View sample mental health research paper on children’s mental health services. Browse other research paper examples for more inspiration. If you need a thorough research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Definition
Population-based mental health services are services that have been intentionally designed to meet the collective mental health needs of all members of a defined community. Services begin with carefully collected information about the mental health status of all community members. From this assessment, a plan is constructed that describes the mental health services that are needed in the community, who will provide these services, and who will receive them. When there are competing needs for services, decisions to provide some services and not others are based on the relative urgency of community members’ needs and the anticipated outcomes of the services. Once the plan is constructed, mental health services are implemented and include individual, group, or community-wide services, as well as services that are both preventive and remedial, depending on the nature and extent of the risk and disorders present in the community. Finally, the impact of the services and the changing face of the community’s mental health needs are monitored in an ongoing fashion, so that the mental health services plan can be refined to best meet the community’s collective needs. This Assess – Plan – Intervene – Evaluate cycle defines the essential purpose of population-based models of mental health services to ensure that decisions made about a community’s mental health services are intentional and informed by data, and that to the maximum extent possible, existing resources are stretched to meet the collective mental health needs of a community.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
In the United States, population-based mental health services are viewed as a promising alternative to traditional referral-based services for children. In referral-based services, individual children are identified as likely candidates for mental health services by one or more adults and are referred for a comprehensive socio-emotional assessment to identify the nature and extent of their mental health needs. Individual service plans are then developed and specify the services that can and should be provided to the child, and the treatment goals that should guide the services. When services are provided using this referral-based delivery model, multiple epidemiological studies have described a profound discrepancy between the need for and availability of mental health services for children and adolescents in the United States. First, while 20% of children demonstrate a diagnosable psychiatric disorder using the criteria of the American Psychiatric Association’s (2000) Fourth Edition, Text Revision of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IVTR), only 5–7% of children are actually receiving mental health services (Doll, 1996; Strein et al., 2003). Second, referral-based models generally restrict mental health services to children who already demonstrate diagnosable psychiatric disorders, a practice that delays intervention until symptoms are pronounced and severe, although mental health services have greater impact when they are delivered in the earlier stages of development of a disorder. Third, referral-based models concentrate mental health services on older children whose pathology has more fully developed, but numerous studies have shown that mental health services have more impact when they are delivered to younger children. Fourth, referral-based service models focus a community’s mental health resources on reducing pathology, but there is increasing evidence that the promotion of psychological wellness is just as important as the treatment of pathology, and that mental health service systems must attend simultaneously to pathology and wellness.
The ultimate intent of population-based mental health services is to leverage existing resources so that more children receive mental health services earlier and with more impact. Population-based services could be integrated most easily into community organizations that already serve all children (e.g., schools, churches, athletics, recreation centers, juvenile justice, and social services) and that share responsibility for children’s mental health services (Doll, 1996; Strein et al., 2003). Further, in most U.S. communities, there is convincing evidence that the services provided by the multiple agencies and providers responsible for children’s mental health duplicate and compete with one another and that children could be better served by a carefully coordinated system of mental health care such as that provided by population-based assessment (Adelman and Taylor, 2006).
Limitations to population-based services have also been identified. In practice, the model has only been implemented on a small scale and within communities that are already population-focused (e.g., schools, military bases, or public health systems.) Transitioning to a population-based model would represent a wholesale reorganization for community mental health systems and may not be practical given current health insurance funding mechanisms that reimburse clinics and private practitioners for treatment of identified disorders. Ironically, systems that are best poised to transition into population-based service delivery models in the United States are public agencies such as schools that were not traditionally vested with responsibility for children’s mental health.
Population-Based Approaches To Children’s Mental Health
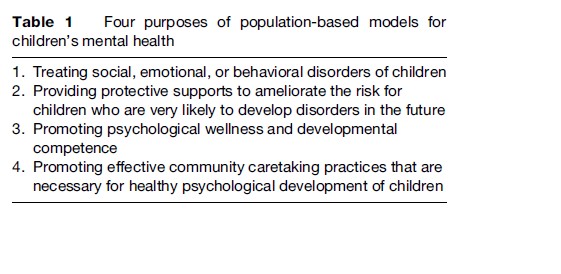
Planning for population-based services for children begins with an understanding of the nature of developmental competence and psychopathology, as derived from the rich developmental research describing children’s social, emotional, cognitive, and personal growth. Given what is known about children’s developmental competence in general, information is then gathered to describe the mental health needs of all children in a particular community. Based on that data-based portrait, resources with the potential to address these needs are identified. Collaborative partnerships that extend throughout the community can create infrastructures that integrate related interventions into comprehensive systems of care and that dismantle programmatic silos – narrowly construed interventions that address a single risk factor or disturbance without regard for children’s other risks or needs. Given the identified mental health needs and resources, a plan is constructed that prioritizes the needs of the community’s children and allocates mental health resources to interventions that are frequently needed and those that will have high impact on the children’s psychological wellness. Table 1 describes four primary purposes that guide these interventions. Periodic reassessment of children’s mental health needs allows community mental health providers to evaluate progress and update the mental health plan. Interventions that emerge out of this problem-solving cycle do not need to focus solely on children. They can also focus on the families, community groups, or agencies. Indeed, when population-based assessments suggest that large numbers of children are faltering, stronger caretaking systems are needed for children in the community.
Research On Developmental Competence And Psychopathology
Throughout most of the twentieth century, the principles and practices of children’s mental health services proceeded independently of the research on typical and atypical child development. In the past two decades, two previously distinct disciplines have merged – research on child development has increasingly examined the interventions that are necessary to shift developmental trajectories toward success, while research on children’s psychopathology has increasingly recognized the impact of natural caretaking systems on the expression of mental illness. Where the two disciplines intersect, important contributions have been made to the design of children’s mental health services, including: (1) examinations of the socioecological predictors of mental health and psychiatric disturbance in children and adolescents (with implications for the interruption of children’s developmental trajectory into psychopathology); and (2) descriptions of developmental differences in the nature and prevalence of psychiatric disorders (with implications for necessary shifts in the nature of mental health services at different age points).
One of the most impressive findings has been the degree to which children’s developmental competence and mental health is predicated on characteristics of the caretaking communities and families rather than the children themselves (Coie et al., 1993; Masten and Coatsworth, 1998). In particular, children’s exposure to poverty, family violence, parental mental illness, or community violence significantly increases their chances of developing debilitating mental illnesses. Consequently, reducing the prevalence of these deleterious factors in children’s communities has the potential to significantly reduce the need for children’s mental health services, and community-wide efforts to address demographic threats to children’s well-being must be incorporated into any population-based mental health service plan. Conversely, many protective factors that allow children to flourish despite adversity are also characteristics of their communities and families: Close bonds with alternative adults, friendships with peers, connections with prosocial organizations, and effective schools. The implication for a community’s mental health program is that some services that ameliorate children’s risk for psychopathology may lie outside the traditional boundaries of mental health services.
Mental health service plans must also be informed by the relatively recent information about the prevalence of mental illness in children and adolescents (Doll, 1996; Strein et al., 2003). Two important bodies of research are relevant here. First, epidemiological studies conducted in the United States in the 1980s and 1990s collected representative community samples of children and screened them for the major psychiatric disorders. Results demonstrated that anxiety disorders are surprisingly prevalent in children and adolescents, with one out of every five children meeting the DSM-IV criteria for one or more anxiety disorders. Prior to the studies, children’s mental health services had seriously underestimated the presence of anxiety disorders in this population and relative few services were provided for it. Other high-frequency psychiatric disorders of childhood and adolescence included disruptive behavior disorders (attention deficit hyperactivity disorder; conduct disorder; oppositional defiant disorder) and mood disorders (depression, bipolar disorder). In other cases, the epidemiological studies demonstrated that there were striking developmental differences in the prevalence of particular disorders. For example, the incidence of attention deficit hyperactivity disorder is more prevalent in preadolescent children, while the incidence of adolescent conduct disorders is at least twice that of preadolescent children and mood disorders are three to four times more prevalent in adolescents. Prevalence and incidence data in other countries may not replicate these figures from the United States because different diagnostic criteria may be used, and even within the United States demographic factors can alter the prevalence of disorders while differing sociocultural contexts can shift diagnostic practices. Thus community-based assessments need to be conducted prior to creating a population-based mental health service plan. Moreover, decisions about which mental health services are most needed by a community cannot be made by prevalence figures alone. Communities must also balance the severity and impact of any disorder, the likely impact of intervention services, and the need for wellness-promoting as well as disorder treatment services.
A second important source of information about the prevalence of children’s DSM-IV disorders in the United States is the National Comorbidity Survey Replication (Kessler et al., 2005). Through this nationwide epidemiological study, 9282 comprehensive clinical interviews were conducted to estimate the prevalence, severity, and comorbidity of DSM-IV disorders in participants aged 18 and older. Its findings have important implications for children. In particular, the study established that the average age of onset for most disorders is in the first two decades of life, and that the mean age of onset for anxiety disorders and impulse control disorders is around 11 years of age. Typically, efforts to secure treatment lagged 6–8 years after the onset of significant symptoms, suggesting that disorders may begin in childhood but often are not treated until early adulthood. Six out of ten cases that were identified through the survey were classified as severe or moderately severe and in immediate need of services. Combined with the earlier epidemiological studies assessing childhood prevalence, the National Comorbidity Survey Replication provides evidence of a profound discrepancy between the need for and availability of mental health services for children in the United States. Population-based mental health services will need innovative strategies and cooperation from multiple agencies and providers in order to bridge this gap.
Assessment Of The Collective Mental Health Status Of Children In The Community
While research has provided some hints about the nature and prevalence of mental health needs that are likely to exist for any single community, the specific array of service needs can shift and change. For example, community needs might change given major drops in adult employment, concentrations of poverty, geographic isolation that limits access to community support programs, or location adjacent to abusable substances or drug transportation routes. Consequently, the strongest population-based mental health services are predicated on data-based portraits gathered to describe children’s mental health needs in the immediate community. Data can include existing community data such as records of school behavior or youth crime or vandalism, particularly when monitoring systems have been put in place to collect these data meticulously and accurately.
Alternatively, using epidemiological survey protocols, children can be deliberately screened for evidence of mental health or psychopathology. In smaller communities, every child might be screened, but larger communities could use systematic sampling strategies to derive reliable estimates of the nature and extent of mental health needs. Epidemiological research has established standards for selecting community samples, screening for all instances of a disorder, confirming diagnoses against professional standards, identifying variables related to instances of the disorder, and using data to identify predictive and causal relations underlying useful intervention strategies (Short and Strein, 2008). Many epidemiological studies use multistage procedures in which the entire child population of a community is first screened to identify any evidence of a disorder. Measures used in this initial screening stage must minimize the number of false-negative identifications so that all children with legitimate need for services will be identified. In subsequent stages, more time-intensive measures are administered to children selected in the first stage and yield more comprehensive descriptions of their needs and strengths. Within research protocols, strict adherence to sound epidemiological methods are possible with sufficient funding. In practice, a pragmatic alternative is to carefully train key informants such as teachers or childcare workers in the primary symptoms of high-frequency disorders, and use these informants as a Stage 1 screening resource to refer children into a second time-intensive stage of screening.
Other assessments could be predicated on the developmental risk research, assessing the chronic stressors that place children at risk for limited personal and social success (Coie et al., 1993; Walker and Shinn, 2002). Community demographic data describing poverty, educational attainment, employment, rates of divorce, incidence of child abuse, or family health can be analyzed to provide useful estimates of the numbers of children growing up with three or more of these risk factors. Risk-based assessments can instead be based on functional risk or evidence of early symptoms of disorder that may not satisfy the diagnostic criteria for a DSM-IV disorder. Records of school discipline or suspension, truancy, status offenses, or youth vandalism can be used as evidence of emerging behavioral disorders that could impair children’s life success. Early identification using functional risk data makes it possible to address adjustment problems when they are first evidenced and, in some cases, to waylay eventual disorders. Many of the same developmental studies that described demographic risk factors also identified protective factors that predict future life success in vulnerable children and that could become the mechanisms underlying preventive interventions. Consequently, population-based assessment could also describe assets in a community’s children such as school success and achievement levels, and youth participation in community service activities and mentoring organizations.
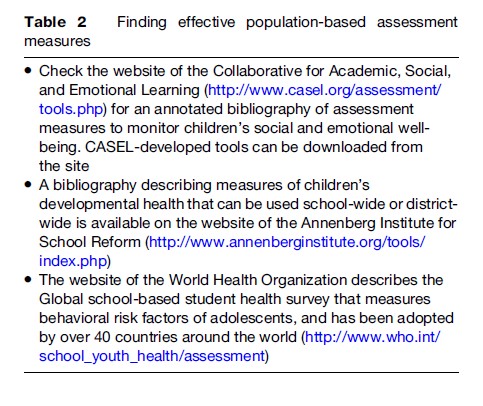
Pragmatic assessment strategies that are used for population-wide assessment may be very different from traditional diagnostic assessment measures. Population-wide assessments must be brief to administer and efficient to code and analyze, so that the task of creating the data-based portrait of children’s mental health needs does not overtax the community resources. The strategies must have strong reliability and validity, so that they are highly accurate in describing the mental health of a community’s children. Examples of strong measures for population-based assessments can be found in Table 2. Data might be aggregated across all children in a community, aggregated across subgroups of children (e.g., by age, gender, or risk factors), or used to identify specific children at high risk (Short and Strein, 2008). Patterns and trends in those data can suggest particular sources of risk, describe the nature of mental health interventions that are required, or make the case for additional interventions from within or outside the community. Effective community assessments will identify children who would have slipped through the cracks in traditional referral-based services, identify the children earlier than would otherwise be the case, and guide the planned development of services to match children’s needs. Thus, population-based assessments allow communities to be proactive rather than reactive in responding to children’ mental health needs.
A Plan For The Community’s Mental Health Services To Children
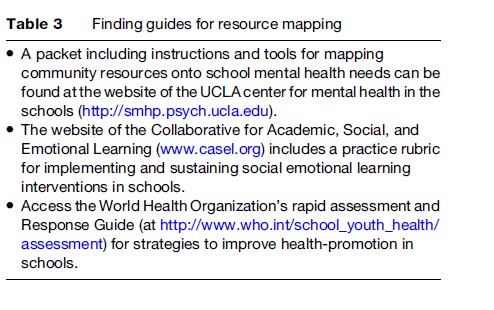
The purpose of the population-based service plan is to create a match between the mental health needs that have been identified in the community assessment and the services that are provided to children in the community. Resource mapping has been proposed as a coordinating framework for matching resources to the needs (Adelman and Taylor, 2006). Resource mapping begins by creating a comprehensive list of the community’s existing mental health programs and the mental health service providers who staff these programs, including how they spend their time, when and where they provide services to children, and the populations of children that they serve. The next step compares the community’s existing mental health services to current mental health needs of the children. Examples of resource maps to guide this comparison can be found in Table 3. Gaps exist when mental health needs are identified and no community services exist to meet those needs; duplication is identified when multiple services simultaneously and repeatedly address the same need.
Once the needed services are identified, mental health provider roles will be reframed to be highly responsive to those needs. Mental health needs that are demonstrated by large numbers of enrolled children (e.g., anxiety symptoms) may indicate that community-wide services would be appropriate. Alternatively, very significant needs may justify the provision of high-intensity mental health services even if these would only be needed by a very few children. In some cases, mental health service planning will document the need for new kinds of services that have not previously been provided. In other cases, community staff may decide that there are ecological factors that facilitate problems that could be addressed preventively. In still other instances, mental health service planning will incorporate services that have not traditionally been thought of as mental health services at all. In particular, the emphasis on family and community factors as causal agents for children’s mental illness raises important questions about who is responsible for children’ mental health and how healthy socioemotional development is promoted. An important component of this reframing process may be modifying existing policies to allow new ways for services to be combined and professionals to interact. In almost every case, the resulting plan will describe a continuum of mental health services extending from individual interventions for children with special needs, much like traditional clinical interventions, to community-wide interventions that address prevalent problems and promote developmental competence.
Population-Based Mental Health Intervention
The continuum of mental health services needed by most communities is likely to look very much like the fourtiered model of service similar to those of Walker and Shinn (2002) and Osher et al. (2004) (Figure 1). The continuum must address the universal mental health needs of children with community-wide services to promote psychological wellness and to prevent disturbance. Developmental resilience research offers important insights into the kinds of services that promote wellness. Specifically, children are resilient in the face of adversity when they have access to close peer friendships, high self-efficacy, high levels of engagement in productive activities, access to warm relationships and guidance from adults, or access to responsive community agencies. Additional examples of interventions that promote wellness can be found on the website of the Collaborative for Academic, Social, and Emotional Learning.
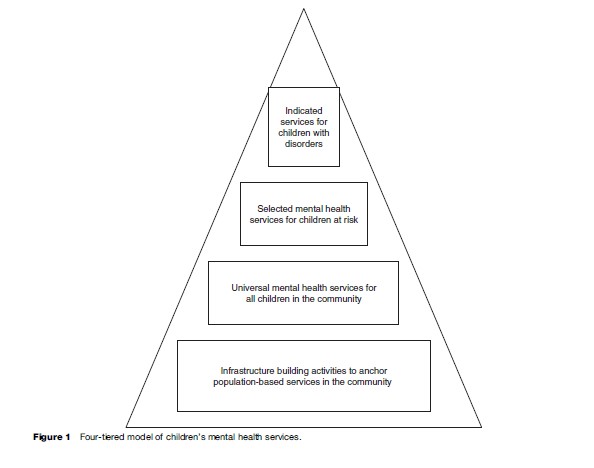
Selected mental health services will also need to be provided to identified children who are at high functional risk (i.e., early evidence of adjustment disturbances) or demographic risk (i.e., evidence of poverty, family violence, or other characteristics that predict poor outcomes). These services are more concentrated and more intense than universal services, address needs that are not broadly held by all children in a community, and have the purpose of strengthening competence as well as ameliorating risk. Because these interventions interrupt developmental risk trajectories, they have necessarily been interwoven with prevention services. The essential characteristics of effective prevention programs have been identified by Nation et al. (2003): They are a comprehensive integration of multiple interventions that are implemented across school, home, and community; they use varied and interactive teaching methods that actively engage children in developing specific skills; their dosage is matched to the problem severity with interventions that are more intense and of longer duration for more severe problems; they are theory-driven and evidence-based; and they promote strong, positive relationships between parents and children, teachers and children, and children and peers. Numerous examples of preventive interventions can be found on the website of the UCLA Center for Mental Health in the Schools.
In every community, a few children will require indicated services, necessary for children whose dysfunction is pronounced. These should be implementations of manualized interventions that have been subjected to rigorous research to demonstrate their effectiveness. Rigorous standards for evidence-based interventions with children assert that evidence-based interventions have been subjected to at least two well-designed group studies or a series of well conducted single-subject studies (Chambless and Hollon, 1998). Participants in the studies should have been randomly assigned to different intervention groups and comparisons should be made between groups of participants provided with no intervention, competing interventions, and with the intervention of interest. Finally, results should demonstrate that improvements are due to the intervention, represent an improvement over no intervention at all, and are at least as strong as those produced by competing interventions. Compendiums describing evidence-based interventions for children can be found in Christophersen and Mortweet (2001) and Kazdin and Weisz (2003).
Adelman and Taylor (2006) argue that infrastructure and planning should be a foundation of the intervention continuum. Before population-based interventions can be implemented, giving children and adolescents access to mental health services in proportion to their mental health needs, important systemic changes need to occur. Their volume provides a comprehensive description of the theory, research, and implementation underlying infrastructures for mental health services.
Evaluation Of Population-Based Services
Evaluation serves two important purposes within population-based service models: (1) To continually update information about the mental health status of children in the community, so that the program of services remains responsive to the needs of children; and (2) to monitor the impact of the population-based services on children’s mental health. Ideally, mental health service providers hope that the program will strengthen psychological wellness and diminish psychopathology among children in the community. Answering these questions is quite challenging. First, although it is possible to aggregate individual evaluation information across multiple children, time and cost constraints make it impossible to conduct comprehensive individual evaluations of all children participating in mental health services. Consequently, service providers must identify and target key indicators of children’s wellness from the beginning, weaving evaluation into the implementation of the program of services. Second, community level effects may be confounded with important psychosocial events that occur during the period of an evaluation. For example, the loss of a major employer in a small rural community can unexpectedly double or triple the parental unemployment rate, and the resulting family stress could be reflected in higher rates of childhood disturbance. Consequently, the evaluation plan must include qualitative records of important community events that serve as the context for services. Third, trends in children’s psychological wellness or psychopathology are likely to stretch across several years, well beyond the timeframe of a typical project year. Consequently, planning for and decisions about population-based mental health services must proactively monitor community indicators of mental health and psychological wellness across projects.
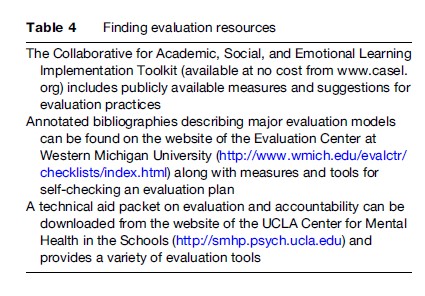
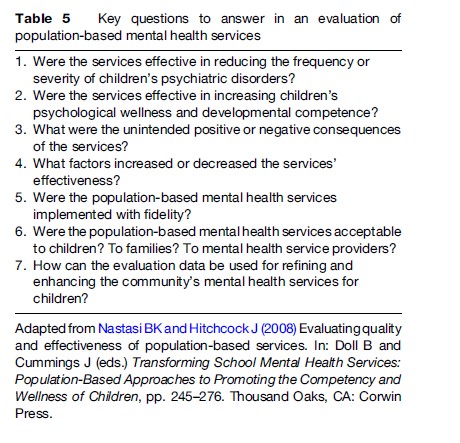
The most useful evaluation will be a formative evaluation that feeds continuous improvement information back to the program leaders, even while it is being implemented. The most effective evaluation is systematic with methodologically rigorous designs and not an anecdotal case study. Table 4 describes resources that guide the development of effective evaluations, are available online, and at very little cost. These resources reinforce the principle that good evaluation requires commonsense judgment as much as rigorous design and analysis. Key considerations in evaluation are described in Table 5 and include not only the degree to which the population-based mental health services were effective, but also the degree to which they were compatible with the needs and values of the community (Nastasi and Hitchcock, 2008). Particularly within population-based models, service providers and program planners will need to be diligent in monitoring the shared impact of services and decisions across all children in the community.
Summary
Population-based models for children’s mental health services are logical responses to the widespread dissatisfaction with traditional referral-based models for service delivery. Based on a public health perspective of mental health, they operationalize key principles of mental health intervention that have been demonstrated in empirical research on developmental competence and childhood psychopathology. They are extensions of the familiar Assess ! Plan ! Intervene ! Evaluate cycle that has been so useful for individually planned mental health services. However, the extension of this cycle to population-based decision making presents some special challenges. First, many of the community-wide assessment and intervention services do not fit neatly into existing service-funding options such as public or private health insurance. Second, important components of the community’s mental health services plan might rely on nontraditional providers of mental health services, such as youth mentorship programs, churches, or neighborhood community centers. Third, designing and implementing a population-based mental health program relies on collaboration across multiple community agencies – public and private – and it can be difficult for these agencies to communicate clearly and efficiently. Fourth, a shift from a traditional mental health model to population-based services will almost always be made in the face of diminishing or at best flat child mental health resources. As a result, population-based planning typically requires a reallocation of resources from previous services to new services, and may create what may be seen as winners and losers within the community. Clearly, a shift to population-based mental health services cannot be made around the edges of traditional services. The strategies require considerable time up front in order to plan, deliver, and evaluate the community-wide interventions. At a minimum, this will require that communities thoughtfully and carefully plan for the nature and amount of mental health services that they will provide to children.
Bibliography:
- Adelman HS and Taylor L (2006) The School Leader’s Guide to Student Learning Supports: New Directions for Addressing Barriers to Learning. Thousand Oaks, CA: Corwin Press.
- American Psychiatric Association (2000) The Diagnostic and Statistical Manual of Mental Disorders, 4th edn., Text Revision. Washington, DC: American Psychiatric Association.
- Chambless DL and Hollon DS (1998) Defining empirically supported therapies. Journal of Consulting and Clinical Psychology 66: 7–18.
- Christophersen ER and Mortweet SL (2001) Treatments That Work with Children: Empirically Supported Strategies for Managing Childhood Problems. Washington, DC: American Psychological Association.
- Coie JD, Watt NF, West SG, et al. (1993) The science of prevention: A conceptual framework and some directions for a national research program. American Psychologist 48: 1013–1022.
- Doll B (1996) Prevalence of psychiatric disorders in children and youth: An agenda for advocacy by school psychology. School Psychology Quarterly 11: 20–46.
- Kazdin AE and Weisz JR (2003) Evidence-Based Psychotherapies for Children and Adolescents. New York: The Guilford Press.
- Kessler RC, Berglund P, Demler O, Jin R, and Walters EE (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry 62: 617–627.
- Masten AS and Coatsworth JD (1998) The development of competence in favorable and unfavorable environments: Lessons from research on successful children. American Psychologist 53: 205–220.
- Nastasi BK and Hitchcock J (2008) Evaluating quality and effectiveness of population-based services. In: Doll B and Cummings J (eds.) Transforming School Mental Health Services: Population-Based Approaches to Promoting the Competency and Wellness of Children, pp. 245–276. Thousand Oaks, CA: Corwin Press.
- Nation M, Crusto C, Wandersman A, et al. (2003) What works in prevention: Principles of effective prevention programs. American Psychologist 58: 449–456.
- Osher D, Dwyer K, and Jackson S (2004) Safe, Supportive, and Successful Schools: Step by Step. Longmont, CO: Sopris Press.
- Short R and Strein W (2008) Social and behavioral epidemiology: Population-based problem identification and monitoring. In: Doll B and Cummings J (eds.) Transforming School Mental Health Services: Population-Based Approaches to Promoting the Competency and Wellness of Children, pp. 23–42. Thousand Oaks, CA: Corwin Press.
- Strein W, Hoagwood K, and Cohn A (2003) School psychology: A public health perspective. I. Prevention, populations, and systems change. Journal of School Psychology 41: 23–38.
- Walker HM and Shinn MR (2002) Structuring school-based interventions to achieve integrated primary, secondary, and tertiary prevention goals for safe and effective schools. In: Shinn MA, Walker HM, and Stoner G (eds.) Interventions for Academic and Behavior Problems II: Preventive and Remedial Approaches, pp. 1–26. Bethesda, MD: National Association of School Psychologists.
- Doll B and Cummings J (2008) Transforming School Mental Health Services: Population-Based Approaches to Promoting the Competency and Wellness of Children. Thousand Oaks, CA: Corwin Press.
- Nastasi BK (2004) Meeting the challenges of the future: Integrating public health and public education for mental health promotion. Journal of Educational and Psychological Consultation 15: 295–312.
- http://www.annenberginstitute.org/tools/index.php – Annenberg Institute for School Reform, bibliography describing measures of children’s developmental health that can be used school-wide or district-wide.
- http://www.casel.org – Collaborative for Academic, Social and Emotional Learning; annotated bibliography of assessment measures to monitor children’s social and emotional well-being. CASEL-developed tools; includes a practice rubric for implementing and sustaining social emotional learning interventions in schools.
- http://www.wmich.edu/evalctr – Evaluation Center at Western Michigan University.
- http://smhp.psych.ucla.edu – UCLA Center for Mental Health in Schools; A packet including instructions and tools for mapping community resources onto school mental health needs.
- http://www.who.int/school_youth_health/assessment – Resources and tools for assessment and monitoring, World Health Organization; describes the global school-based student health survey that measures behavioral risk factors of adolescents, and has been adopted by over 40 countries around the world; strategies to improve health-promotion in schools.
- http://www.who.int/school_youth_health/assessment – World Health Organization’s Rapid Assessment and Response Guide for strategies to improve health-promotion in schools.




