Sample Obsessive-Compulsive Disorder Research Paper. Browse other research paper examples and check the list of research paper topics for more inspiration. If you need a religion research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our research paper writing service for professional assistance. We offer high-quality assignments for reasonable rates.
1. Clinical Aspects
1.1 Clinical Symptomatology And Course
Obsessive–compulsive disorder (OCD) is a chronic, disabling disorder that is characterized by recurrent obsessions and uncontrolled compulsions. Obsessions are defined as persistent ideas, thoughts, impulses, or images that are experienced as intrusive and inappropriate. Usually patients attempt to ignore or suppress the obsessions, which typically deal with contamination, doubts, or aggressive imaginations. Compulsions are repetitive behaviors (e.g., hand-washing, checking locked doors) or mental acts (e.g., counting, repeating words) that the person feels driven to perform in response to an obsession or according to rigid rules. Characteristically, compulsions counteract the anxiety associated with an obsession. Diagnosis by DSM IV also requires that the person recognize that the obsessions or compulsions are excessive or unreasonable; they must also cause marked distress, consume at least one hour a day, or considerably interfere with daily functioning.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
OCD typically begins in late adolescence, though onset in childhood is not uncommon. The disorder tends to exhibit a waxing and waning course over the life span, with periods of relative good functioning and limited symptoms punctuated by periods of symptomatic exacerbation. A small minority of subjects exhibits either complete remission of their disorder or a progressive, deteriorating course. There is a high comorbidity with major depression, panic disorder, phobias, and eating disorders. Approximately half of all patients with Tourette’s disorder meet criteria for OCD, although less than 11 percent of patients with OCD meet criteria for Tourette’s disorder.
1.2 Differential Diagnosis
Obsessive–compulsive (OC) symptomatology is also found in various other psychiatric disorders. It can be difficult to differentiate OCD from major depression, which is sometimes associated with obsessive thoughts. In contrast to OCD, obsessional thinking in depression usually subsides in parallel to the remission of depression. Psychotic symptoms can also provoke obsessive thoughts and compulsive behaviors, but are accompanied by other characteristics of schizophrenia. Principally, OCD patients differ from schizophrenic patients by their knowledge that obsessions and compulsions are inappropriate, absurd, or irrational (‘egodystonic’). However, when the condition is very severe the patient might experience his obsessions or compulsions as more ego-syntonic and is transiently not sure about the real risk of danger or the real necessity to perform a certain ritual in order to prevent a negative event. There is a subgroup of OCD patients who are frequently misdiagnosed as schizophrenic due to these ‘psychosis-like symptoms’. OCD also displays some similarity to obsessive–compulsive personality disorder, which is associated with an obsessive concern for details, perfectionism, and rigidity. However, a genuine syndrome of obsessions and compulsions is not present in obsessive–compulsive personality disorder. Patients with OCD experience distress connected with their symptoms. By contrast, the traits of patients with obsessive–compulsive personality disorder very often disturb others more than themselves. Finally, OCD is sometimes misdiagnosed in patients suffering from phobias (e.g., phobic avoidance of any assumed risks to be infected by the AIDS virus). However, phobic patients never develop the kind of rituals which are characteristic of OCD.
1.3 Epidemiology
The lifetime prevalence in the US, Canada, and comparable countries has been found to be 2.2 to 2.3 per 100 persons (Kessler et al. 1994); in other countries, prevalence rates were between 1 and 3 percent. Most remarkably, these rates contradict the previous traditional view of OCD as a rare disorder on the basis of published clinical reports.
2. Pathogenesis
There is strong evidence that neurobiological as well as psychological factors play an important role in the pathogenesis of OCD. Phenomenological similarities between focal dystonias and OCD are related to the persistent, perseverative, repetitive and involuntary nature of the symptoms. The occurrence of OC symptoms as part of the postencephalitis Parkinsonian syndrome (Schilder 1938) stimulated the search for a biological link between basal ganglia dysfunction and OC symptomatology. Compulsive behavior and ob- sessional thinking have been observed after basal ganglia lesions (Laplane et al. 1989, Swedo et al. 1989) and in patients with Gilles de la Tourette’s syndrome (Pauls et al. 1986). Accordingly, symptomatic dystonias can be associated with structural brain lesions (Kostic et al. 1996). Patients suffering from spasmodic torticollis (Bihari et al. 1992) or from blepharospasm, conditions which are also related to basal ganglia dysfunction, showed significantly more OC symptoms than normal controls or patients with hemifacial spasms, a condition with similar symptomatology, but caused by an irritation of the facial nerve (Broocks et al. 1998b).
2.1 Neuroanatomical Hypothesis Of OCD
Since around 1990 positron emission tomography (PET) and other brain imaging studies have produced further evidence for basal ganglia involvement in the pathogenesis of OCD. It has been postulated that a disturbed striatal filter function causes a disinhibition of cerebral activities generated in orbitalfrontal and cingulate structures (Baxter et al. 1992, Benkelfat et al. 1990, and Schwartz 1998). During an implicit sequence learning task, healthy subjects recruit the right striatum whereas patients with OCD fail to do so and instead exhibit aberrant medial temporal activation that may serve a compensatory function (Rauch et al. 1997). It has been assumed that the striatum may be the principal site of primary pathology in OCD and related disorders, a theory that finds support from models of pathogenesis related to autoimmune processes known to cause striatal damage (Swedo et al. 1989). Also, N-acetyl aspartate (NAA) levels, as measured by magnetic resonance spectroscopy (MRS), which are interpreted as indices of early neuronal degeneration, have been found to be reduced within the striatum (Bartha et al. 1998, Ebert et al. 1997).
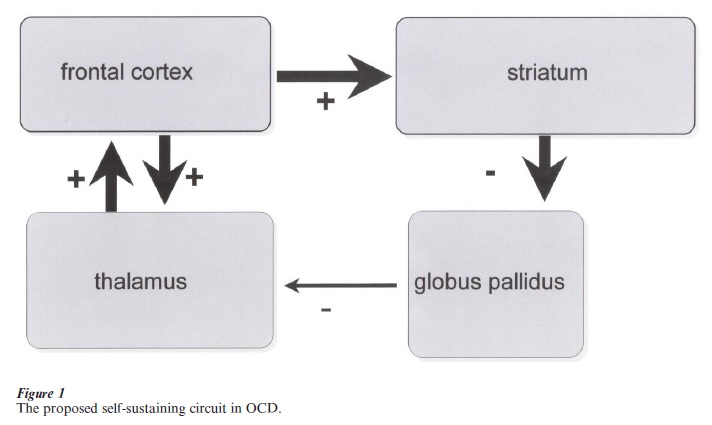
The pathological increase of metabolic activity in the orbitalfrontal cortex (OCF) demonstrated in PET studies that most OCD patients experience the neurobiological expression of the sensations of anxiety and worry. The caudate nucleus and other striatal structures are stimulated by the OCF. Leading researchers in this field have postulated that in OCD a positive feedback mechanism between the OCF and the striatum is activated, which also involves thalamic structures. Physiologically, inhibitory pathways from the caudate nuclei to the thalamus (via the globus pallidum) have the task of keeping this neurosensory circuit in balance. One explanation of the proposed dysbalance in OCD could be that an increased inhibition of the globus pallidum results in a desinhibition of the thalamus creating a self-sustaining circuit (Fig. 1). Pharmacological and neurosurgical interventions are obviously able to decrease this neuronal overactivity with the consequence of decreased OC symptoms. Pretreatment metabolic correlation between orbital cortex and caudate and between orbital cortex and thalamus were abolished by successful CBT (Baxter et al. 1992, Schwartz et al. 1996). It is fascinating that psychological interventions, which are primarily mediated by various cortical structures, are also able to affect these orbitofrontal-subcortical neurocircuits.
Neuropsychological testing has revealed that patients with OCD are impaired on measures of spatial working memory, spatial recognition, and motor initiation and execution (Purcell et al. 1998, Schmidtke et al. 1998). In contrast, performance of these tasks by patients with panic disorder or depression did not differ from that of controls.
2.2 Neurochemical Hypothesis Of OCD
The most compelling findings suggesting a role of serotonergic pathways in the symptomatology of OCD come from well-replicated treatment studies. Most OCD patients improve during treatment with serotonin (5-HT) reuptake inhibitors including clomipramine, fluoxetine, fluvoxamine, paroxetine, and sertraline, but not with non-5-HT selective antidepressants (Murphy et al. 1996, Pigott and Seay 1999). This observation was replicated in a recent multicenter trial enrolling 166 patients with concurrent OCD and major depression, in which the SSRI sertraline was more effective in reducing depressive and OC symptoms than the primarily norepinephrine reuptake inhibitor desipramin (Hoehn et al. 2000). Using a placebo-controlled design, discontinuation of clomipramine was followed by an increase of OCD symptoms (Pato et al. 1991). Interestingly, coadministration of the 5-HT2 receptor antagonist metergoline to OCD patients being treated with clomipramine was associated with higher OC symptoms in comparison to placebo coadministration (Benkelfat et al. 1989). An exacerbation of OC symptoms after administration of the non-selective serotonergic agonist, m-chlorophenylpiperazine (m-CPP) was observed in several, but not all studies (Broocks et al. 1998a, Charney et al. 1988, Hollander et al. 1992, Zohar et al. 1988).
When oral m-CPP was re-administered during chronic treatment with clomipramine (Zohar et al. 1988) or fluoxetine (Hollander et al. 1992, Pigott et al. 1990), OCD patients did not show an exacerbation of OC symptoms although plasma prolactin and cortisol responses to m-CPP were not attenuated. This suggests that chronic clomipramine or fluoxetine treatment in OCD patients may be associated with the development of an adaptive subsensitivity in one or more serotonergic subsystems (Murphy et al. 1996).
2.3 Genetic Findings
In a relatively small twin study concordance rates for OCD showed a non-significant trend towards higher rates in MZ versus DZ twin pairs (33 versus 7 percent). There are only few family studies of OCD employing adequate research methods (operational diagnostic criteria, controls, and blind assessment of relatives). However, two out of three studies indicate familial aggregation in relatives of patients with OCD versus relatives of normal controls. Discrepant findings might reflect differences in methodology as well as etiologic heterogeneity within the diagnostic category. That is why several researches have now begun to subtype patients by such variables as age at onset, presence of neurological symptoms, and symptom patterns of the disorder. There is a familial and perhaps genetic relationship between Tourette’s disorder and chronic motor tics and some cases of OCD. As there is considerable evidence of a genetic contribution to Tourette’s disorder this finding also supports a genetic role in a subset of cases of OCDs.
Recently, new evidence has emerged for possible immunological factors in the pathogenesis of OCD. It has long been known that about 10 to 30 percent of patients with rheumatic fever, caused by a streptococcal infection, develop Sydenham’s chorea. Over 70 percent of these patients manifest OC symptoms in addition to the choreatiform movements. A monoclonal antibody to B lymphocytes, D8/17, developed using mice immunized with B lymphocytes from a patient with rheumatic carditis, has been used to measure B-cell D8/17 antigen in a small sample of patients with childhood onset of OCD or Tourette’s syndrome. A22 31 patients, 29 percent of whom had pure OCD, showed an elevated percentage of D8/17 antigen, contrasted with only 1 of 21 controls. This antigen might therefore serve as a marker for vulnerability to some forms of childhood OCD.
3. Treatment
For decades, OCD has been considered as a fascinating but treatment-refractory mental condition. Conventional pharmacological approaches as well as psychodynamic therapy did not lead to satisfactory improvements of OC symptomatology. The first major advances in the treatment of OCD came from two directions. Clomipramine, which differs from other tricyclic antidepressants by its potent inhibition of serotonin reuptake, proved to exert specific antiobsessional effects. At the same time, the introduction of special cognitive-behavioral techniques began to continuously improve the prognosis of OCD. In the following years, many studies have shown that behavior therapy, especially exposure with response prevention, and selective serotonin reuptake inhibitors (SSRIs) significantly reduce OC symptoms.
3.1 Psychological Treatment
Exposure/response prevention has been compared to various control treatments including relaxation, anxiety management training, and pill placebo (Kozak et al. 1999), leading to solid evidence for the efficacy of this procedure. Summarizing all controlled trials, average responder rates were 83 percent immediately after treatment and 76 percent after an average followup interval of 29 months.
Current exposure/response prevention programs usually combine in vivo exercises to feared stimuli with imaginative exposure. Repeated prolonged exposure leads to a psychophysiological habituation process, which also affects irrational beliefs held by the patient. It is crucial that the duration of the exposure exercise continues at least until the patient experiences a decrease of the induced distress. During this time therapists have to be alert to detect and restrain covert neutralizing thoughts (Salkovskis 1999). If possible, a friend or a family member should be taught to support the patient between sessions in order to achieve adequate exposure. Irrespective of the emotional arousal, the patient has the task to describe precisely the experienced emotions and the accompanying cognitions. This description is the basis of the cognitive restructuring which most therapists view as an essential component of successful exposure.
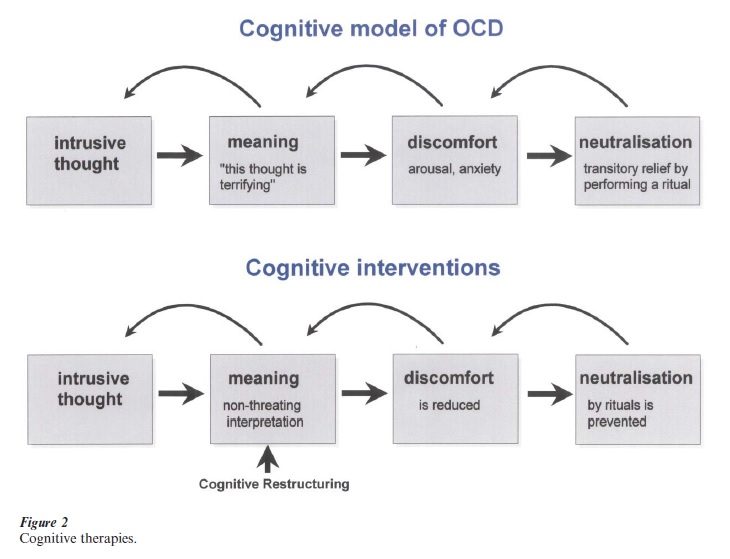
In recent years, cognitive approaches have been proposed for the treatment of OCD, especially obsessional ruminations (Salkovskis 1999). According to the cognitive hypothesis, obsessional problems occur when intrusive cognitions are interpreted as an indication that the person may be responsible for a certain harmful event, which has happened in the past or will happen in the future. Cognitive therapy is thought to work by altering both strongly held beliefs associated with OCD symptoms and interpretations of intrusive mental experiences (Fig. 2). It is also important to help patients to identify and to modify underlying general assumptions, which might represent the roots of the more overt dysfunctional thoughts. As in other anxiety disorders, the general style of therapy is that of guided discovery. Further details of the cognitive treatment of obsessions including the use of loop tapes are described in Salkovskis 1999.
Schwartz has proposed a cognitive-biobehavioral self-treatment for OCD (Schwartz 1996). It integrates the results of neuroimaging research into the cognitive approach based on the literature on the behavioral neurobiology of the basal ganglia. In a four-step process, the OCD patient learns to identify his or her obsessions and compulsions, to label them as such (‘It’s not me, it is my OCD’), and to attribute them to abnormal activity of the fronto-striatal system. While ‘working around OCD symptoms,’ patients learn new adaptive responses to intrusive OCD thoughts and urges. They are tutored to become increasingly aware of avoidance behaviors and to use treatment techniques to perform previously avoided behaviors (Schwartz 1996).
In addition to exposure, response prevention and cognitive techniques, the multimodal treatment of OCD also focuses on social deficits, reduced tolerance for intensive emotions, and reduced emotional awareness. In addition, it deals with deficits in problem-solving and self-initiated alternative behaviors as well as interpersonal problems. In severe cases, complex combinations of multimodal interventions are often needed, including marital or family interventions as well as individual or group treatments. Multimodal CBT has been shown to be effective with very low dropout rates in severely ill inpatients (Hohagen et al. 1998) and outpatients (Hand 1998). Furthermore, its long-term efficacy has been demonstrated in follow-up studies in unselected patients (Hand 1998). Whether multimodal behavioral therapy is superior to exposure therapy alone and whether it is appropriate to treat refusers, dropouts, and nonresponders to conventional exposure therapy with response prevention, are still open questions.
3.2 Drug Treatment
In comparison to clomipramin, selective inhibitors of serotonin reuptake (SSRI) have the advantage of a very low toxicity and a more favorable side effect profile. Consequently, these agents have been the focus of several large-scale, placebo-controlled studies of OCD. Interestingly, very low placebo response rates were observed in most studies. Based on metaanalyses of effect sizes in placebo-controlled trials clomipramine was considered more effective than the SSRIs. However, recent direct comparisons demonstrated similar efficacy between clomipramine and different SSRIs (Pigott and Seay 1999). Pharmacological treatment of OCD usually involves relatively high daily dosages (clomipramine up to 250 mg; fluvoxamine up to 300 mg; fluoxetine, paroxetine, and citalopram up to 80 mg; and sertraline up to 200 mg a day), but some investigators believe that longer duration of treatment rather than higher dosage is essential for response. Ten weeks of treatment trial is currently the minimum recommendation, but it is not unusual to have treatment continue for several months before peak efficacy is reached.
The algorythm in Fig. 3 can be recommended for the pharmacological treatment of OCD patients.
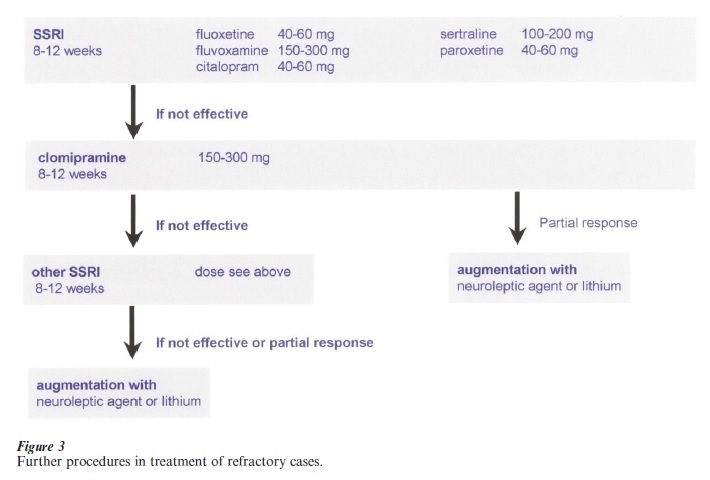
When adequate trials with serotonin reuptake inhibitors, including augmentation strategies, have not been rewarded by a satisfying improvement, it seems justified to try irreversible inhibitors of the monoaminoxydase A such as phenelzyne or tranylcypromine, although the evidence from the literature is not sufficient yet.
When a patient does not respond to a pharmacological or psychological therapy, a repeated motivational and functional analysis might reveal inner resistance and other obstacles which have prevented the patient from therapeutic success so far.
3.3 Combined Pharmacological And Cognitive – Behavioral Treatment (CBT)
Several studies examining the combination of pharmacotherapy with CBT have suggested that the combination of both treatment approaches is associated with only small additional benefits (Cottraux et al. 1993, Foa et al. 1992, Marks et al. 1988, and van Balkom et al. 1998). However, Hohagen et al. 1998 reported that the combination of multimodal CBT with fluvoxamine is superior to the single treatment conditions in patients who suffer predominantly from obsessions or have a high degree of secondary depression.
3.4 Prognosis
The presence of schizotypal, borderline, and avoidant personality disorders predicts a less favorable prognosis, whereas duration of illness, sex, age, and type of symptoms had no clear predictive value. In cognitive behavioral therapy the best predictor of good outcome at the end of treatment and of follow-up was early compliance in doing exposure homework (De Araujo et al. 1996).
4. Summary And Future Tasks
Despite all progress in treatment, a considerable percentage of patients experience only a partial unsatisfactory response. At least 25 percent of OCD patients do not comply with exposure therapy response prevention (Schwartz 1998). In addition to dropouts, 20 percent to 30 percent do not respond sufficiently. Since OCD is a chronic disorder, re- occurrence of the OCD symptomatology is likely when patients do not adhere to the newly adopted cognitive-behavioral habits due to motivational problems, acute life stress, or depression. With SSRI treatment alone, 40–60 percent of patients have not shown significant progress and have to be classified as non-responders.
In summary, there is still an urgent need to improve the present treatment options for OCD. The few ECT case studies in intractable OCD show considerable benefits up to one year, but these results have to be confirmed in controlled trials. There is initial evidence that repetitive transcranial magnetic stimulation affects acute OC symptoms and could represent a new treatment option in future. In severely ill patients, some people can obtain at least partial relief from OCD by neurosurgery (Jenike 1998). The most frequently performed operation, stereotactic subcaudate tractotomy or capsulotomy, intersects the connections between the frontal lobe and the thalamus and exerts its efficacy on the proposed functional imbalance in OCD between the frontal lobe and subcortical structures. Cingulotomy resulted in significant improvement in 25 to 30 percent of patients previously unresponsive to medication and behavioral treatments (Baer et al. 1995). This rate of improvement seems independent of the changes in anxiety and depression scores.
Pharmacogically, new augmentation strategies should be evaluated. The addition of buspirone or lithium has been of limited success, but larger scale studies are required. Interestingly, the addition of haloperidol in patients, who were refractory to adequate treatment with the serotonin-uptake inhibitor fluvoxamine alone, lead to a clinically and statistically significant improvement (McDougle et al. 1994). This effect was strongly related to a comorbid chronic tic disorder, which is present in up to one third of all OCD patients. Because OCD patients typically require prolonged pharmacotherapy, the risk of tardive dyskinesia has severely limited the use of additional neuroleptic treatment in OCD. The development of the new ‘atypical neuroleptics’ which—in clinical dosages—have not been found to induce extrapyramidal side effects (EPS) and tardive dyskinesia could lead to a new intriguing treatment option for OCD patients (Bogetto et al. 2000).
The lack of experienced therapists and the cost of multiple individual treatment sessions raise the question whether these interventions could be applied successfully in a group therapy context. The efficacy, acceptance and cost-effectiveness of short-term interventions for patients suffering from less severe forms of OCD needs further improvement. Self-directed exposure using self-help manuals (Foa and Wilson 1991) seems to be effective in a subgroup of OCD patients. More research is required to identify patients who are able to overcome their problems by pure self-help or manual-guided exposure strategies. Another intriguing research field is the question whether neurobiological abnormalities associated with OCD can be modulated by effective treatment strategies. With cognitive-behavioral treatment, significant decreases in caudate glucose metabolism were found in treatment responders compared with nonresponders. It would be of great interest if parameters, which —in comparison to PET findings—can be more easily measured in clinical settings, turn out to be predictors of treatment success or predictors of relapse at the end of a successful treatment.
Bibliography:
- Baer L, Rauch S L, Ballantine H J, Martuza R, Cosgrove R, Cassem E, Giriunas I, Manzo P A, Dimino C, Jenike M A 1995 Cingulotomy for intractable obsessive-compulsive disorder. Prospective long-term follow-up of 18 patients. Archives of General Psychiatry 52: 384–92
- Bartha R, Stein M B, Williamson P C, Drost D J, Neufeld R W, Carr J J, Canaran G, Densmore M, Anderson G, Siddiqui A R 1998 A short echo 1H spectroscopy and volumetric MRI study of the corpus striatum in patients with obsessive-compulsive disorder and comparison subjects. American Journal of Psychiatry 155: 1584–91
- Baxter L J, Schwartz J M, Bergman K S, Szuba M P, Guze B H, Maziotta J C, Alazraki A, Selin C E, Ferng H K, Munford P 1992 Caudate glucose metabolic rate changes with both drug and behavior therapy for obsessive-compulsive disorder. Archives of General Psychiatry 49: 681–9
- Benkelfat C, Murphy D L, Zohar J, Hill J L, Grover G, Insel T R 1989 Clomipramine in obsessive-compulsive disorder. Further evidence for a serotonergic mechanism of action. Archives of General Psychiatry 46: 23–8
- Benkelfat C, Nordahl T E, Semple W E, King A C, Murphy
- D L, Cohen R M 1990 Local cerebral glucose metabolic rates in obsessive-compulsive disorder. Patients treated with clomipramine. Archives of General Psychiatry 47: 840–8
- Bihari K, Hill J L, Murphy D L 1992 Obsessive-compulsive characteristics in patients with idiopathic spasmodic torticollis. Psychiatry Research 42: 267–72
- Bogetto F, Bellino S, Vaschetto P, Ziero S 2000 Olanzapine augmentation of fluvoxamine-refractory obsessive-compulsive disorder (OCD): a 12-week open trial [In Process Citation]. Psychiatry Research 96: 91–8
- Broocks A, Pigott T A, Hill J L, Canter S, Grady T A, L’Heureux F, Murphy D L 1998a Acute intravenous administration of ondansetron and m-CPP, alone and in combination, in patients with obsessive-compulsive disorder (OCD): behavioral and biological results [In Process Citation]. Psychiatry Research 79: 11–20
- Broocks A, Thiel A, Angerstein D, Dressler D 1998b Higher prevalence of obsessive-compulsive symptoms in patients with blepharospasm than in patients with hemifacial spasm. American Journal of Psychiatry 155: 555–7
- Charney D S, Goodman W K, Price L H, Woods S W, Rasmussen S A, Heninger G R 1988 Serotonin function in obsessive-compulsive disorder. A comparison of the effects of tryptophan and m-chlorophenylpiperazine in patients and healthy subjects. Archives of General Psychiatry 45: 177–85
- Cottraux J, Mollard E, Bouvard M, Marks I 1993 Exposure therapy, fluvoxamine, or combination treatment in obsessive-compulsive disorder: one-year follow-up. Psychiatry Research 49: 63–75
- De Araujo L A, Ito L M, Marks I M 1996 Early compliance and other factors predicting outcome of exposure for obsessive-compulsive disorder. British Journal of Psychiatry 169: 747–52
- Ebert D, Speck O, Konig A, Berger M, Hennig J, Hohagen F 1997 1H-magnetic resonance spectroscopy in obsessive-compulsive disorder: evidence for neuronal loss in the cingulate gyrus and the right striatum. Psychiatry Research 74: 173–6
- Foa E B, Kozak M J, Steketee G S, McCarthy P R 1992 Treatment of depressive and obsessive-compulsive symptoms in OCD by imipramine and behaviour therapy. British Journal of Clinical Psychology 4: 279–92
- Foa E, Wilson R 1991 Stop Obsessing. Bantam, Philadelphia, Vol. ISBN 0553353500
- Hand I 1998 Out-patient, multi-modal behaviour therapy for obsessive-compulsive disorder. British Journal of Psychiatry, (Suppl.) 1998: 45–52
- Hoehn S R, Ninan P, Black D W, Stahl S, Greist J H, Lydiard B, McElroy S, Zajecka J, Chapman D, Clary C, Harrison W 2000 Multicenter double-blind comparison of sertraline and desipramine for concurrent obsessive-compulsive and major depressive disorders. Archives of General Psychiatry 57: 76– 82
- Hohagen F, Winkelmann G, Rasche R H, Hand I, Konig A, Munchau N, Hiss H, Geiger K C, Kappler C, Schramm P, Rey E, Aldenhof J, Berger M 1998 Combination of behavior therapy with fluvoxamine in comparison with behaviour therapy and placebo. Results of a multicentre study. British Journal of Psychiatry, (Suppl.) 1998: 71–8
- Hollander E, DeCaria C M, Nitescu A, Gully R, Suckow R F, Cooper T B, Gorman J M, Klein D F, Liebowitz M R 1992 Serotonergic function in obsessive-compulsive disorder. Behavioral and neuroendocrine responses to oral m-chlorophenylpiperazine and fenfluramine in patients and healthy volunteers. Archives of General Psychiatry 49: 21–8
- Jenike M A 1998 Neurosurgical treatment of obsessive-compulsive disorder. British Journal of Psychiatry, (Suppl.) 1998: 79–90
- Kessler R, McGonagle K, Zhao S, Nelson C B, Hughes M, Eshleman S, Wittchen H U, Kendler K S 1994 Lifetime and 12-month prevalence of DSM-II-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychology 51: 8–19
- Kostic V S, Stojanovic-Svetel M, Kacar A 1996 Symptomatic dystonias associated with structural brain lesions. Canadian Journal of Neurological Sciences 23: 53–6
- Kozak M J, Liebowitz M R, Foa E B 1999 Cognitive Behavior therapy and pharmacotherapy for OCD. In: Goodman W K (ed.) Obsessive-Compulsive Disorder: Contemporary Issues in Treatment. Harper, Washington, DC
- Laplane D, Levasseur M, Pillon B, Dubois B, Baulac M, Mazoyer B, Tran Dinh S, Sette G, Danze F, Baron J C 1989 Obsessive-compulsive and other behavioural changes with bilateral basal ganglia lesions. A neuropsychological, magnetic resonance imaging and positron tomography study. Brain 112: 699–725
- Marks I M, Lelliott P, Basoglu M, Noshirvani H, Monteiro W, Cohen D, Kasvikis Y 1988 Clomipramine, self-exposure and therapist-aided exposure for obsessive-compulsive rituals. British Journal of Psychiatry 152: 522–34
- McDougle C J, Goodman W K, Leckman J F, Lee N C, Heninger G R, Price L H 1994 Haloperidol addition in fluvoxamine-refractory obsessive-compulsive disorder. A double-blind, placebo-controlled study in patients with and without tics. Archives of General Psychiatry 51: 302–8
- Murphy D L, Greenberg B, Altemus M, Benjamin J, Grady T, Pigott T 1996 The Neuropharmacology and Neurobiology of Obsessive-compulsive Disorder. In: Westenberg H G M (ed.) Advances in the Neurobiology of Anxiety Disorders. John Wiley & Sons Ltd., pp. 279–97
- Pato M T, Zohar-Kadouch R, Zohar J, Murphy D L 1991 Return of symptoms after discontinuation of clomipramine in patients with obsessive-compulsive disorder. American Journal of Psychiatry 145: 1521–5
- Pauls D L, Leckman J F, Towbin K E, Zahner G E, Cohen D J 1986 A possible genetic relationship exists between Tourette’s syndrome and obsessive-compulsive disorder. Psychopharmacol Bulletin 22: 730–3
- Pigott T A, Pato M T, Bernstein S E, Grover G N, Hill J L, Tolliver T J, Murphy D L 1990 Controlled comparisons of clomipramine and fluoxetine in the treatment of obsessive-compulsive disorder. Behavioral and biological results. Archives of General Psychiatry 47: 926–32
- Pigott T A, Seay S M 1999 A review of the efficacy of selective serotonin reuptake inhibitors in obsessive-compulsive dis-order. Journal of Clinical Psychiatry 60: 101–6
- Purcell R, Maruff P, Kyrios M, Pantelis C 1998 Neuropsychological deficits in obsessive-compulsive disorder: a comparison with unipolar depression, panic disorder, and normal controls. Archives of General Psychiatry 55: 415–23
- Rauch S L, Savage C R, Alpert N M, Dougherty D, Kendrick A, Curran T, Brown H D, Manzo P, Fischman A J, Jenike M A 1997 Probing striatal function in obsessive-compulsive disorder: a PET study of implicit sequence learning. Journal of Neuropsychiatry and Clinical Neurosciences 9: 568–73
- Salkovskis P M 1999 Understanding and treating obsessive-compulsive disorder. Behavioral Research and Therapy S29–52
- Schilder P 1938 The organic background of obsessions and compulsions. American Journal of Psychiatry 94: 1397–414
- Schmidtke K, Schorb A, Winkelmann G, Hohagen F 1998 Cognitive frontal lobe dysfunction in obsessive-compulsive disorder. Biological Psychiatry 43: 666–73
- Schwartz J M 1996 Brain Lock. Harper Collins, New York
- Schwartz J M 1998 Neuroanatomical aspects of cognitivebehavioural therapy response in obsessive-compulsive dis-order. An evolving perspective on brain and behaviour. British Journal of Psychiatry, (Suppl.) 1998: 38–44
- Schwartz J M, Stoessel P W, Baxter L J, Martin K M, Phelps M E 1996 Systematic changes in cerebral glucose metabolic rate after successful behavior modification treatment of obsessive-compulsive disorder. Archives of General Psychiatry 53: 109–13
- Swedo S E, Rapoport J L, Cheslow D L, Leonard H L, Ayoub E M, Hosier D M, Wald E R 1989 High prevalence of obsessive-compulsive symptoms in patients with Sydenham’s chorea. American Journal of Psychiatry 146: 246–9
- van Balkom A J, de Haan E, van Oppen P, Spinhoven P, Hoogduin K A, van Dyck R 1998 Cognitive and behavioral therapies alone versus in combination with fluvoxamine in the treatment of obsessive compulsive disorder. Journal of Nervous and Mental Disease 186: 492–9
- Zohar J, Insel T R, Zohar Kadouch R C, Hill J L, Murphy D L 1988 Serotonergic responsivity in obsessive-compulsive disorder. Effects of chronic clomipramine treatment. Archives of General Psychiatry 45: 167–72




