View sample mental health research paper on mental health epidemiology. Browse other research paper examples for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Overview
Background
Epidemiology (derived from the Greek epi meaning upon, demos meaning people, and logos meaning study) is the study of factors that influence the occurrence, distribution, prevention, and control of diseases and other health-related events in human populations. It provides a framework that helps public health officials identify important health problems, their magnitude and causative factors.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
Epidemiology has been traditionally an observational science of populations but more recently newer areas in the field (e.g., clinical epidemiology) have initiated interventions in populations. By determining the personal characteristics and environmental exposures that increase risk for disease, epidemiologists identify individual risks and assist in the development of public health policy to alleviate personal and environmental exposures. They have helped to understand the factors that influence the risk of developing chronic diseases such as schizophrenia.
A variety of types of studies are used in epidemiology. The most common found in mental health are cross-sectional (prevalence) studies. Data from such studies have been used to determine levels of need, to identify groups that are at highest risk for disease, and to determine changes over time in the occurrence of disorders. Such data are particularly informative in public policy for allocating resources and developing public health prevention strategies. More recently, psychiatric epidemiology has focused on determining better ways to classify people into more homogeneous disease groups to focus interventions into populations in which they will be most successful. In addition, the field has sought to determine risk factors (including biological and social) for the development of disorders to promote future efforts at prevention. One of the key issues is identification of the factors that are responsible for the occurrence of a particular mental health problem.
The purpose of this research paper is to provide a general overview of epidemiology in the mental health area. The term mental health in this research paper refers to conditions defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM) and the International Statistical Classification of Diseases and Related Health Problems (ICD) Classification of Mental and Behavioral Disorders. Thus, it will refer to disorders that are sometimes called psychiatric or neuropsychiatric (including substance use disorders). This research paper presents key examples of methods and assessment instruments used in mental health epidemiology. However, a detailed review and discussion of epidemiologic methods and instruments is beyond the scope of this research paper. For such details, the reader is referred to several textbooks on mental health epidemiology listed in the ‘Further reading’ section.
History
The early period of epidemiology is marked by a focus on health issues related to the growing industrial revolution in Europe. Public health officials were concerned with general social reform and the effects of overcrowding in urban industrial areas, with an emphasis on sanitary conditions. In the mental health area, there was concern that environmental toxins were the cause of disorders. For example, mercury was considered a cause of psychosis and lead exposure was suspected as a contributor to mental disorders. One of the early founders of epidemiology, William Farr, was among the first to study mental illnesses. He studied the physical condition of inmates in English asylums in the early part of the nineteenth century. During this time, many thought there was a virtual epidemic of mental illness but another important figure in epidemiology, John Snow, insisted the increase was more likely the result of an increase in detection rather than a true increase in incidence.
The second period in the development of epidemiology began around the start of the twentieth century and focused on germs as a cause of disease. Epidemiology became virtually synonymous with the study of infectious diseases. One of the causes of insanity identified during this time was the late effects of syphilis. Discovery of the spirochete that causes this illness led to the development of the first medication to stop this infectious agent (Salvarsan 606). Although emphasis was placed on finding infectious agents, there were some epidemiologists at this time who studied other causes of disease. One notable finding during this time was the association of nutritional deficiency with the occurrence of pellagra. Initially it was thought to be due to an infectious agent but studies in institutionalized populations (including those in mental institutions) led to the association with nutritional deficiency.
After the Second World War, infectious diseases started to decline in the higher-income countries. However, those countries realized the increasing importance of noncommunicable diseases such as cardiovascular disease. This led to a move away from consideration of single etiologic factors and to the consideration of various risk factors that could lead to disease development. New methods such as cohort and case-control designs were developed to identify these risk factors. Mental illnesses were also considered to be chronic noncommunicable disorders, but initial epidemiological work in psychiatry focused more on counting disease in community surveys rather than the study of risk factors. Thus, there were very few cohort or case-control studies in the early part of this era that focused on mental illnesses. Most of the studies in mental health during the initial years of this period were unstructured face-to-face field surveys with poor reliability.
In the late 1970s during the Carter administration in the United States, a special commission on mental health called for a study to obtain information on mental illness across the United States. Around the same time, the third edition of the Diagnostic and Statistical Manual (DSM-III) was published in the United States. It moved toward use of explicit criteria to make a diagnosis and increased the reliability of making such diagnoses. This standard nomenclature made it possible to develop measures that could be used in large community surveys.
Substance abuse had for some time not been considered a true disorder but rather a weakness of character or a personality disorder. However, after the Second World War it was recognized as a major public health problem, and the field sought to quantify it through assessments that focused on alcohol and drug use disorders. As a result of this effort, the significant impact of such disorders has now been recognized as well as the frequent comorbidity with other psychiatric disorders.
In recent years, mental health epidemiology has expanded to include attention to genetics and the molecular basis of disease. This has brought more attention to determination of biological risk factors through the field of genetic epidemiology. Attention has also been focused on social processes that can affect exposure to risk factors. This field of social epidemiology seeks to understand how social factors might influence differences in health status across populations.
Methods
Issues For Mental Health
One of the major problems in psychiatric epidemiology has been the difficulty in measuring mental and substance abuse disorders reliably and validly. Determination of a case is made on the basis of symptoms and not clear objective signs like a biopsy result. Because diagnosis is dependent on symptom reports from individuals there can be significant problems with biased reporting (both over and underreporting). A key concern is the lack of objective, well-defined biological markers of mental illness.
There are continuing debates in the field about how to define the presence of an illness and whether there should be categorical definitions or use of a dimensional model. A dimensional approach focuses on a collection of symptoms and involves a quantitative assessment of the number of symptoms a person has from a few to many. Another approach is to define pathology in terms of a syndrome. In this scheme, a pattern of symptoms may include essential symptoms and others associated with the syndrome. This type of scheme takes the duration of symptoms into consideration and may include severity of the symptoms and resulting disability. Depending on the types of symptoms present, the duration and disability, a syndrome may be considered to be present or absent. Thus, this becomes a dichotomous measure (present or absent) and the resulting conditions are placed into categories of disorders.
Other problems in making diagnoses in mental health are the changes in symptoms over time, even without treatment, and the potential for recall bias (i.e., failure to remember past symptoms). The latter is a particular problem when trying to assess lifetime diagnoses. Stigma may also affect what a person reports about his/her behavior. Some people may not want to report symptoms due to embarrassment and may not come forward for treatment.
Terms
Below are listed some common terms used in psychiatric epidemiological studies. Familiarity with these will aid the reader in understanding such studies. A more detailed description of the various epidemiologic terms can be found in resources listed in the section titled ‘Further Reading.’
- Case: This represents the presence of a mental or substance abuse disorder in a person.
- Case registry: A database of people with a defined mental and/or substance use disorder. It may include other data such as demographic and clinical treatment information.
- Comorbidity: This is the presence in a person of at least two different disorders. It may be used to represent the occurrence of somatic or psychiatric disorders and simultaneous or lifetime occurrence.
- Control group: This is a group of people who are used as a basis for comparison to another group. Depending on the study design, control subjects do not receive the experimental intervention or are healthy and do not possess the disorder or risk factor in question.
- Incidence: This represents the number of new cases or events that occur during a particular period of time.
- Odds ratio (OR): A measure of the odds of an event/ disorder occurring in one group compared to the odds of the event/disorder occurring in another group. Thus, an odds ratio of one (1) means that the event/ disorder is equally likely to occur in both groups. If the odds ratio is greater than one (>1), then the event/ disorder is more likely to occur in the first group. If less than one (<1), then the event/disorder is less likely to occur in the first group.
- Predictive value of a test: The positive predictive value of a test or screen is the proportion of all people who test positive on a screen who actually have the disorder being screened. The negative predictive value is the proportion of all people who test negative on a screen who do not have the disorder being screened.
- Prevalence: This represents the number of cases/events that exist during a particular period of time. This figure would include both new cases (incidence) and those that were already present but still existed during the defined period of time. It is expressed in terms of the period of time defined to contain the cases or events. Thus, point prevalence would be the prevalence at a specific point in time. Period prevalence would expand the time over which cases or events could be present. For example, one might have one month, 6 months, 12 months (1 year), or lifetime prevalence. Period prevalence is used more often these days in mental health epidemiology because the diagnosis of mental disorders requires the occurrence of symptoms over periods of time.
- Risk factor: This is something that increases the chance for development of a disorder or the occurrence of an event. It is important to note that it is not necessarily causal but rather associated with the disorder or event. There may also be more than one risk factor for a given disorder and a particular combination of such factors may be necessary before a disorder develops. Risk factors can be inherent in the individual (e.g., age and gender) or they may represent an exposure (e.g., substance abuse, economic status).
- Reliability: This is the degree to which any particular measure produces consistent results even among different raters of the measure. Reliability is often a problem in making diagnoses of mental and substance abuse disorders.
- Sensitivity: This represents the proportion of people with a disorder in a population who are identified correctly by a screen or test as having a disorder.
- Specificity: This represents the proportion of people without a disorder in a population who are identified correctly by a screen or test as not having a disorder.
- Validity: This is the extent to which any given indicator of a disease actually represents the presence of that disease. In psychiatry, the gold standard against which validity is most often measured is the diagnosis made by a clinician.
Assessment
Background
The field of psychiatric epidemiology has developed various ways to assess and diagnose mental disorders. Some early studies used direct observation and assessment by clinicians. However, with the growing need for larger community surveys, it became too expensive to use clinicians to make every assessment. As a result, survey instruments were developed that could be used by either clinicians or trained lay interviewers to provide reliable diagnoses of mental illnesses.
Before considering the specific instruments used to measure mental disorders, it is important to understand how such disorders are determined. In psychiatric epidemiological studies, disorders are assessed usually through a set of defined questions. The set of questions is known as an instrument or test and can be divided into two types: A scale or schedule. An instrument can be administered through direct observation by a clinician, through trained lay interviewers, or self-report by the subject.
A scale is sometimes called a screen and usually focuses on the dimensional aspect of pathology. Responses to items or questions on a scale are given individual values and when added provide a score. The presence of pathology is determined by this overall score.
A schedule is more comprehensive and complex than a scale and determines various diagnoses through a structured set of questions. Some instruments have been designed to be administered by trained lay people (i.e., nonclinicians) in community settings. In addition, schedules determine if the symptoms are present at the time of the interview or occurred at some other point in time. They are designed to contain a variety of disease modules so one can opt to assess a selected number of diagnoses. Some are designed so a respondent who answers negatively to certain stem questions for a particular disease can skip the rest of the module.
Concern has been raised about the validity of schedules used in epidemiological studies. They may overestimate the prevalence of disorders, especially if compared to assessments made by clinicians. However, some recent studies seem to indicate clinician assessments may actually result in a larger number of identified cases (i.e., a higher prevalence) unless one looks only at recent symptoms when clinician assessments may have lower estimates of pathology. In addition to concerns about reliability and validity, a major issue is whether dimensional or categorical measurement is better. The concern is that categorical measurement is too restrictive and human behavior is not so easily divided into strict categories. Yet, dimensional measures such as scales often use cut points and thus create categories, while categorical measures involve some dimensional qualities. Most branches of medicine use categorical diagnoses; thus such approaches are compatible with general medical diagnostic practice.
Instrument Development
During the Second World War, several scales were developed to assess psychopathology such as the Maudsley Personality Inventory in the United Kingdom. The first structured interviews were conducted in two community surveys shortly after the Second World War. These were the Stirling County Study and the Midtown Manhattan Study. They used the Health Opinion Survey and the Twenty-Two Item Scale, respectively. Yet, the studies did not rely on the instruments for final diagnoses. Instead, they had psychiatrists review the results from the instruments. In spite of some differences in the way the two studies assessed psychiatric conditions, they both reported that about 20% of people had a mental disorder.
President Carter’s Commission on Mental Health called for national information on psychiatric disorders and use of mental health services in the United States at the start of the 1980s. This led to the development of the Epidemiologic Catchment Area (ECA) study, the first national epidemiologic survey for psychiatric conditions in the United States. The Diagnostic Interview Schedule (DIS) was developed for use in the ECA. It was the first complex diagnostic schedule designed to be used in a community study and set the stage for future epidemiologic surveys around the world.
Around the time of the ECA study, the WHO collaborated with the U.S. Alcohol, Drug Abuse and Mental Health Administration to assess the state of international diagnosis and classification. A product of this collaboration was the development of a new instrument, the Composite International Diagnostic Interview (CIDI). This instrument is highly structured and does not allow interviewers to interpret responses, as was allowed in some early international studies that used the Present State Examination (PSE) developed in the United Kingdom. One version of the CIDI, the UM-CIDI, was used in the U.S. National Comorbidity Survey (NCS). The CIDI has been used in a variety of international epidemiologic surveys, including national surveys in Australia and Norway. The latest version is being used in the World Mental Health Project, which is attempting to provide an international estimate of mental disorders and the disability associated with them.
Instruments have also been developed for use in various clinical settings (e.g., primary care settings). The most prominent of these is the General Health Questionnaire (GHQ ). Other instruments designed for this setting are the Personal Health Questionnaire, the Patient Health Questionnaire, the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36), and the Primary Care Evaluation of Mental Disorder (PRIME-MD).
Other instruments have been designed to allow clinicians to make reliable assessments of patients in clinical settings. Among the most prominent of these is the Hamilton Rating Scale for assessment of depressive symptoms. Others include the Schedule for Affective Disorders and Schizophrenia (SADS) and the Structured Clinical Interview for DSM-III-R (SCID).
The selection of an instrument depends on what one wants to do with it. For example, if one wants to compare community data to those being collected around the world the choice at this time is the CIDI as it is being used in the largest international study to date.
Study Designs
Here are described the common study designs and examples of each related to mental health and substance abuse. The most common design used in traditional mental health epidemiological studies is the cross-sectional (prevalence) survey.
Nonexperimental Or Observational
In these types of studies, an investigator does not have control over exposure to an intervention or risk factor in any particular group. There are three basic types summarized here.
Cross-Sectional (Prevalence) Surveys
In this type of study, one selects a population and determines the presence or absence of a disease or exposure to a risk factor by assessing the subject at a single point in time. The subject may be asked about past events but is not followed for any period of time. The classic epidemiological surveys in psychiatry have been cross-sectional in design (e.g., the ECA study). These studies are useful in determining the mental health status and service needs of community populations. A variety of techniques are used to sample community populations for such studies (e.g., stratified random sampling). A few of these cross-sectional studies have had additional follow-up interviews with subjects (e.g., the Stirling County Study). Such studies with a repeated assessment could be considered a hybrid design.
In addition, the type of instrument used in a cross-sectional survey can vary. One might create a case registry such as that used by the National Health Insurance in the United Kingdom. These could use assessments by both clinicians and individually administered instruments. However, a typical design is to administer an instrument to every subject from a survey population. A less expensive option is a two-stage design in which people are first given a short instrument (e.g., a scale) and those who test positive are then given a more thorough instrument to assess psychopathology.
Case-Control Study
In this type of study, one selects two different groups to compare. One is a group of people with the condition one wants to study (cases) and the other is a group of people who are as similar as possible to those people with the condition, except they do not have the condition (controls). One looks back in time to determine whether the two groups had different exposure to risk factors of interest. Although these types of studies are subject to potential biases (e.g., selection bias), they are relatively inexpensive and can be conducted quickly. For rare disorders, it is an efficient study design. If a case-control study indicates a finding of interest it can be tested through more rigorous methods such as a cohort study.
Cohort Study
In this type of study, people are selected to be observed over time. These are usually conducted in a prospective (forward) fashion with disease-free subjects but can be done in a retrospective (backward) time fashion as long as the temporal sequence of exposure predating disease onset can be established. In contrast to case-control studies, groups are not defined by the presence of a disease, but rather by the presence of a risk factor or exposure and subjects are followed over a period of time. During the time of study, one looks for the development of new cases (incidence) and attempts to connect exposure to certain risk factors with the development of the disorder. These studies require large numbers of people since only a small number are likely to develop the condition of interest and thus can be quite costly and take long periods of time. Nevertheless, cohort studies can establish without question that risk factors predated disease onset and are an important strategy in epidemiology.
Experimental
Clinical Trials
These types of studies are also known as randomized controlled clinical trials (RCTs). In this type of study, people are allocated randomly to either a group that receives an experimental intervention or a group that does not receive the intervention. Thus, the investigator can control both the distribution of subjects into comparison groups and the experimental condition for a group. By using random assignment, one can reduce greatly or eliminate the potential for selection bias. In addition, raters are usually blinded to the experimental intervention and in many studies placebos are used. Some recent clinical trials have utilized hybrid designs in which subjects are given some choice of the intervention and no placebo is used.
Studies And Results
Listed below are the designs of some of the most influential recent epidemiological studies in mental health. This is followed by a summary of results from these and some other studies. The reader is referred to the published full reports of the studies for comprehensive details and results.
Recent Studies
Epidemiologic Catchment Area Study
The Epidemiological Catchment Area (ECA) Study, funded by the U.S. National Institute of Mental Health, was launched in the early 1980s to assess the prevalence of mental and substance use disorders in the United States and the use of mental health services. Instead of a national probability sample, the ECA used five specific geographic regions in the U.S. to select population samples. Two waves of data were collected from subjects. The first wave started around 1980 and the second wave was collected 1 year later, with the last site finishing in the mid- 1980s. The first wave had a combined sample size of a little over 20 000 people and the second wave was not able to assess about 21% of the first sample. It used the Diagnostic Interview Schedule (DIS) to obtain diagnoses for the major DSM-III diagnoses through trained lay interviewers in face-to-face community interviews. This was a ground-breaking study in that it was the first to use structured complex diagnostic interview schedules to obtain estimates of community mental health.
National Co-Morbidity Survey-Replication
This study is a replication of a similar study (National Co-Morbidity Survey) conducted in the early 1990s on a national sample in the United States. The National CoMorbidity Survey-Replication (NCSR) is part of the World Mental Health Surveys described in the next section and was funded by the U.S. National Institute of Mental Health. It is a nationally representative (United States), cross-sectional household survey of people aged 18 and older. Interviews were conducted in person from 2001 to 2003 by trained lay interviewers using the WMHCIDI. The response rate was approximately 71%, and the sample size was a little over 9200 people.
National Epidemiologic Survey On Alcohol And Related Conditions
The U.S. National Institute of Alcohol Abuse and Alcoholism launched a nationally representative survey of people 18 years and older in 2001. The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) study has two waves of data collection with the first wave completed in 2001–02. Although the survey is of noninstitutionalized populations, it did make an effort to include people who live in housing units more likely to have higher substance use patterns (e.g., shelters and group homes). The response rate for the first wave (81%) was much higher than previous surveys.
The survey used the Alcohol Use Disorder and Associated Disability Interview Schedule-DSM-IV version (AUDADIS-IV). This is a state of the art structured diagnostic interview that is designed to be used by lay interviewers. This instrument was designed to be more accurate than previous instruments in assessing alcohol and substance use disorders. The survey conducted face-to-face interviews with over 43 000 people across the United States.
WHO World Mental Health Surveys
In 1998 the WHO established the World Mental Health Survey (WMH) Consortium to address the limitations of previous surveys of mental health disorders around the world. Prior surveys were unable to adequately assess severity of disorders, interviews used in the surveys were not standardized to allow cross-national comparisons, and the majority of surveys were in high-income countries, thus limiting their generalizability to other areas of the world. The Consortium expanded the CIDI (WMH-CIDI) to include questions that would assess severity, impairment, and treatment. Surveys were then launched in 28 countries in each region of the world, including low-income countries.
Each area is using the WMH-CIDI, a fully structured diagnostic interview that uses trained lay interviewers to obtain information. Age of subjects varies by country, but the most common range is 18 and older. Sample sizes vary by country but all used multistage household probability sampling. Response rates have varied so far from lows around 45% to highs of about 88%. There are differences in the demographics, with some sites having young and less educated populations.
Global Burden Of Disease
In the early 1990s, the WHO supported a study that was the first to use epidemiologic data and projections of disability from various disorders to estimate the public health burden of various medical disorders. The purpose of the study was to quantify the years of healthy life lost as a result of disease in the various countries of the world. The identified measure for this is known as DALYs (disability-adjusted life years) and incorporates death and disability from a disorder. This study, known as the Global Burden of Disease (GBD) study, had a significant influence on the perception of the impact of various disorders. Prior estimates had indicated infectious diseases were the most important causes of public health problems. However, this study, which considered not only mortality from a disease but the burden imposed by living with disability from the disease, changed the perception of which diseases were the most important in terms of impact on public health. Chronic diseases with significant effects on long-term disability (e.g., major depression) now were considered more important from a public health perspective than had previously been projected. There were a number of criticisms about the methodology of the study and concerns about miscalculations of the impact of certain diseases (e.g., HIV/AIDS).
These projections were updated recently by the WHO to consider more current epidemiological data on burden of disease and mortality. In addition, the update moved from considering projections by only the eight regions of the world to project at the country level and then aggregated the results into regional and income-level groups. The various diseases and injury causes were grouped into three levels: Group I (communicable, maternal, nutritional causes), Group II (noncommunicable diseases), and Group III (injuries).
Data On Mental Illness And Substance Use Disorders
Table 1 shows a comparison of data from the three most prominent studies in the United States and a meta-analysis of studies conducted in Europe and the initial findings of the European component of the WHO World Mental Health Surveys. It is important to note that one cannot make clear comparisons across these studies as the time of data collection was different, the samples are obviously different, and the methods varied. However, despite these differences, it is remarkable that estimates are very close in some diseases. The obvious exception is the report from the ESMeD study, which has lower 12-month prevalence estimates. It is not clear why this would be the case, but it represents a summary of data from several European countries and if one looks at the range for those countries (Table 2) there is significant variation. In addition, there were some initial problems in the survey implementation in these countries that could have resulted in lower estimates. The meta-analysis represented in the column labeled Europe presents median estimates and the range is variable for these, especially alcohol dependence, depression, and specific phobia. For substance abuse, the figures from the NCS-R study are probably low because the module used to obtain these diagnoses did not consider responses to questions about dependence in those who did not respond positively to abuse questions.
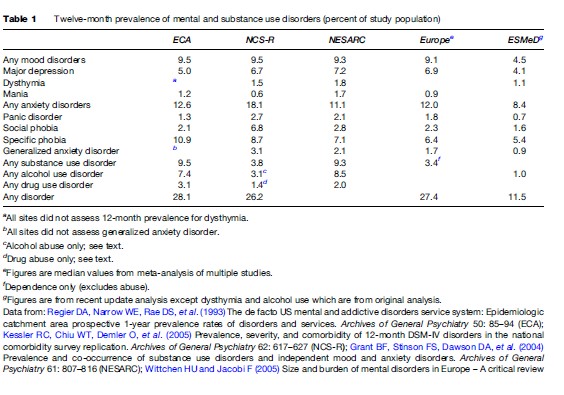
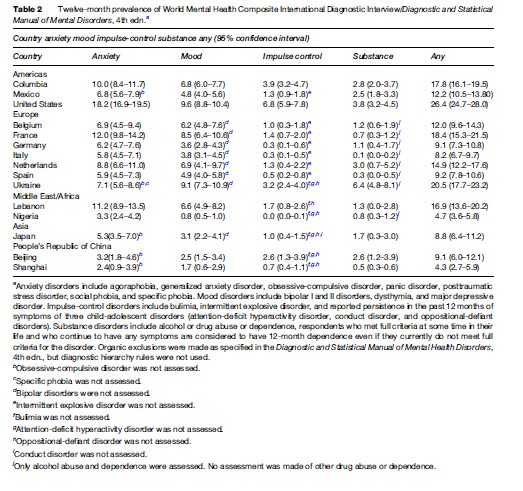
Table 2 shows the first data from the WHO-Mental Health Survey (WMH). The estimates vary across countries despite similar methodology. However, there are likely to be cultural differences in the interpretation of the questions and the concept of mental illness. In addition, the stigma attached to mental illness and substance abuse may be greater in some areas and impede responses to such questions. An issue that often arises in any mental health survey is a concern that the disorders reported do not represent significant clinical problems. Thus, recent surveys such as the WMH have attempted to measure severity and disability. The WMH initial reports show variation in severity and disability but in some settings more than 50% of the cases are of serious or moderate severity. Days out of work are much higher for those with serious disorders than those classified as having mild severity.
Data On Comorbidities
Among the interesting findings from recent studies is the recognition that mental disorders and substance use disorder are comorbid at higher levels than was previously expected. The NESARC study found that 20% of people with a current substance use disorder also had a mood disorder. These disorders appear to be independent and not substance induced. Such findings on co-morbidity are important as they point to the need to assess and provide services for both mental and substance abuse disorders when a person is seen initially for one or the other disorder. There are no current data to clarify this increased co-morbidity among mental and substance abuse disorders. One may lead to the onset of the other type of disorder, there may be common genetic or environmental causes or the methods used to assess these disorders may overestimate co-morbidity. An understanding of these linkages could aid in development of preventive and treatment interventions for co-morbidity.
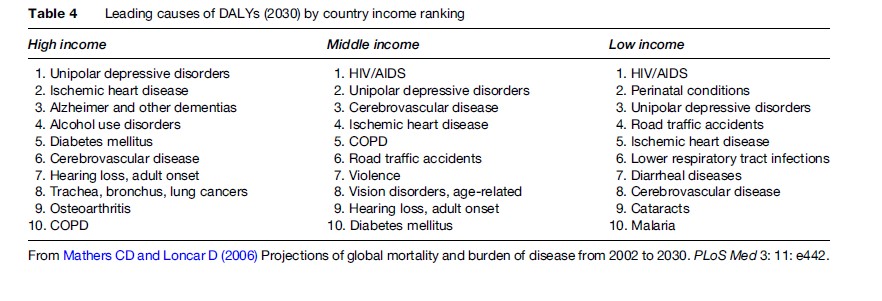
Burden Of Disease Data
One can see in Table 3 that noncommunicable diseases (Group II) are the most important causes of disease burden. By the year 2030, Group II causes are expected to have a greater impact on overall burden of disease around the world than Group I (communicable) causes. Table 4 shows that major depression becomes a significant factor in the overall burden of disease regardless of a country’s income level.
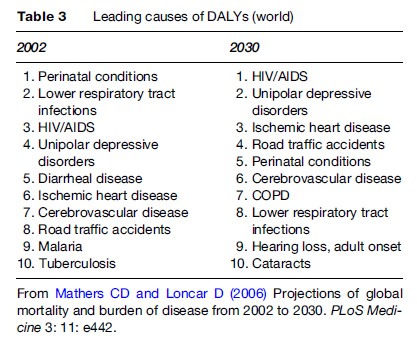
Although these updated projections address some of the criticism of the original Global Burden of Disease Study, there are still limitations to the study. Recent epidemiological studies such as the WHO-WMH study have improved what data are available for mental health, but there are still problems in the quality of such epidemiological data across regions. In addition, measures of disability are not ideal and projections are based on present data and various assumptions about future disease that could change with time. Thus, although data such as these are helpful for planning distribution of future health services, they must be interpreted with caution.
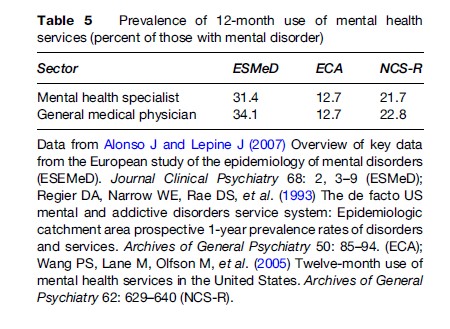
Service Use Data
Many of the epidemiological studies have assessed use of mental health services. As can be seen in Table 5, large numbers of people with a mental disorder during a 1-year period do not seek medical care for such services. Obviously, such data will differ according to the ability to access such services and the stigma attached to using them. However, it is interesting to note that even within countries that provide universal coverage there is still a large amount of unmet need (low use in those with disorders). The studies also looked at the use of a variety of other service sectors (including nontraditional providers). Such data show that even though significant numbers of people use other service sectors for mental health care there are still large numbers of people with a disorder who do not seek care anywhere. Those least likely to use services are the elderly, men, people without resources such as insurance, and those living in rural areas where care is not readily available.
Future Needs
Assessments And Methods
The field of mental health epidemiology has come a long way in the past 100 years, with tremendous growth since the end of the Second World War. Key to this expansion has been the development of explicit criteria for diagnostic assessment. These have increased reliability in making diagnoses and facilitated the development of instruments that can be used in large-scale community surveys. However, a number of issues still confront the field. Among the most prominent is the issue of diagnostic validity. Efforts are underway currently to update the DSM and ICD classification systems. That process has initiated discussions about the best ways to classify mental and substance abuse disorders and whether a more dimensional approach should be considered. Given the growing findings from basic neuroscience and genetics about potential biological causes of mental disorders, there is a need to connect this information with future diagnostic classifications. Collection of biological data in epidemiological studies could help to further this connection.
In addition to classification by symptoms, more attention should be focused on other aspects of disorder such as disability. A number of efforts are already underway in this area, but better assessments of severity, disability, and quality of life are needed. For many people with mental and substance abuse disorders, the most important end points in treatment are improvement in functional status and quality of life, not just a reduction in symptoms.
Previous studies have focused on cross-sectional looks at populations with very few cohort studies. Although they are less costly and perhaps easier to conduct, these prevalence studies have major limitation when trying to determine risk factors for development of disorders. Thus, the field needs to launch large cohort studies that would help delineate the various risk factors (biological, individual, environmental, and social) and the interplay among them. Only more comprehensive information is likely to lead us to a better understanding of the natural history of mental disorders and the various etiological factors that are involved in their development.
More international collaboration would be helpful. Previous studies have shown the importance of mental and substance abuse disorders as public health problems throughout the world. There is much to learn from different regions and standardization of assessments and classification systems together with collaborative large multinational studies would move the field much further.
Topics
A number of recent studies have looked at the interface between mental disorders and other medical disorders such as cardiovascular disease. More work in this area would help to delineate the impact of mental health on other medical disorders and vice versa. This could lead to new interventions for the prevention and early intervention of medical disorders that are co-morbid with mental health disorders.
Given the increasing attention to genetic factors in disease, genetic epidemiological studies in mental health offer an opportunity to understand the complex linkage between genes and environment. Recent work has shown that the presence of certain genes together with certain environmental exposures increases the risk for development of depression. Studies that address the impact of genes on response to pharmacological or psychotherapeutic interventions in the presence of particular environmental exposure would help to revolutionize treatments in mental health.
Epidemiological studies have tremendous potential to inform the allocation of public health resources. However, previous studies have tended to focus on specific individual factors that affect use of resources (e.g., insurance status, availability of services). Studies that address both individual factors and macro-level environmental factors (e.g., organization of services, public mental health policies) at the same time would strengthen the ability to make more informed public policy decisions for the provision of health-care services. This could lead to better systems of care, ensuring that limited services reach those most in need of them.
Bibliography:
- Alonso J and Lepine J (2007) Overview of key data from the European study of the epidemiology of mental disorders (ESEMeD). Journal Clinical Psychiatry 68: 2–9.
- ESEMeD/MHEDEA 2000 Investigators (2004) Prevalence of mental disorders in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatrica Scandinavica Supplementum 109 (supplement 420): 21–27.
- Grant BF, Stinson FS, Dawson DA, et al. (2004) Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Archives of General Psychiatry 61: 807–816.
- Hughes CC, Tremblay MA, Rapoport RN, and Leighton AH (1960) People of Cove and Woodlot: Communities from the Viewpoint of Social Psychiatry. Vol. 2, Stirling County Study of Psychiatric Disorder and Sociocultural Environment. New York: Basic Books.
- Kessler RC, Chiu WT, Demler O, et al. (2005) Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry 62: 617–627.
- Mathers CD and Loncar D (2006) Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 3(11): e442.
- Regier DA, Narrow WE, Rae DS, et al. (1993) The de facto US mental and addictive disorders service system: Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Archives of General Psychiatry 50: 85–94.
- Wang PS, Lane M, Olfson M, et al. (2005) Twelve-month use of mental health services in the United States. Archives of General Psychiatry 62: 629–640.
- WHO World Health Survey Consortium (2004) Prevalence, severity and unmet need for treatment of mental disorders in the World Health Organization world mental health surveys. Journal of the American Medical Association 291: 2581–2590.
- Wittchen HU and Jacobi F (2005) Size and burden of mental disorders in Europe – A critical review and appraisal of 27 studies. European Neuropsychopharmacology 15: 357–376.
- Kessler RC, Demler O, Frank RG, et al. (2005) Prevalence and treatment of mental disorders, 1990 to 2003. New England Journal of Medicine 352(24): 2515–2522.
- McDowell I (ed.) (2006) Measuring Health: A Guide to Rating Scales and Questionnaires. Oxford, UK: Oxford University Press.
- Mezzich JE, Jorge MR, and Salloum IM (1994) Psychiatric Epidemiology: Assessment of Concepts and Methods. Baltimore, MD: Johns Hopkins University Press.
- Murphy JM, Laird NM, Monson RR, et al. (2000) A 40-year perspective on the prevalence of depression. Archives of General Psychiatry 57: 209–215.
- Murray CJL and Lopez AD (eds.) (1996) The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases Injuries and Risk Factors in 1990 and Projected to 2020. Cambridge, MA: Harvard University Press.
- Prince M, Stewart R, Ford T, and Hotopf M (eds.) (2003) Practical Psychiatric Epidemiology. Oxford, UK: Oxford University Press.
- Regier DA, Kaelber CT, Rae DS, et al. (1998) Limitations of diagnostic criteria and assessment instruments for mental disorders. Archives of General Psychiatry 55: 109–115.
- Robins LN and Regier DA (eds.) (1991) Psychiatric Disorders in America: The Epidemiological Catchment Area Study. New York: Free Press.
- Susser E, Schwartz S, Morabia A, and Bromet EJ (eds.) (2006) Psychiatric Epidemiology. Oxford, UK: Oxford University Press.
- Tsuang MT and Tohen M (eds.) (2002) Textbook in Psychiatric Epidemiology. New York: A John Wiley & Sons Inc.
- US Department of Health, Human Services (1999) Mental Health: A Report of the Surgeon General. Rockville MD: US Department of Health and Human Services.
- US Department of Health and Human Services (2001) Mental Health: Culture Race, and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General. Rockville MD: US Department of Health and Human Services.
- World Health Organization (2001) Mental Health: New Understanding New Hope. Geneva, Switzerland: World Health Organization.




