OSA, and 50 to 90 percent of sleep apnea patients have been documented to have hypertension.
Perhaps the most well-known ‘sleeping disorder’ or ‘sleep sickness’ is narcolepsy. Long assumed to be synonymous with uncontrollable daytime sleepiness, narcolepsy is now known to be a neurological disorder, and genetic abnormalities have recently been described in a canine model of narcolepsy. This disorder is associated with an extraordinary degree of daytime sleepiness but that alone does not define the syndrome. Many individuals with OSAS also have an equivalent degree of daytime sleepiness. Narcolepsy is identified by other ancillary symptoms. Perhaps the most common and dramatic is cataplexy in which individuals have a partial or complete loss of skeletal muscle control in the face of emotional stimuli such as fear, anger, or laughter. In the sleep laboratory, narcolepsy is associated with a unique pattern of sleep where an onset of REM sleep is noted usually within 10 to 15 minutes after sleep onset. This is considered to be a pathognomonic sign of narcolepsy. Unfortunately, there is no cure for narcolepsy at the present time, and treatment is limited to the symptomatic improvement of daytime sleepiness with stimulant medication, and the control of the ancillary symptoms primarily via tricyclic antidepressant medication.
The results of the Gallop survey indicated that 36 percent of American adults suffer from some type of sleep problem. Approximately 25 percent reported occasional insomnia, while 9 percent said that their sleep-related difficulty occurs on a regular or chronic basis. In addition, the survey documented that insomniacs were 2.5 times more likely than noninsomniacs to report vehicle accidents in which fatigue was a factor. In addition, compared to noninsomniacs, insomniac patients reported a significantly impaired ability to concentrate during the day. The welldocumented excessive daytime sleepiness in patients with obstructive sleep apnea has been documented in several studies to result in a significant increase in traffic accidents, as well as at-fault accidents (Findley et al. 1989). The extreme sleepiness noted in patients with OSAS is almost certainly the result of an extreme degree of sleep fragmentation secondary to arousals from sleep by repeated events of obstructed breathing. Furthermore, it is well established that the sleepiness experienced by patients with OSAS is completely reversible by appropriate therapy which resolves the sleep related breathing disorder. The most common approach to therapy currently is the application of a positive nasal airway pressure via a technique referred to as continuous positive airway pressure (CPAP).
The effects of sleep deprivation, either as a result of willful sleep restriction, poor sleep secondary to insomnia, or fragmented sleep secondary to OSAS, has substantial effects on physical and behavioral health as noted above. Studies on chronic sleep deprivation have shown minimal physiologic effects, but have documented dose related effects in performance decrements and decreased alertness. More recently, however, an extraordinary set of studies has demonstrated that long-term sleep deprivation does have very significant effects in rats, and can ultimately result in death. The most likely explanation of death appears to be the result of a profound loss of thermal regulation (Rechtschaffen 1998). Also of interest, are recent studies which suggest alterations in immune function secondary to chronic sleep deprivation in humans.
In conclusion, the intuitive notion that sleep has important consequences with regard to one’s health appears to be clearly documented. Alterations in sleep producing a fragmentation of sleep or restriction in the normal duration of sleep have been shown to have significant consequences with regard to waking behavior. In addition, sleep disorders which fragment sleep such as obstructive sleep apnea produce effects that relate not only to waking behavior, but also have significant consequences with regard to both cardiovascular and cerebral vascular complications as well as producing a significant increase in mortality. Perhaps, the most important message to be gleaned from the remarkable increase in our knowledge of sleep is that sleeping behavior affects waking behavior and waking behavior affects sleeping behavior.
Bibliography:
- Carskadon M, Dement W 1994 Normal human sleep: An overview. In: Kryger M, Roth T, Dement W (eds.) Principles and Practice of Sleep Medicine. Saunders, Philadelphia, PA
- Dement W C 1990 A personal history of sleep disorders medicine. Journal of Clinical Neurophysiology 7: 17–47
- Findley L J, Fabrizio M, Thommi G, Suratt P M 1989 Severity of sleep apnea and automobile crashes. New England Journal of Medicine 320: 868–9
- Hla K M, Young T B, Bidwell T, et al 1994 Sleep apnea and hypertension. Annals of Internal Medicine 120: 382–8
- Orr W 1997 Obstructive sleep apnea: Natural history and varieties of the clinical presentation. In: Pressman M, Orr W (eds.) Understanding Sleep. American Psychological Association, Washington, DC
- Rechtschaffen A 1998 Current perspectives on the function of sleep. Perspectives in Biology and Medicine 41: 359–90
- Stradling J R, Crosby J H 1990 Relation between systemic hypertension and sleep hypoxaemia or snoring: Analysis in 748 men drawn from general practice. British Medical Journal 300: 75
- Young T, Palta M, Dempsey J, et al 1993 The occurrence of sleep-disordered breathing among middle-aged adults. The New England Journal of Medicine 328: 1230–5




