Sample Eating Disorders Research Paper. Browse other research paper examples and check the list of research paper topics for more inspiration. iResearchNet offers academic assignment help for students all over the world: writing from scratch, editing, proofreading, problem solving, from essays to dissertations, from humanities to STEM. We offer full confidentiality, safe payment, originality, and money-back guarantee. Secure your academic success with our risk-free services.
The current system of psychiatric classification, the Diagnostic and Statistical Manual of Mental Disorders–Fourth Edition (DSM-IV; American Psychiatric Association [APA], 1994), includes two official eating disorder (ED) syndromes: anorexia nervosa and bulimia nervosa, and a third (still provisional) diagnosis, binge-eating disorder. Binge-eating disorder, however, is likely to become officially recognized in future editions of the diagnostic manual and we therefore include it in this research paper. Anorexia, bulimia, and binge eating are polysymptomatic syndromes, defined by maladaptive attitudes and behaviors around eating, weight, and body image, including as well nonspecific disturbances of self-image, mood, impulse regulation, and interpersonal functioning. In this research paper, we review pathognomonic features of the EDs and findings on concurrent traits and comorbid psychopathology. We also discuss the putative set of factors, biological, psychological, and social (as well as eating-specific and more generalized) that may explain ED development.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
Defining Characteristics
Anorexia Nervosa
Anorexia nervosa (AN) is defined by a relentless pursuit of thinness and a morbid fear of the consequences of eating (usually expressed as a dread of weight gain or obesity). The result is a willful (and often dramatic) restriction of food intake. The person with AN imposes upon herself a state of gradual weight loss and (sometimes) dangerous emaciation. (Recognizing different proportions of EDs among females and males, we use feminine personal pronouns. This convention is not intended to disregard eating syndromes in males.) At the core of such behavior appears to be a literal phobia of weight gain, so intense that the individual avoids behaviors (e.g., eating unfamiliar foods, eating without exercising) that could lead to weight gain and thus incrementally loses further weight.
Individuals with AN typically eat a restricted range of safe (usually low-calorie) foods or avoid social eating situations so that they will have full control over what, how much, and in what way they can eat. In some cases, anorexics purge after eating through vomiting, misuse of laxatives, or other means, due to fears that they may have overeaten. About half of sufferers eventually develop binge-eating episodes—that is, periodic dyscontrol over eating, or incapacity to satiate (DaCosta & Halmi, 1992). Consequently, a distinction is usually made between AN, restricting subtype, in which the sufferer limits food intake but does not engage in binge eating or purging (i.e., self-induced vomiting; misuse of laxatives, diuretics, or enemas), and AN, binge-eating/purging subtype, in which (as the label implies) binge or purge episodes are prominent.
Bulimia Nervosa
In apparent contrast to AN, the main feature of bulimia nervosa (BN) is binge eating (i.e., appetitive dyscontrol, vs. AN’s overcontrol). Bulimia nervosa is diagnosed in relatively normal or overweight individuals (not anorexics) who display recurrent eating binges, and who then compensate for overeating through self-induced vomiting, laxative misuse, intensive exercise, fasting, or other means. It is the combination of binge eating and compensation that define BN and that differentiates it from an apparently related syndrome, binge-eating disorder (which we will introduce shortly). In BN, binges are characterized by consumption, with a terrifying sense of dyscontrol, of sometimes massive quantities of calories. Binges can provoke profound feelings of shame, anxiety, or depression, and the bulimic’s sense of self-worth and well-being often shifts quite dramatically in concert with her sense of control around eating and body image. This lends to BN a characteristic unpredictability or lability, as people with this syndrome will shift rapidly (depending upon felt control over eating) from a sense of well-being, expansiveness, or excitability, to profound despair, irritability, and depression. Although the validity of BN as a unique diagnostic category seems well supported (Gleaves, Lowe, Snow, Green, & Murphy-Eberenz, 2000), the distinction (in DSM-IV criteria) between purging and nonpurging bulimic subtypes may be of dubious merit in identifying truly different populations of sufferers (Tobin, Griffing, & Griffing, 1997).
Binge-Eating Disorder and Eating Disorders Not Otherwise Specified
Other variations on EDs occur, classified in the DSM-IV system as eating disorder not otherwise specified (EDNOS). For example, anorexic-like weight preoccupations and pursuit of thinness in individuals who retain menses, are given the diagnosis of EDNOS. Most important of the EDNOS variants is, however, an apparently quite prevalent pattern characterized by recurrent eating binges in the absence of compensatory behaviors such as vomiting or fasting. This pattern, which (eventually) renders the sufferer overweight, is currently labeled binge-eating disorder (BED). According to provisional criteria, defining characteristics include eating more rapidly than normal, eating until uncomfortably full, eating when not hungry, eating alone due to embarrassment around the quantity one eats, or feeling intense guilt, disgust, or depression after eating. In BED, binge episodes must be markedly distressing.
Compared to individuals with BN, BED patients are noted to binge over considerably longer periods of time (Fairburn, 1995), with individuals in some cases showing day-long binges. Eating in individuals with BED is noted to have a less desperate or driven character than in BN, and BED patients apparently consume more proteins than do bulimics, who preferentially binge on sweets or carbohydrates (Fitzgibbon & Blackman, 2000). In addition, BED subjects are reportedly more likely than bulimics to find the food on which they binge soothing or relaxing (Mitchell et al., 1999).
There has been controversy surrounding the BED diagnosis—a concern being that BED may not isolate a truly psychological or behavioral disturbance. However, data show obese people with BED to have more fear of weight gain, more body dissatisfaction, more problems of self-esteem and dysphoric mood, and poorer maintenance of weight loss (once achieved) than do non-BED obese people (Marcus, Wing, & Hopkins, 1988; Streigel-Moore, Wilson, Wilfley, Elder, & Brownell, 1998).Also lending credence to the validity of BED as a unique entity, data indicate taxonomic and genetic distinctiveness of the syndrome. A latent-class analysis applied in a large cohort of female twins (N = 2,163) identified a distinct BED syndrome and showed greater resemblance for the syndrome among monozygotic versus dizygotic twins (Bulik, Sullivan, & Kendler, 1998).
The Restrictor-Binger Distinction
A distinction between restrictors (those anorexic patients who restrict food intake without binging and purging) and bingers (those ED patients, sometimes anorexic, sometimes bulimic, sometimes obese, who binge and purge) has been introduced by various theorists as an alternative to the formal anorexic-bulimic distinction (see DaCosta & Halmi, 1992). The restrictor-binger distinction has been thought to correspond to important phenomenological and etiological differences, including differences as to key personality features, family interaction styles, and associations with biological processes (all will be reviewed presently).
Where relevant, throughout this research paper, we will address and clarify the rationale for the restrictor-binger distinction concept.
Epidemiology
Anorexia nervosa and bulimia nervosa occur disproportionately, often in industrialized (vs. economically less developed) nations, but are otherwise reported to occur with surprisingly uniform prevalences in developed parts of Europe, Asia, and the Americas. Reported prevalences in school-aged females of strictly defined AN generally fall in the 0.5% to 1% range (Wakeling, 1996), and of BN generally in the 1% to 2% range (e.g., Garfinkel et al., 1995). However, it is probably fair to assume that in subthreshold forms, identified using less stringent diagnostic criteria, EDs occur in larger numbers (Garfinkel et al.). At least 10% of school-aged females in the industrialized world display partial anorexic or bulimic syndromes, associated with significant dietary, psychological, and medical distress.
Although a popular stereotype is the young adolescent AN sufferer, actual peak prevalences of EDs are observed in young adult women, reflecting the (unfortunate) tendency of EDs to run a chronic course and of BN to develop later in the life cycle (during the transition to adulthood). Although they occur about one-tenth as often in men as in women, classical anorexic and bulimic syndromes are also noted in males (e.g., Wakeling, 1996) and there are some indications to suggest that if ED prevalences are rising in any group, it is doing so especially among males. Eating disorders appear to occur less frequently in certain racial and ethnic groups, for example, among Black andAsian-AmericanversusWhitefemales(Crago,Shisslak,& Estes, 1996). A comparison of White, Hispanic, and Black adolescent females, both athletic (N 571) and nonathletic (N 463), for example, showed reliably lower rates of disordered eating in both of the Black female groups, compared to those obtained in White and Hispanic groups (Rhea, 1999). However, some findings suggest that Black women may yet be especially susceptible to certain aspects of eating disturbance: For example, a telephone-interview survey involving 1,628 Black and 5,741 White urban women found Blacks to report more fasting, abuse of laxatives or diuretics, and highfrequency binge eating than did the White women (StriegelMoore,Wilfley, Pike, Dohm, & Fairburn, 2000).
Although changes in diagnostic and record-keeping practices make it difficult to pin the issue down, evidence suggests an increasing ED incidence (Wakeling, 1996). Reviewing annual incidence rates for AN in the United States published between the early 1960s and the mid-1980s, Mitchell and Eckert (1987) concluded that there had been a progressive increase, from 0.35 to 4.06 per 100,000. Similarly, an incidence study in the Rochester, Minnesota, area concluded, after screening 2,806 medical records for new cases of AN, that there had been a long-term increase in AN, especially among 15- to 24-year-old females (Lucas, Crowson, O’Fallon, & Melton, 1999). In a similar vein, it is commonly believed that EDs are disorders of affluent, urban society. However, current data show surprisingly limited linkage to upper socioeconomic status, and unexpectedly high numbers of EDs found in rural communities suggest that EDs may not be as much an urban phenomenon as may once have been believed (Gard & Freeman, 1996).
Only limited epidemiological data are available for BED, given its more recent addition to the diagnostic nomenclature. Nonetheless, studies suggest a disturbingly common syndrome that may affect from 1% to 5% of the general population and about 8% of the population of obese people. In selected subgroups, such as obese people undergoing weight-loss treatment, BED prevalences apparently run as high as 30–50% (Spitzer et al., 1992). Intriguingly, data show BED to have a more even gender-based distribution than do other EDs, probably affecting 2 males for every 3 females (Streigel-Moore et al., 1998), and to affect a broader age group, with peak age being about 40 years, compared to 28 years for BN (Fitzgibbon & Blackman, 2000). Bingeeating disorder, therefore, seems to be less gender and age dependent than either AN or BN.
Comorbidity with Other Psychopathology
Paradoxically, it seems that if one assertion can be made about EDs, it is that they are not only about eating. Rather, EDs frequently co-occur with other forms of psychopathology, for example, mood, anxiety, substance-abuse, posttraumatic stress, and personality disorders.
Mood Disorders
Among comorbid tendencies noted in ED sufferers, comorbid mood disorders figure very prominently. Råstam (1992) reported a 40% rate for currently comorbid major depression in her anorexic sample, a 70% rate for overall mood disorders, and a rate of lifetime mood disorder in excess of 90%. A comparable, or perhaps even more pronounced, tendency toward comorbid mood disorder is noted in binge-purge syndromes. One study, comparing point prevalences of major depression across restricting and binging-purging anorexics, noted the disorder in about 30% of restrictors and in 53% of binger-purgers (Herzog, Keller, Sacks, Yeh, & Lavori, 1992). Other investigations have suggested that from 20% to more than 40% of bulimics are clinically depressed (Brewerton et al., 1995; Garfinkel et al., 1995).
Co-aggregation with other mood-disorder variants is also apparently considerable. A community study by Zaider, Johnson, and Cockell (2000) points to an important affinity between EDs and dysthymia, a milder chronic mood disturbance. In addition, evidence has shown a strong association of BN with seasonal affective disorder (SAD), implying cyclical season-dependent recurrences in depressed mood. In one study, 69% of BN patients were noted to show comorbid SAD (Levitan, Kaplan, Levitt, & Joffe, 1994). Furthermore, a study by our group demonstrated stronger SAD comorbidity in bulimic rather than anorexic ED variants. In a sample of 259 patients presenting at our specialized ED clinic, 27.0% were rated as showing SAD—71.4% diagnosed with BN, 18.6% with AN, and 10.0% with EDNOS (Ghadirian, Marini, Jabalpurlawa, & Steiger, 1999).
Various areas of etiological overlap can be postulated to explain eating disorder–mood disorder convergence. Both syndromes are believed to depend upon similar familial or developmental substrates (e.g., developmental neglect or familial overprotection), and both have been thought to have similar neurobiological substrates. Pertinent to questions of shared causality, a genetic-epidemiological study by Wade, Bulik, Neale, and Kendler (2000), involving 850 female twin pairs indicates that both genetic and environmental factors contribute significantly to shared risk for AN and major depression. Given the implication of serotonergic factors in mood disorders in general and in seasonality in particular, there is ample potential for serotonin-mediated crossover of risk for BN, mood disorders, and SAD—a notion that has been partially corroborated by findings showing serotonin abnormalities to be more pronounced in BN patients with a seasonal profile (Levitan et al., 1997).
Anxiety Disorders
Anxiety disorders in AN reportedly vary from 20% (Herzog et al., 1992) to more than 80% (Godart, Flament, Lecrubier, & Jeammet, 2000), and reported rates in BN vary from 13% (Herzog et al.) to about 60% (Garfinkel et al., 1995). Godart and colleagues reported 83% of persons with AN and 71% of those with BN to have at least one lifetime anxiety-disorder diagnosis. Most common among the conditions they studied was social phobia (present in 55% of anorexics and 59% of bulimics).
Although studies report generalized anxiety disorder, social and simple phobias, agoraphobia, panic disorder, and obsessive compulsive disorder (OCD) in the EDs, we pay particular attention to data on the convergence between OCD and the EDs. This is because the structure of the EDs so closely resembles that of OCD—intrusive obsessions with weight and body image that are appeased by apparently compulsive gestures, such as fasting or purging. Lifetime prevalences of OCD are reported to range from 15% to 70% in anorexics, and from 3% to 30% in bulimics. Thornton and Russell (1997) reported that OCD was more prevalent in 35 women with AN (27%) than in 33 women with BN (3%), suggesting stronger co-aggregation of OCD with anorexic ED variants. Arguing for a specific affinity, one study indicated that obsessive-compulsive symptoms in adolescent anorexics are more common than are depressive symptoms (Cassidy, Allsopp, & Williams, 1999). Arguing that OCD characteristics may constitute an equally common (and apparently stable) trait in those susceptible to BN, von Ranson, Kaye, Weltzin, Rao, and Matsunaga (1999) found scores measuring OCD to be higher in 31 active bulimics and 29 recovered bulimics (abstinent for more than 1 year) than in 19 healthy comparison women, with scores on measures of symmetry and exactness being as abnormal in recovered bulimics as they were in active cases.
Various additional studies have examined the temporal sequence of onset for anxiety and eating syndromes, testing the idea that in vulnerable individuals, EDs actually may evolve from anxiety disorders. Thornton and Russell (1997) and Godart et al. (2000) both concluded that anxiety disorders often precede ED onset, implying that an anxious (and often obsessive-compulsive) disposition predisposes to ED development—or may be a manifestation of an incipient ED.
Substance-Abuse Disorders
Studies consistently indicate bulimic ED variants to be more strongly associated with alcohol and chemical dependencies than is the AN-restrictive type (see Holderness, BrooksGunn, & Warren, 1994). Relevant findings show from 10% to 55% of women with BN to abuse substances, whereas from 25% to 40% of females with alcohol dependence show some form of (often bulimia-spectrum) ED. Schuckit and colleagues (1996) found BN, but not AN, to occur at a greaterthan-expected rate among alcoholic women. Corroborating the impression of syndrome-specific aggregation, a study implicating 1,031 adolescent girls and 888 adolescent boys showed binge eating, especially when associated with compensatory weight-control behaviors, to coincide with elevated substance abuse (Ross & Ivis, 1999). Not surprisingly, studies examining psychopathological implications of substance abuse in the EDs report that concurrent substance abuse predicts greater comorbidity. Lilenfeld and colleagues (1997), for example, found substance abusers in an eating disordered population to show significantly more social phobia, panic disorder, and personality disorders.
Holderness and colleagues (1994) discuss sources for etiological overlap between bulimic ED variants and substanceabuse disorders. A so-called addictive personality (one prone to misuse of substances) has been postulated to underlie both types of syndromes, but evidence of such a personality style is unconvincing. It remains viable to consider shared biological substrates underlying substance-abuse and binge-eating behaviors, mediated by shared genetic diathesis, or shared factors related to serotonin, endorphin, or other neurotransmitters or neurohormones.
Posttraumatic and Dissociative Disorders
Eating disorders are, in an alarming proportion of cases, associated with adverse (potentially traumatic) life experiences (Everill & Waller, 1995; Wonderlich, Brewerton, Jocic, Dansky, & Abbott, 1997)—a link that we discuss more fully in a later section on developmental factors. Consistent with such observations, findings have suggested a remarkable coincidence between EDs and posttraumatic stress disorder (PTSD). One study reported PTSD in about half of 294 women with AN, BN, or EDNOS (Gleaves, Eberenz, & May, 1998). Severity of PTSD, however, was not found to predict subtype or severity of ED symptoms, suggesting that trauma (and associated posttraumatic stress) may not specifically control eating symptoms. On a related theme, there is a sizable body of data addressing the connection between EDs and dissociative disorders. Characterized by disturbances in memory (e.g., amnesias), consciousness (e.g., problems of identity, or apparent fragmentation of the personality), and sensorimotor function (e.g., conversion-type symptoms), dissociative disorders are sometimes regarded as failed adaptive responses to traumatic stress. Applying the dissociative-disorder concept to EDs, several groups have noted that individuals with BN and BED both produce elevations, relative to normal subjects, psychiatric comparison subjects, and restrictor anorexics, on validated self-report instruments measuring dissociation (e.g., Vanderlinden,Vandereycken, van Dyk, &Vertommen, 1993). Likewise, one study reported that 29 obese women with BED showed significantly more dissociative symptoms on a selfreport questionnaire, and more traumatic experiences, than did 35 obese women with no binge-eating symptoms (Grave, Oliosi, Todisco, & Vanderlinden, 1997).
Although evidence suggests a link between dissociative phenomena and bulimic symptoms, the extent to which dissociative symptoms correspond to binge eating, per se, or to general psychopathological indicators that (only incidentally) co-occur with bulimic eating problems, remains to be established. Various relevant studies suggest that dissociation coincides more closely with nonspecific than eating-specific components of psychopathology in ED patients. For example, a study by Gleaves and Eberenz (1995) linked dissociative symptoms more closely to severity of anxiety and depressive symptoms than to bulimic or anorexic symptoms in 53 ED patients. Similarly, Demitrack, Putnam, Brewerton, Brandt, and Gold (1990) concluded that the propensity toward self-mutilation in BN patients is linked more strongly to dissociative pathology than to severity of eating symptoms. In contrast, indicating some degree of specificity in the dissociative disorder–eating disorder connection, Everill, Waller, and Macdonald (1995) found self-reported dissociation, and especially the style of absorption (e.g., daydreaming), to predict frequency of binging in 26 clinical BN sufferers; whereas Katz and Gleaves (1996), studying 52 females diagnosed as having either an ED with dissociation, ED alone, dissociation alone, or neither condition, found that even those ED patients who showed no comorbid dissociative disorder tended to display dissociative-spectrum psychopathology.
Various pathways might account for an etiological link, direct or indirect, between the EDs and traumatic events. Where traumata impact directly upon the body, intuition leads to consideration of relatively direct effects acting upon bodily experience, and in turn upon eating and weight-control behaviors. Alternatively, abusive experiences might impact upon regulation of self, mood, and impulse, and in these ways indirectly heighten the risk of maladaptive eating behavior or moderate the intensity of eating symptoms such as binging or purging. Full discussions of direct and indirect pathways thought to link trauma and EDs are available elsewhere (see Everill & Waller, 1995; Wonderlich et al., 1997). Our group has documented a tendency for more severely abused bulimics to show greater abnormalities on indices reflecting serotonin and cortisol function (Steiger, Gauvin, et al., 2001). Such results could imply neurobiological factors, associated with childhood abuse, that could heighten the risk of overreactivity to stress and of self- and appetitive dysregulation.
Personality Disorders
Among various comorbid propensities in the EDs, that with personality disorders is arguably the strongest (see Vitousek & Manke, 1994). A recent meta-analysis (Rosenvinge, Martinussen, & Ostensen, 2000) of 28 studies on this area of comorbidity represents well the general tendencies in findings. In particular, Rosenvinge and colleagues found a higher proportion (58%) of eating-disordered than of comparison women (28%) to have a personality disorder. Furthermore, whereasAN and BN patients were found to show comparable likelihood of DSM Cluster-C (anxious-fearful) personality disorders (45% and 44%, respectively), BN patients showed higher proportions of Cluster-B (dramatic-erratic) personality disorders (44% overall) and of borderline personality disorder (31%) than did AN patients or controls. Such findings are representative of themes noted in earlier reviews: Personality disorders are frequently present in anorexic and bulimic syndromes, and results imply differential co-aggregation of personality-disorder subtypes with restrictive and bulimic ED variants. Restrictive AN seems to be associated with a high concentration of anxious-fearful personality-disorder diagnoses (characterized by anxiousness, orderliness, introversion, and preference for sameness and control). Eatingdisorder variants characterized by binge-purge symptoms coincide with more heterogeneous personality-disorder subtypes than do restrictive forms, and more importantly, with more pronounced affinity for the dramatic-erratic personality disorders (characterized by prominent attention and sensation seeking, extraversion, mood lability, and proneness to excitability or impulsivity). In other words, the dietary overcontrol that characterizes restrictive AN seems to be paralleled by generalized overcontrol, as a personality or adaptive style, whereas the dietary dyscontrol that characterizes binge-purge syndromes seems, in many cases, to be paralleled by generalized dyscontrol.
Malnutrition can have adverse effects upon personality functioning (Keys, Brozek, Henschel, Mickelson, & Taylor, 1950).This raises the concern that apparent personality disturbances seen in ED sufferers (and, in turn, personality-disorder diagnoses) may reflect state disturbances associated with an active ED rather than trait tendencies. In other words, caution around the use of personality-disorder diagnoses in active ED patients is warranted. Nonetheless, various findings associate the EDs with stable underlying personality disturbances. One investigation reports 26% of women recovered from AN or BN to show some form of ongoing personality disorder, with Cluster-B personality disorders’being more closely associated with bulimic subtypes (Matsaunaga, Kaye, et al., 2000). Another study, comparing 51 weight-restored adolescent-onset anorexics to 51 matched comparison cases, concluded that anorexics often show persistent obsessions, compulsions, and social-interaction problems (Nilsson, Gillberg, Gillberg, & Råstam, 1999).
Etiology
Contemporary etiological theory on the EDs invokes a multidimensional, biopsychosocial causality (Garfinkel & Garner, 1982; Striegel-Moore, Silberstein, & Rodin, 1986). In general form, such theory postulates that EDs implicate a collision among biological factors (e.g., heritable influences on mood, temperament, and impulse controls), social pressures (promoting body-consciousness or generalized selfdefinition problems), psychological tendencies (autonomy disturbances, perfectionism, preference for order and control, hypersensitivity to social approval), and developmental processes (conducive to self-image or adjustment problems). In the following sections, we review evidence pertaining to biological, psychological, and social factors that may act in ED development.
Psychological Factors
Developmental Theories
Psychological theories on ED development are very diverse. However, there is some consensus concerning convergence of psychological characteristics, developmental dynamics, and ED variants. Restrictive AN has been widely associated with traits of compliance and anxiousness in individuals who gravitate to orderliness or control, whereas bulimic subtypes of EDs (including AN, binge-purge subtype) have been linked to self-regulatory deficits, dramatic fluctuations in self-concept, and erratic efforts to regulate inner tensions. Early psychodynamic models interpreted anorexic symptoms as a defense against conflicting drives (e.g., sexual drives); eating was thought to invoke forbidden sexual fantasies, and food refusal to reduce associated anxiety (e.g., Waller, Kaufman, & Deutsch, 1940). Crisp (1980), in a related vein, formulated AN as a phobic-avoidance response, reinforced by a literal escape from maturational changes at puberty. In her conceptualization, Bruch (1973) emphasized maternal overinvolvement and failure to respond appropriately to the child’s self-affirming behaviors, believing such parenting problems to underlie autonomy deficits and pervasive feelings of ineffectiveness on the child’s part. Strober’s (1991) organismic-developmental paradigm again addressed pathological adaptations to adolescence, but emphasized an incompatibility between developmental imperatives surrounding puberty and a heritable temperament characterized by harm-avoidance, hyperreactivity to social approval, and preference for sameness. Related theories regard food refusal as a gesture of self-assertion, mounted by some children in the face of excessive familial controls or emotional overinvestment; in other words, as an adaptation to familial intrusions and overprotectiveness (e.g., Humphrey, 1991; Johnson, 1991).
From a developmental perspective, bulimic ED variants have been thought to be linked to family-wide interaction patterns tinged with greater hostility, neglect, criticism, rejection, and blaming (Humphrey, 1991; Johnson, 1991). For example, Johnson linked bulimic symptoms to parental neglect, in his view spanning a continuum from nonmalevolent forms (in families in which parents’ perfectionistic needs place excessive demands upon children) to malevolent forms (occurring in frankly chaotic or abusive families). Humphrey referred to family-wide deficits in nurturance and tension regulation and systems that ensnare members in mutually destructive, hostile, blaming projections. In both views, bulimic behaviors are conceived to play self- and mood-regulatory functions and to be metaphors for chaotic family interactions, tinged with desperate attempts to achieve closeness and hostile rejections.
Empirical Findings: Individual Psychological Characteristics
Empirical findings on personality and on cognitive and emotional functioning in individuals with EDs provide qualified support for tendencies outlined previously in the theoretical accounts.
Personality Characteristics. Early psychometric studies showed anorexic patients to be neurotic, socially anxious, and often depressed (Sohlberg & Strober, 1994). In addition, various findings pointed to a systematic co-aggregation between restrictor and binger-purger subtypes (on the one hand) and personality traits with an overcontrolled or dyscontrolled style (on the other)—the binger-purgers’being noted to show greater emotional lability, impulsivity, or oppositionality than the restrictors, and lesser extraversion and novelty seeking (risk taking). The same concept is reiterated, although imperfectly, in various contemporary studies. Findings with the Millon Clinical Multiaxial Inventory have, for example, suggested more schizoid or avoidant tendencies among restrictors and more histrionic tendencies among normal- or anorexic-weight bingers (Norman, Blais, & Herzog, 1993). With the Multidimensional Personality Questionnaire, Casper, Hedeker, and McClough (1992) found normal-weight bulimics to be less conforming and more impulsive than were either restrictor or binger-purger anorexics, but found the restrictors to show the greatest self-control, conscientiousness, and emotional inhibition. With the Tridimensional Personality Questionnaire, Bulik, Sullivan, Weltzin, and Kaye (1995) found normal-weight bulimics to be more novelty seeking than restrictor or binger anorexics, and restrictor anorexics to be more reward dependent than bulimic anorexics, but bulimic anorexics to be more harm avoidant than restrictors.
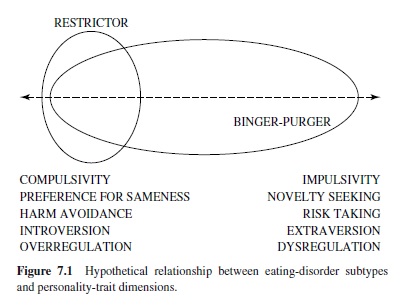
Taken together, available findings seem to support two theoretically important generalizations (seen also in data reviewed earlier on comorbid personality disorders): (a) Restrictive AN is associated with relatively circumscribed personality characteristics, with particular emphasis on traits of rigidity, emotional constriction, and compulsivity. (b) Binge-purge syndromes, on the other hand, are associated with relatively heterogeneous psychopathological characteristics that sometimes implicate greater behavioral disinhibition and affectivity. We illustrate this combination of tendencies in Figure 7.1, making the assumption that overcontrol and dyscontrol can be regarded as spanning a continuum along various theoretically related dimensions (e.g., compulsivity vs. impulsivity; preference for sameness vs. novelty seeking; introversion vs. extroversion; etc.). The figure depicts a tendency for there to be a circumscribed convergence, inrestrictive ED variants, of overcontrolled tendencies, but greater heterogeneity as to characteristics in bulimic (binge-purge) variants. Some bulimic cases show overcontrol, as has been associated with restrictive AN, but many others show marked erraticism and dyscontrol. Given trait heterogeneity among bulimics, theorists have proposed the existence of multiple pathways to bulimic eating disturbances, with some individuals being vulnerable due to underlying dysregulatory processes that manifest themselves in the form of mood and impulse dysregulation. What is believed is that, in some individuals, processes that correspond to generalized behavioral disinhibition may also underlie appetitive dysregulation (seeVitousek & Manke, 1994).
Specific Traits of Importance. Clinical observations consistently associate AN with specific personality traits, including perfectionism and impulsivity. For example, one study reported 322 anorexic women (restrictors and bingerpurgers alike) to have higher Multidimensional Perfectionism Scale scores than do 44 healthy control women, and notes a coincidence between degree of perfectionism and severity of eating symptomatology (Halmi et al., 2000). Perfectionism is also noted to be elevated in BN probands and their relatives (Lilenfeld et al., 2000), but not in individuals with BED (Fairburn et al., 1998). In addition, data show perfectionism to be evident in AN after long-term weight recovery (Srinivasagam et al., 1995), suggesting that the dimension may be an exophenotypic characteristic of AN. Following from this view, studies have attempted to link perfectionism causally to ED development. Perfectionism has been noted to be elevated premorbidly in those with AN and BN, compared to those with other mental disorder (Fairburn, Cooper, Doll, & Welch, 1999). However, assessed prospectively, perfectionism has not emerged as a predictor of individuals who, among healthy adolescents, would develop later ED symptoms (Calam & Waller, 1998).
We have already noted that bulimic patients can show remarkable propensities toward nonreflectiveness, behavioral disinhibition, self-harming behaviors, or other impulsive characteristics. Almost half of a cohort of normal-weight bulimics studied by Newton, Freeman, and Munro (1993), for example, met criteria for a multi-impulsive syndrome characterized by substance abuse, multiple overdoses, recurrent self-harm, sexual disinhibition, or shoplifting. Such findings corroborate the impression (described earlier) that impulse-control problems are prominent in many BN sufferers. Pronounced impulsivity in BN has been linked, in different reports, to more severe eating disturbances (binge eating, vomiting, laxative abuse, and drive for thinness), greater body-image problems, and greater generalized psychopathology—including substance abuse, self-injurious behaviors, and borderline traits (e.g., Wiederman & Pryor, 1996). However, impulsivity has not been shown to correspond to severity of bulimic symptoms in other studies (e.g., Wolfe, Jimerson, & Levine, 1994). In consequence, controversy remains around the question of whether impulsivity drives bulimic symptoms (and hence corresponds to their severity), or whether it should be regarded as an independent comorbid dimension that may heighten susceptibility but that is otherwise independent of symptom severity.
Gender Identifications. Given its gender distribution, there has been interest among ED theorists in variables reflecting gender-role adherence and gender identifications. Early findings suggested that eating-disordered women tended (in the most traditional sense of the term) to be hyperfeminine, or overidentified with traditional female roles (Sitnick & Katz, 1984).Arecent meta-analysis of 22 studies on the relationship between gender-role adherence and EDs provides modest corroboration of this proposal, finding clinical eating problems to be related positively with femininity and negatively with masculinity (Murnen & Smolak 1997).
Body-Image Perception. Given that the defining characteristics of AN and BN include disturbed body perception and experience, there has been a surprising degree of controversy around the body-image disturbance concept in the EDs. Although many empirical findings suggest overestimation of bodily proportions or unusually harsh attitudes toward body image in ED patients, many others suggest that eating-disordered individuals have body-image perceptions and attitudes that are quite normal (see Hsu & Sobkiewicz, 1991). Where abnormalities in bodily experience are identified, current findings tend to emphasize emotional and attentional factors and not perceptual ones (e.g., Carter, Bulik, Lawson, Sullivan, & Wilson, 1996). The actual origins of bodily disturbances in the EDs remain uncertain and have been postulated to reflect various factors; from social-learning influences, to effects of biological abnormalities that alter thought and perception, to the impact of body-relevant trauma.
Body Dysmorphic Disorder. Although its relationship to the EDs is uncertain, body-image disturbance is as much a central characteristic of body dysmorphic disorder (APA, 1994) as it is of EDs, and we therefore provide a special comment on this syndrome. Body dysmorphic disorder is defined by distress or functional impairment due to a preoccupation with a real (but minor) or an imagined physical defect. Because it involves an intense, distressing preoccupation (in this case with bodily characteristics) and the drive to correct perceived imperfections, it is often thought to represent a variant of OCD. Hence, one possible common pathway linking body dysmorphic disorder and eating disorders might be an underlying obsessive-compulsive structure. Regardless of whether this is true, body dysmorphic disorder appears to be prevalent in people with EDs, and it has been proposed that this convergence reflects common pathogenesis—especially at a neurobiological level (Olivardia, Pope, & Hudson, 2000)—and possible etiological convergence with OCD (see Widiger & Sankis, 2000). Consistent with the possibility of an ontological relationship, symptoms of body dysmorphic disorder have been reported to precede onset of anorexic symptoms in some anorexic patients. Indeed, some theorists have proposed that the thinness preoccupations seen in anorexic and bulimic women may represent gender-specific variants of the more generalized bodily preoccupations that manifest as body dysmorphic disorder—and which may be more focused upon fitness than on thinness among men (Widiger & Sankis, 2000). However, despite a common object of concern (i.e., the body), various differences are noted. Eating-disordered patients are noted to be mainly concerned about weight and body shape, whereas sufferers of body dysmorphic disorder have more diverse physical complaints and more pronounced negative self-evaluation and social avoidance due to appearance (Gupta & Johnson, 2000). Furthermore, EDs are, in at least some studies, noted to have broader implications for psychopathology. Hence, although speculations on commonalities remain appealing, it is premature to assume that EDs and body dysmorphic disorder are truly comparable syndromes at either phenomenological or etiological levels.
State versus Trait Issues on Personality Dimensions
Given the known effects of malnutrition (and other ED sequelae) upon the mental status, it is necessary, when studying affinities between psychological characteristics and eating disturbances, to differentiate stable,underlying traits from effects of being in an eating-disordered state. One approach to this question has been to assess characteristics in formerly eatingdisordered individuals after recovery. Certain tendencies have seemed to represent likely ED sequelae. For example, data have indicated recovered anorexics to display less harm avoidance and oppositionality and a more external locus of control than do actively ill anorexics (Bulik, Sullivan, Fear, & Pickering, 2000). Similarly, a study by our group showed rather marked illness-related sequelae (in the form of increased depression, anxiety, suicidality, interpersonal problems, and compulsivity in actively ill bulimics) that were not evident in recovered ones (Lehoux, Steiger, & Jabalpurlawa, 2000). In contrast, enduring traits of rigidity, overcautiousness, and obsessionality have been reported to persist (over several years) in recovered anorexics (Windauer, Lennerts, Talbot, Touyz, & Beumont, 1993), whereas enduring narcissistic disturbances are reported in recovered bulimics (Lehoux et al., 2000).
Binge Antecedents and Consequences
Cognitive components of dietary restraint—so-called restrictive eating attitudes (e.g., the belief that one should always eat low-calorie foods, or compensate when one eats more than usual)—are thought to make an important contribution to the development of disinhibited (binge-like) eating behaviors. Polivy and Herman’s (1985) restraint theory specifically postulates that chronic attitudinal restraint of eating potentiates the breakdown of cognitive controls upon appetitive behaviors, and eventual counterregulation (or overeating). It also proposes that counterregulation has specific cognitive and emotional triggers. An impressive catalogue of findings, derived mainly from laboratory studies in nonclinical populations, shows counterregulation of eating behavior to be induced (in attitudinally restrained eaters) by manipulations that generate (a) beliefs that one has exceeded an allowable calorie limit; (b) negative affects; (c) feelings of self-inadequacy; or (d) global disinhibition, as is induced following alcohol consumption. Clinicalexperiencedictatesthatallofthesefactorsarerelevant as binge precipitants in clinical BN patients.
The connection between binge eating and emotional factors deserves specific comment. Functional analyses of binge-eating antecedents (usually performed using on-line experience-sampling procedures) suggest that the proximal antecedents to binge episodes often include negative emotions (depression, anger, emptiness, worry), aversive social experiences, or negative self-perceptions (e.g., Polivy & Herman, 1993; Steiger, Gauvin, Jabalpurlawa, Séguin, & Stotland, 1999; Stickney, Miltenberger, & Wolff, 1999). Furthermore, data show that, compared with nonclinical dieters and nondieter controls, bulimic patients respond to laboratory stressors with increases in both hunger and the desire to binge (e.g., Tuschen-Caffier & Vogele, 1999). As for sequelae, binge episodes are reported to provide transient relief from negative feelings and thoughts and to decrease hunger and food cravings (e.g., Stickney et al.), but to heighten negative affect, poor self-esteem, and probability of further binge eating (Steiger, Gauvin, et al.) over the long term. Such consequences of binge-eating behaviors may be ingredients in the tendency for binge eating to become entrenched and self-perpetuating.
The preceding suggests that binge antecedents may include states characterized by caloric deprivation, negative affects, high social stress, and negative self-concepts. Intriguingly, available literature has also suggested that different antecedents may influence binge-eating behaviors in different individuals. In support, studies have documented a subgroup of binge eaters who deny dieting prior to the onset of eating binges (e.g., Borman Spurrel, Wilfley, Tanofsky, & Brownell, 1997). Moreover, Borman Spurrell et al. noted that people in whom binge eating preceded onset of dieting showed more evidence of personality pathology. These findings resonate with data from our research group, suggesting that restraint may be a weaker hour-to-hour antecedent to binge episodes in highly impulsive versus in less-impulsive bulimics (Steiger, Gauvin, et al., 1999). We interpret these findings as implying that processes associated with impulsivity may contribute directly to the propensity to binge. In this regard, it is noteworthy that some of our findings (described in the section titled “Neurobiology”), have linked impulsivity in bulimics to greater disturbance of central serotonin mechanisms that are also thought to underlie problems with satiety mechanisms.
Cognitive Functioning
Anorexic and bulimic ED variants have both been linked to (generally mild) neuropsychological impairments associated with higher-level cognitive functions such as active memory, attention, and problem solving (e.g., Szmukler et al., 1992). In addition, some neuropsychological data corroborate the theme of general restrictor-binger differences. Blanz, Detzner, Lay, Rose, and Schmidt (1997) found that BN but notAN patients to show better nonverbal than verbal performance, and Toner, Garfinkel, and Garner (1987) indicated bulimic anorexics to be more likely than restrictor anorexics to commit errors of commission, suggesting problems with response inhibition. Studies that examine the prospective course of neuropsychological impairments in ED patients report improvements that coincide with ED-symptom remission for both AN (Szmukler et al.) and BN (Lauer, Gorzewski, Gerlinghoff, Backmund, & Zihl, 1999). However, some findings indicate alarmingly permanent structural and neuropsychological alterations (Lambe, Katzman, Mikulis, Kennedy, & Zipursky, 1997).
Family and Developmental Characteristics
Suggestive themes emerge in family findings pertaining to the EDs. However, there are several important limitations of the literature in this area: (1) Very few of the available studies apply appropriate psychiatric control groups to establish specificity of observed patterns to eating syndromes. (2) Studies rarely provide for corroboration, by family members, of observations from actively eating-disordered participants. (3) Even when systematic tendencies are identified (ED-specific or otherwise), there remains a need to clarify whether they express dynamic family patterns (transmitted via psychosocial pathways), or effects of temperamental traits (representing inherited tendencies). These concerns aside, available data have provided partial corroboration of developmental theories on EDs (reviewed earlier).
Studies on anorexic individuals and their relatives have provided general corroboration of the concepts of enmeshment, overprotection, separation problems, and conflict avoidance. Studies report anorexics’ families to limit members’ autonomy, or to show unusually low levels of conflict. Crisp, Hsu, Harding, and Hartshorn (1980) reported disturbed parent-child interactions in about half of 102 cases of AN, with enmeshment being the most commonly reported theme. Goldstein (1981), using coded records of parent-child interactions, discriminated families of hospitalized anorexics from those of hospitalized nonanorexics, on dimensions reflecting requests for protection and conflict avoidance. Similarly, families of anorexics have been noted to show unusually low expressed emotion, indicating low levels of conflictual or disapproving interactions (Hodes & leGrange, 1993). Such observations are compatible with the concept of an enmeshed or underseparated familial organization. However, Kog, Vertommen, and Vandereycken’s (1987) study of families with an eating-disordered daughter indeed identified a subset that displayed low conflict, although they found this pattern to coincide with bulimic ED variants as frequently as it did with restrictive ones. Their finding raises some doubts about the specificity of the conflict-avoiding, enmeshed family concept for AN.
Observational studies of families in which binge-purge syndromes develop have tended to corroborate the perspective that such syndromes coincide relatively more often with overt familial discord and hostility. For example, Sights and Richards (1984) noted bulimics’ families to display marked parent-daughter stress and rated bulimics’ mothers as being domineering and demanding. Similar themes are conveyed by Humphrey’s rather extensive observational work with eating-disordered families (see Humphrey, 1991). In studies comparing bulimic-anorexic mother-father-daughter triads to those of normal triads, her findings showed the bulimicanorexic families to be more blameful, rejecting, and neglectful, and less nurturant and comforting. Likewise, in a series of studies contrasting family processes in females with normal-weight bulimia, bulimic AN, restrictive AN, or no ED, Humphrey found the families of both bulimic subgroups to be prone to deficits in parental nurturance and (to some extent) empathy. In keeping with this notion, studies have indicated expressed emotion (i.e., open conflict and critical comments) to be greater in bingers’ than in restrictors’ families (Hodes & leGrange, 1993).
Data on family interaction patterns in BED are very rare, making it premature to draw conclusions. However, Hodges, Cochrane, and Brewerton (1998) obtained self-reports on family functioning in 23 anorexic-restrictor, 45 bulimic, 20 anorexic-binger, and 43 BED women. The BED patients reported less family cohesion than did anorexic ones and less familial expressiveness than did bulimic ones. The BED women also indicated their families to show less cohesion, expressiveness, independence, and intellectual-cultural and active-recreational pursuits than did women in a normal control group. Relative to the normal control women, BED patients reported their families to be higher on dimensions measuring conflict and control. In other words, BED patients seemed to be reporting a constellation of family interaction patterns that was at least partially reminiscent of those of BN patients.
Although there are systematic convergences between family interaction patterns (on the one hand) and ED subtypes (on the other), recent thinking on family factors in the EDs is close to abandoning the probably unrealistic notion that there may be ED-specific family interaction variants. Instead, theorists address more interesting questions about the possible modulating role of family functioning in the development and maintenance of eating symptoms. Schmidt, Humfress, and Treasure (1997) noted that severity of family dysfunction corresponds closely to severity of personality pathology in affected individuals, suggesting a modulating influence of family functioning enacted through concurrent psychopathological traits.
Psychosocial Induction
It is appealing to presume that the EDs depend upon psychosocial induction effects in which parents convey maladaptive concerns with body image, weight, and eating to their children. Indeed, in clinical populations, many studies report parents of ED sufferers to show abnormal eating and body-image attitudes (e.g., Hall & Brown, 1983). However, many others report an absence of differences between parents with and without eating-disordered daughters (e.g., Hall, Leibrich, Walkley, & Welch, 1986). At the same time, various findings are consistent with parental influences upon children’s eating behavior. Miller, McCluskey-Fawcett, and Irving (1993) compared perceptions of early mealtime experiences across normal eaters, repeat dieters, and bulimics, and found the bulimics to display more eating-related issues in the early family context. In a related vein, a recent study of 369 adolescent girls and their parents found that parents’ encouragements to daughters to lose weight were more significant as predictors of daughters’ dietary restraint than were parents’ own dietary restraint levels, and mothers’ encouragements were more influential than were fathers’ (Wertheim, 1999). Such findings may be sensitive to retrospective reporting biases but they are consistent with the idea that the family’s eating and body-image-relevant attitudes can convey risk for an ED.
Yet another source of parental influence over children’s eating patterns is suggested by data showing a disturbing degree of association between mothers’ EDs and feeding problems in children. Whelan and Cooper (2000) rated a filmed family meal in three groups of 4-year-olds: Children with feeding problems (N 42), children with a nonfeeding form of disturbance (e.g., shyness or behavioral disturbance; N 79), and children with no disturbance (N 29). They found mothers of children with feeding problems, when compared to mothers in the other two groups, to have higher rates of current and past EDs but not mood disorders.
Attachment
On the basis of a review of studies concerning parent-child and familial attachment patterns in the EDs, Ward, Ramsay, Turnbull, Benedettini, and Treasure (2000) concluded that ED patients display pathological attachment tendencies. Various studies have indicated that individuals with anorexia, relative to healthy controls, report one or both parents to be less affectionate, empathic, caring, or protective (Rhodes & Kroger, 1992; Steiger, Van der Feen, Goldstein, & Leichner, 1989). Rhodes and Kroger found anorexic individuals to be anxious about parental separation and engulfment, whereas Armstrong and Roth (1989) found AN subjects to have more anxious attachments and separation depression than controls. While such findings are suggestive, we note that they do not necessarily imply ED-specific anomalies.
Data indicate parallel attachment problems in BN. Individuals with bulimia report themselves to form dependent or insecure attachments (Jacobsin & Robins, 1989), to be mistrustful of others, anxious about revealing imperfections, and fearful of intimacy (Pruitt, Kappins, & Gorman, 1992). An experience-sampling study by our group highlights the potential importance of relationship factors in BN, in that stressful social experiences emerged as relatively direct antecedents to binge episodes in actively bulimic women (Steiger, Gauvin, et al., 1999).
Childhood Sexual Abuse
Modal figures indicate roughly 30% of ED sufferers to report some form of unwanted sexual experience during childhood (e.g., Everill & Waller, 1995; Wonderlich et al., 1997). Given that they implicate such markedly disturbed bodily experience, it is enticing to think that EDs may be specifically (and causally) linked to body-relevant trauma occurring during childhood. However, it should be noted that observed rates of trauma in ED sufferers do not consistently exceed those obtained in females with other psychopathology, an implication that there is a strong but nonspecific association of the EDs with childhood trauma.
Data comparing prevalence of childhood sexual trauma in restricting and binging subgroups have suggested that bulimic ED variants might be associated with the more unfavorable developmental experiences. Schmidt et al. (1997), for example, conclude that findings have consistently associated childhood abuse more strongly with binge-purge than with restrictive ED variations. In keeping with the suggested tendency, Webster and Palmer (2000) found that women with bulimic symptomatology (but not restrictive AN) reported more troubled childhood experiences than did normal-eater comparison women, but reported experiences comparable to those of women with depression. Although such observations could reflect greater repression in restrictors, or protectiveness of the family, the trend in question would also be consistent with an overall portrait of the bulimic family as being the more destructive, abusive, or neglectful, rendering the child subject to a heightened risk of abuse. These data also reiterate the point made earlier about relative nonspecificity of the link between EDs and childhood abuse.
Community-survey data have corroborated the notion that BN coincides with relative elevations of victimization experiences. A telephone survey of 3,006 women linked history of forcible assault or rape to BN more than to BED or non–eating disordered status. Furthermore, in this study, reliance upon compensatory behaviors was associated with higher rates of victimization (Dansky, Brewerton, Kilpatrick, & O’Neil, 1997). Even if childhood traumata are more strongly linked to bulimic than to restrictive ED variants, however, this need not imply bulimia-specific pathogenic effects. Several studies in BN have noted that severity of childhood abuse predicts severity of personality pathology, impulsivity, dissociative potentials, and other forms of comorbid psychopathology more directly than it does severity of bulimic symptoms. For example, a study comparing 50 sexually abused versus 83 nonsexually abused eatingdisordered women showed elevations in the sexually abused women, not on ED symptoms, but on various self-reported personality dimensions: schizotypal, avoidant, schizoid, passive-aggressive, and borderline (Moreno, Selby, & Neal, 1998). One study of 44 former bulimics found that those with a history of sexual or physical abuse (N 20) had more posttraumatic symptoms and more substance dependence (Matsunaga, Kaye, et al., 1999).
Sociocultural Context
Eating disorders occur disproportionately often in Western industrialized nations, implying that cultural ideals prevailing in the West may be conducive to ED development. It is obvious that Western social values to some extent equate slimness with cultural ideals of success, beauty, power, and self-control, and there is little doubt that such factors play some role in the development of clinical EDs (see Garfinkel & Garner, 1982). Changing ideals for female body shape are thought to be associated with the apparent increase in incidence of EDs that occurred in the West during the decades since 1960 (see the section titled “Epidemiology”). This period coincided with a dramatic shift in a cultural ideal—from a voluptuous form represented by such icons as Marilyn Monroe, Elizabeth Taylor, or Sophia Loren to a thin (and often relatively androgynous) ideal for female appearance that became popular in the early 1960s, and that remains prominent in celebrity and media images in the 2000s.Attesting to the importance of peer and pop culture influences in the development of maladaptive eating, a 1-year prospective study of 6,982 girls showed that measures of the felt importance of looking like the females that are seen on television, in movies, or in magazines predict the onset of regular vomiting or laxative abuse as a means of weight control (Field, Camargo, Taylor, Berkey, & Colditz, 1999). Further supporting the concept that social values pertinent to thinness have a causal role in EDs, the work of Garner and Garfinkel (see Garfinkel & Garner, 1982) shows AN to occur exceptionally often in individuals whose social milieu emphasizes weight control (e.g., ballet dancers, models, or athletes). In a related vein, various findings suggest that Western cultural values have a special role in generating risk for ED development. Davis and Katzman (1999) noted that level of eating and body-image concerns corresponded quite directly to the level of acculturation toAmerican values of Chinese university students studying in the United States. Likewise, Lake, Staiger, and Glowinski (2000) compared Australian-born and Hong Kong–born Australian university students on eating attitudes and body-shape perceptions, and found that Australian-born and Western-acculturated Hong Kong–born women showed greater body-image problems.
Although risk for EDs is certainly linked to Western social contexts, such social effects may yet have only a limited influence in ED etiology. For example, systematic cross-cultural research indicates anorexia-like syndromes, characterized by food refusal, to be prevalent in diverse (non-Western) contexts (Pate, Pumariega, Hester, & Garner, 1992), suggesting that anorexia-like syndromes may not be as culture-bound as once thought. A self-report assessment of attitudes toward eating among undergraduate women studying in Pennsylvania (N = 111) and South Korea (N = 115) showed similar percentages (21% and 18%, respectively) of respondents reporting elevations on an ED-screening instrument (Lippincott & Hwang, 1999). Indeed, some cross-cultural data reduce emphasis upon the role of cultural pressures favoring slimness in ED pathogenesis altogether. Lee, Ho, and Hsu (1993), for example, provided a well-constructed study of individuals with anorexia in Hong Kong—all of whom were clearly anorexic according to criteria reflecting self-imposed weight loss, resistance to others’ encouragements to eat, and amenorrhea (or loss of libido, in one male case). However, unlike individuals with anorexia encountered in American contexts, roughly 60% were noted to display no conscious fear of becoming fat. They justified their food refusal instead by stating a desire to avoid gastric bloating. Given similar findings from other Asian studies, Lee and colleagues proposed that fat phobia may be characteristic of weight-conscious Western societies but not definitive of AN at large.These findings imply that culture may exert pathoplastic effects that shape ultimate ED expression.
Other cross-cultural studies have reported an absence of cultural influences or culture-free universals that apply to the EDs. For example, bulimic tendencies and proneness to generalized impulse-control problems have been noted to coincide as much in Japanese samples as in Western cases (Matsunaga, Kiriike, et al., 2000). Similarly, cross-cultural data make a case that, regardless of cultural context, EDs and OCD converge (Matsunaga, Kiriike, et al., 1999). Emphasizing a universal importance of maladaptive family interactions as an ED correlate, one study has shown that the degree of maladaptive eating attitudes and behaviors in British Asian schoolgirls correlates with measures of familial overprotection and conflicts around socializing (Furnham & Husain, 1999).
Biological Factors
Family Studies
Findings from available family studies provide unequivocal support for the conclusion that there is familial aggregation for the EDs, a prerequisite if one assumes biological transmission. The largest case-controlled study available examined the prevalence of EDs among first-degree relatives of 300 probands with AN or BN (Strober, Freeman, Lampert, Diamond, & Kaye, 2000). This investigation found substantially higher risks for AN in female relatives of anorexic and bulimic probands (relative risks of 11.3 and 12.3, respectively) compared to those obtained in relatives of normaleater comparison subjects. A familial propensity was also indicated for BN, with relative risks of 4.2 for relatives of anorexic probands and 4.4 for bulimic probands, respectively. These findings suggest a strong family tendency for both anorexic and bulimic ED variants, but stronger aggregation for AN than for BN. Results of another recent family study have suggested that relatives of AN and BN probands both show similarly elevated risk for ED, withoutAN or BN specificity (Lilenfeld et al., 1998). These findings are consistent with familial transmission for a general factor that heightens susceptibility to EDs, but not specifically toAN or BN.
Cotransmission in Families With Other Syndromes
Family data need not imply disorder-specific transmission effects. Rather, they could reflect a liability that is conveyed by linkage within the family to another heritable disturbance or syndrome. Relationships of this type have been explored for the EDs with respect to various forms of psychopathology. Family studies suggest substantially higher rates of mood disorders, especially unipolar depression, among relatives of anorexic (e.g., Strober, Lampert, Morrell, Burroughs, & Jacobs, 1990) and bulimic (e.g., Logue, Crowe, & Bean, 1989) probands. However, when distinctions between ED probands with and without an ascertained history of mood disorder have been made, findings reveal increased risk of affective disorders in only the relatives of those ED probands who themselves suffer from mood disturbance (Lilenfeld et al., 1998; Strober et al.). In other words, while shared vulnerability factors may be implicated, there does not seem to be any simple or direct cotransmission for eating and affective disturbances.
Similarly, various studies have documented an increased rate of alcohol and drug abuse in ED patients and their relatives, especially in the relatives of bulimic probands (Lilenfeld et al., 1998). However, as noted for mood disorders, evidence on the co-aggregation of eating and substance-use disorders favors belief in independent transmission because only the relatives of ED probands who themselves abuse substances show consistently higher risk of substance-abuse problems (e.g., Lilenfeld et al.). Likewise, Lilenfeld and colleagues report that only eating-disordered probands who themselves show heightened OCD have family histories characterized by higher OCD prevalence. In other words, familial transmission of OCD appears also to occur independently of EDs.
In an intriguing contrast to the preceding, Lilenfeld and colleagues (1998) have also suggested shared familial transmission of obsessive-compulsive personality disorder (OCPD) with AN (but not BN). In their study, relatives of anorexic probands showed elevated OCPD, regardless of the presence of OCPD in the anorexic proband. Such findings are in keeping with the notion that there may be a relatively ANspecific transmission, within families, of personality traits of perfectionism, rigidity, and harm avoidance (i.e., OCPD) and risk for AN.
Twin Studies
Through comparison of concordance rates in genetically identical (i.e., monozygotic) versus nonidentical (i.e., dizygotic) twins, it becomes possible to isolate genetic factors that contribute to a disorder. Twin data can, furthermore (using behavioral-genetic models), be analyzed to tease apart the relative contributions of additive-genetic effects (i.e., inherited liabilities) , shared-environmental effects (i.e., liabilities resulting from such influences as general familyinteraction patterns, or the family’s socioeconomic status), and effects of the nonshared or individual-specific environment (i.e., liabilities related to having experienced childhood trauma, or having had a particular type of relationship with one parent). Various twin studies of EDs have now been completed, providing intriguing yet equivocal findings.
In a clinically ascertained sample of 31 monozygotic and 28 dizygotic anorexic twins, Treasure and Holland (1989) found substantially higher concordance in monozygotic than in dizygotic pairs (45% vs. 2%, respectively). Furthermore, when diagnostic criteria were narrowed to accept only restricting AN (i.e., excluding patients with binge or purge symptoms), differences between mono- and dizygotic twins became even more striking—with concordance increasing to 65% for monozygotic and falling to 0% for dizygotic. Such findings imply rather striking heritability for a restrictive AN factor, and based on their results, Treasure and Holland estimated a 70% liability for restrictive AN attributable to additive genetic effects. Raising controversy around such conclusions, however, Walters and Kendler (1995), in a population-based (vs. Clinically ascertained) sample, obtained no evidence of heightened risk for AN in monozygotic compared to dizygotic twins.
A reanalysis of combined data from the early-available twin studies on BN revealed 46% concordance for monozygotic twins versus 26% concordance for dizygotic twins, with an estimated 47% of the variance attributable to additive genetic effects, 30% to shared environment, and 23% to nonshared environment (Bulik, Sullivan, Wade, et al., 2000). Similarly, a population-based study of 2,163 female twins found concordance rates for BN to be 22.9% for monozygotic and 8.7% for dizygotic twins (Kendler et al., 1991), with an estimated 55% of variance from additive genetic effects, 0% from shared environment, and 45% from individual-specific environmental effects. Other studies have examined genetic effects acting upon more broadly defined (subthreshold) variants of BN. For example, Bulik, Sullivan, and Kendler (1998) estimated heritability of broadly defined BN to be 83% in a sample of 854 twin pairs, suggesting that BN is quite a heritable syndrome.
Genetic Linkage Studies
Genetic linkage studies seek to identify genes, in affected individuals and their relatives, that may underlie risk for a specific disorder. Studies aimed at candidate genes underlying ED vulnerability have focused on genes coding for dopamine, serotonin, and noradrenaline systems, under the assumption (which will be explained further) that these monoamines may regulate eating behavior. To date, relevant studies in anorexic samples have failed to find systematic linkage of particular variants of dopamine (Bruins-Slot et al., 1998) or 3-adrenergic receptor (Hinney et al., 1997) genes in AN. The search for candidate genes within the serotonin (5-hydroxytryptamine, or 5HT) system has, however, yielded somewhat more promising results. Association has been reported between AN and a polymorphism (–1438G/A) in the promoter region of the 5HT2A receptor (Enoch et al., 1998). Furthermore, this 5HT2A finding has been found to be associated with both AN restrictor subtype and OCD, but not with bulimic ED variants. Together, such findings argue that the 5HT gene variation in question may correspond to both “anorexic” and “generalized” obsessions and compulsions.
Possible genetic substrates for BN are also identified. Levitan et al. (2000) reported an association between the C218 allele of the gene encoding for tryptophan hydroxylase (or TPH, the rate-limiting enzyme for 5HT synthesis) and BN. It is pertinent to note that Nielsen and colleagues (1998) reported a similar association, in male offenders, between a TPH gene variant (on the one hand) and suicidality and alcoholism (on the other hand), suggesting that this gene variant may correspond to an impulsive–behaviorally dysregulated phenotype. Such findings, viewed together, are consistent with the tendency of bulimic ED variants to be characterized by impulsivity and behavioral dyscontrol.
Neurobiology
The search for neurobiological agents that are implicated in the pathophysiology of EDs has led to the exploration of neurotransmitter, neuropeptide, and hormone systems involved in appetite, feeding behaviors, affect regulation, and temperament.
Neurotransmitters. Various monoamine neurotransmitters play a role in appetite regulation.Actions upon appetitive behaviors of noradrenaline and dopamine appear to include both excitatory and inhibitory effects upon feeding behavior, depending upon receptor sites stimulated. In contrast, serotonin (5HT), via its action on hypothalamic receptors, is believed to act mainly in the mediation of satiety.Animal and human studies indicate experimental manipulations that increase 5HT neurotransmission to lead to suppression of food intake, whereas antagonism of 5HT leads to hyperphagia (see Brewerton, 1995). We shall review the findings obtained for AN and BN in studies of each of these systems.
Several investigations have studied the noradrenergic system in AN. Anorexia nervosa has been associated with reduced concentrations of noradrenaline and its major metabolite, 3-methoxy-4-hydroxyphenylglycol (MHPG) in cerebrospinal fluid (CSF), as well as with increased density and sensitivity of platelet 2-adrenergic receptors (see Fava, Copeland, Schweiger, & Herzog, 1989). However, after nutritional rehabilitation, CSF MHPG levels in women with AN are found to compare to those of control women (Kaye, Frank, & McConaha, 1999), suggesting that changes in the noradrenergic system may mainly constitute adaptations to starvation. Studies of dopamine activity in AN have yielded contradictory results. Kaye, Ebert, Raleigh, and Lake (1984) reported anorexic women to show lower CSF homovanillic acid (HVA, a dopamine metabolite) than did control women, and then, in a 1999 study, reported lower CSF HVA in a group of recovered anorexic restrictors and a tendency toward lower HVA in recovered anorexic bingers. Although such findings imply lowered dopamine activity in active or recovered AN, Johnston, Leiter, Burrow, Garfinkel, and Anderson (1984) found no differences when comparing HVA levels in women with anorexia to those in controls.
Studies of the serotonin system have revealed various 5HT abnormalities, consistent with reduced 5HT tone, in active anorexics, including (a) decreased platelet binding of serotonin uptake inhibitors (Weizman, Carmi, Tyano, Apter, & Rehavi, 1986); (b) blunted prolactin and cortisol responses to 5HT agonists and partial agonists (Monteleone, Brambilla, Bortolotti, La Rocca, & Maj, 1998); and (c) reduced CSF levels of 5HT metabolites (Kaye et al., 1984). Some investigators have reported normalization of prolactin response to a 5HT releasing agent, d-fenfluramine, in recovered anorexics (Ward, Brown, Lightman, Campbell, & Treasure, 1998), as might indicate a state-related 5HT abnormality. In contrast, Kaye, Gwirtsman, George, and Ebert (1991) found elevated CSF 5-hydroxyindoleacetic acid (or 5HIAA, a 5HT metabolite) in a sample of weight-restored anorexics. They interpreted this apparently anomalous finding as an indication that AN and associated traits (e.g., harm avoidance, perfectionism) may actually be linked to a primary state of increased 5HT tone that is then masked by malnutrition-induced reductions in 5HT activity during active stages of the disorder. Further work is needed to clarify this possibility.
As with AN, findings in BN have been consistent with decreased noradrenaline activity. For example, women with BN have been reported to show low resting levels of plasma noradrenaline (Kaye et al., 1990). Given a study reporting normal CSF MHPG levels in recovered bulimics, however, it appears that noradrenaline abnormalities in BN may need to be regarded as state-dependent effects (Kaye et al., 1998). Studies focused on dopaminergic activity in BN have documented low CSF HVA (a dopamine metabolite) in active BN (Jimerson, Lesem, Kaye, & Brewerton, 1992). However, again, one study reports normal CSF HVAlevels in recovered bulimics (Kaye et al., 1998).
More extensive than that in AN, study of the 5HT system in BN has consistently suggested reduced 5HT activity. Bulimia nervosa patients are noted to display (a) decreased CSF 5HIAA (Jimerson et al., 1992), (b) reduced platelet binding of 5HT uptake inhibitors (Steiger et al., 2000), and (c) blunted neuroendocrine responses to 5HT precursors and 5HT agonists or partial agonists (e.g., Levitan et al., 1997; Steiger, Koerner, et al., 2001). Such findings have been taken to suggest decreased brain 5HT turnover and down-regulation of postsynaptic 5HT receptors mediating neuroendocrine responses. Other studies have used dietary manipulations to explore links between 5HT levels and bulimic symptoms. For instance, tryptophan depletion, which lowers brain tryptophan and subsequent 5HT synthesis, has been shown to exacerbate bulimic symptoms in actively bulimic women (Kaye et al., 2000) and to lead to transient reappearance of bulimic symptoms in recovered bulimics (Smith, Fairburn, & Cowen, 1999). These results appear to reflect a particular vulnerability within the 5HT system of women at risk for BN and establishes a potential neurobiological substrate for antecedent effects of dieting in BN.
Given their marked co-aggregation, there has been an interest in the possibility that bulimic symptoms and impulsivity have a common serotonergic basis. In non–eating disordered populations,datadocumentaclearassociationbetweenimpulsivity and low 5HT (Coccaro et al., 1989). Paralleling such findings,Steiger,Koerner,etal.(2001b)foundcorrespondence between the extent of apparent reduction in 5HT activity and the severity of impulsive symptoms. Such findings imply that 5HT abnormalities may mediate both binge eating and impulsive symptoms, and may (in part) account for the frequent convergence of BN with problems of impulse regulation.
Appetite-Regulating Peptides and Hormones. Cholecystokinin (CCK), a peptide secreted by the gut, acts on the hypothalamus to produce satiety. Available data suggest low basal and postprandial (after-eating) plasma CCK in BN, but not in AN (Pirke, Kellner, Frie, Krieg, & Fichter, 1994). It is not known to what extent low CCK in BN may preexist disorder onset or may result from abnormal eating behaviors. Regardless, once established, low CCK could help perpetuate binge-eating behavior via its impact on satiety.
Leptin is a newly identified hormone secreted by fat cells. Leptin acts on the hypothalamus to regulate appetite and energy expenditure in accordance with fat stores. In active AN, findings have shown reductions in serum and CSF leptin levels corresponding to decreased body mass (Grinspoon et al., 1996). Findings have also shown restoration of normal levels upon weight recovery (Hebebrand et al., 1997). However, although low leptin levels in AN may, therefore, be partly attributable to low fat stores, one study found decreased leptin in restricting but not purging anorexics, despite equally low body weight in both groups (Mehler, Eckel, & Donahoo, 1999).Astudy of bulimic women has also reported low leptin levels, despite normal body weight (Monteleone, Di Lieto, Tortorella, Longobardi, & Maj, 2000). Leptin levels may, therefore, not be modulated by body weight alone, and further work is needed to investigate the full interplay that may exist between leptins and the EDs.
Neuroimaging Studies. Neuroimaging studies aim to establish structural or functional brain abnormalities and use techniques like computerized tomography (CT) and magnetic resonance imaging (MRI) to allow visualization of gross brain structure. Functional neuroimaging techniques, including positron emission tomography (PET) and proton magnetic resonance spectroscopy (H-MRS), are used to analyze specific chemical and electrical activity within the brain. With the use of CT and MRI, structural brain changes have been detected in both anorexic and bulimic patients. Findings include enlarged ventricles and sulcal widening, gray- and white-matter abnormalities, and lateralization of deficits (e.g., Hoffman et al., 1989). Reversible and irreversible components have been identified, including persistent graymatter (but not white-matter) volume deficits in weightrecovered anorexics (Lambe et al., 1997). Taken together, imaging studies suggest that many abnormalities constitute transient effects of nutritional deprivation, but that some may be disturbingly permanent sequelae.
An Integrated (Multidimensional) Etiological Concept
In a social context that equates thinness with many social values, it is not surprising to find that most people display bodyimage and diet consciousness, and that an alarming number of these persons (especially young women) progress to the development of full-blown EDs. However, as much as the EDs are defined by pathognomonic preoccupations with eating, weight-control, and body image, they are also polysymptomatic syndromes, invariably including characterological, affective, interpersonal, and self-regulatory disturbances. Syndromes with this degree of phenomenological complexity are likely to implicate diverse causal processes. An adequate etiological model for the EDs will need to account for roles of converging biological, psychological, familial, and sociocultural processes.
In attempting to understand ED etiology, we have often found it heuristic to contemplate two classes of causal agents, each having its own character and each (presumably) its own multiple (biopsychosocial) etiological agents. One factor relates to eating-specific aspects of disturbance (surrounding eating, weight, and body image); the other relates to more generalized vulnerabilities, psychopathology, or maladaptation. This proposal, that EDs implicate eating-specific and generalized components of pathology, was first addressed in the two-component model of eating disorders proposed by Garner, Olmstead, Polivy, and Garfinkel (1984). A basic aspect of this view is that eating-specific concerns are not sufficient to explain the development of clinical ED, and that the concurrent presence of a more generalized psychopathology, expressed through broad mood and behavioral dysregulation, is required. How might generalized and eating-specific factors interact in ED pathology? To reflect a diversity of possible pathways, we provide some illustrative examples.
- Constitutional vulnerabilities (e.g., inherited problems of serotonin neurotransmission) may, along with their predictable effects on mood and impulse regulation, confer vulnerability to disorders of satiation (and hence bulimic eating patterns) in individuals disposed by social or family pressures emphasizing thinness to restrict their food intake. This might, in part, explain an affinity of bulimic eating syndromes for manifestations including mood or impulse dyscontrol and, in part, findings showing BN to be associated with reduced serotonin functioning. In other words, BN may (at least sometimes) implicate a generalized (serotonin-linked) risk factor, related to susceptibility to impulsivenessandappetitivedysregulation,butwhatmight be needed to trigger the expression of this vulnerability is a specific pressure or encouragement toward dietary restraint.
- Given a social context that overvalues thinness and that links body-esteem to overall self-esteem (especially in women), generalized self-image problems in females (along with a propensity to be perfectionistic or overly sensitive to social approval) might indirectly heighten susceptibility to dieting and, eventually, to pathological eating practices. In this eventuality, one would expect (as tends to be the case) to find perfectionism, self-criticism, reward dependence, and related characteristics in ANprone individuals. We presume that such (generalized) tendencies heighten the likelihood that normal (eatingspecific) social concerns about slimness may be carried, in clinical ED sufferers, to the pathological extreme.
- Parental overprotection or overcontrol, while alone insufficient to explain ED development, might support the progression from compulsive dieting to frank eating obsession in the weight-conscious adolescent. Furthermore, the adolescent’s rejection of parental controls might, if the parents themselves showed propensities toward compulsiveness or anxious overcontrol, mobilize destructively intrusive overreactions on the part of the parents. The child’s further opposition would gradually feed into an escalating spiral of parental intrusiveness followed by angry oppositionality on the part of the affected child. Self-starvation seems, at least sometimes, to be mobilized as a weapon in such an escalation of conflict.
In each of the preceding examples, we assume that development of a clinical ED requires that thresholds be surpassed in key areas of vulnerability, some eating-specific, some more generalized. A main implication of this view is that diffuse psychopathology, while not representing an ED-specific ingredient, might be a manifestation of a process that serves to enhance risk of ED development. At the same time, it is also necessary to contemplate the full range of interactions (among biological, psychological, and social factors) that may occur once an ED has developed, such that increasingly more severe and more entrenched eating and generalized disturbances may ensue. Consider the following hypothetical examples.
In the first example, an insecure adolescent girl with an anxious, perfectionistic bent (prone to difficulties with establishing limits around her own performance) begins dieting to bolster her self-esteem. Weight loss produces various social rewards as peers and parents pay her more positive attention. However, dieting also leads to alteration of normal neurobiological systems (known sequelae of intensive dieting). One consequence can be an exacerbation of anxiety and obsessionality and, gradually, increasing preoccupation with thinness. Her natural tendency to demand too much of herself evolves, under new biological influences, into full-blown obsession—and intensive dieting gradually evolves into a full-blown ED.
Alternatively, consider the effects, in a second adolescent, in whom a very-destructive developmental environment characterized by parental hostility and physical abuse has (aside from having damaging effects upon her sense of selfworth) been a manifestation of a family wide tendency towards impulse dysregulation. Assume that the family tendency of impulse dysregulation may have been borne, in part, by genes that code for lowered serotonin synthesis and neurotransmission. For this girl, dieting to achieve a better selfimage (which would reduce brain serotonin activity even further) may not only lower the threshold for the expression of impulsive tendencies, but may lower the threshold for binge eating by creating impairment in satiety mechanisms. She might gradually develop binge eating, while at the same time becoming progressively more disinhibited, irritable, labile, and self-damaging. An implicit concept, especially important in designing eventual treatments, is that ED symptoms can become quite self-perpetuating, and in time, quite divorced from the psychobiological and sociocultural factors that may have originally contributed to the development of the disorder.
If ED etiology is as genuinely biopsychosocial as findings lead us to believe, then the study of eating disorders may inform theory on psychopathology in many ways, including the manner in which psychopathology can represent the activation of latent genetic vulnerabilities through specific environmental pressures; the manner in which latent traits and tendencies can be shaped by developmental experiences; and how maladaptive traits within the at-risk individual can mobilize destructive responses from the social environment. In addition, the EDs teach us to appreciate the ways in which socially prescribed responses (even those as apparently innocuous as a young girl’s dieting) can, in specifically vulnerable individuals, generate multiple and highly maladaptive repercussions that can come to broadly affect an individual’s global psychological development and functioning.
Bibliography:
- American Psychiatric (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author.
- Armstrong, J., & Roth, D. M. (1989). Attachment and separation difficulties in eating disorders: A preliminary investigation. International Journal of Eating Disorders, 8, 141–155.
- Blanz, B. J., Detzner, U., Lay, B., Rose, F., & Schmidt, M. H. (1997). The intellectual functioning of adolescents with anorexia nervosa and bulimia nervosa. European Child and Adolescent Psychiatry, 6, 129–135.
- Borman Spurrel, E. B., Wilfley, D. E., Tanofsky, M. B., & Brownell, K. D. (1997). Age of onset for binge eating: Are there different pathways to binge eating? International Journal of Eating Disorders, 21, 55–65.
- Brewerton, T. D. (1995). Toward a unified theory of serotonin dysregulation in eating and related disorders. Psychoneuroendocrinology, 20, 561–590.
- Brewerton, T. D., Lydiard, R. B., Herzog, D. B., Brotman, A. W., O’Neil, P. M., & Ballenger, J. C. (1995). Comorbidity of Axis I psychiatric disorders in bulimia nervosa. Journal of Clinical Psychiatry, 56, 77–80.
- Bruch, H. (1973). Eating disorders: Obesity, anorexia nervosa and the person within. New York: Basic Books.
- Bruins-Slot, L., Gorwood, P., Bouvard, M., Blot, P., Ades, J., Feingold, J., Schwartz, J., & Mouren-Simeoni, M. (1998). Lack of association between anorexia nervosa and D3 dopamine receptor gene. Biological Psychiatry, 43, 76–78.
- Bulik, C. M., Sullivan, P. F., Fear, J. L., & Pickering, A. (2000). Outcome of anorexia nervosa: Eating attitudes, personality, and parental bonding. International Journal of Eating Disorders, 28, 139–147.
- Bulik, C. M., Sullivan, P. F., & Kendler, K. S. (1998). Heritability of binge-eating and broadly defined bulimia nervosa. Biological Psychiatry, 44, 1210–1218.
- Bulik, C. M., Sullivan, P. F., Wade, T. D., & Kendler, K. S. (2000). Twin studies of eating disorders: Areview. International Journal of Eating Disorders, 27, 1–20.
- Bulik, C. M., Sullivan, P. F., Weltzin, T. F., & Kaye, W. H. (1995). Temperament in eating disorders. International Journal of Eating Disorders, 17, 251–261.
- Calam, R., & Waller, G. (1998). Are eating disorders and psychosocial characteristics in early teenage years useful predictors of eating characteristics in adult years? A7-year longitudinal study. International Journal of Eating Disorders, 24, 351–362.
- Carter, F. A., Bulik, C. M., Lawson, R. H., Sullivan, P. F., & Wilson, J. S. (1996). Effect of mood and food cues on body image in women with bulimia and controls. International Journal of Eating Disorders, 20, 65–76.
- Casper, R. C., Hedeker, D., & McClough, J. F. (1992). Personality dimensions in eating disorders and their relevance for subtyping. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 830–840.
- Cassidy, E., Allsopp, M., & Williams, T. (1999). Obsessivecompulsive symptoms at initial presentation of adolescent eating disorders. European Child & Adolescent Psychiatry, 8, 193–199.
- Coccaro, E. F., Siever, L. J., Klar, H. M., Maurer, G., Cochrane, K., Cooper, T. B., Mohs, R. C., & Davis, K. L. (1989). Serotonergic studies in patients with affective and personality disorders:
- Correlates with suicidal and aggressive behavior. Archives of General Psychiatry, 46, 587–599.
- Crago, M., Shisslak, C. M., & Estes, L. S. (1996). Eating disturbances among American minority groups: A review. International Journal of Eating Disorders, 19, 239–248.
- Crisp, A. H. (1980). Anorexia nervosa: Let me be. London: Academic Press.
- Crisp, A. H., Hsu, L., Harding, B., & Hartshorn, J. (1980). Clinical features of anorexia nervosa: A study of a consecutive series of 102 female patients. Journal of Psychosomatic Research, 24, 179–191.
- DaCosta, M., & Halmi, K. A. (1992). Classifications of anorexia nervosa: Question of subtypes. International Journal of Eating Disorders, 11, 305–313.
- Dansky, B. S., Brewerton, T. D., Kilpatrick, D. G., & O’Neil, P. M. (1997). The National Women’s Study: Relationship of victimization and posttraumatic stress disorder to bulimia nervosa. International Journal of Eating Disorders, 21, 213–228.
- Davis, C., & Katzman, M. A. (1999). Perfection as acculturation: Psychological correlates of eating problems in Chinese male and female students living in the United States. International Journal of Eating Disorders, 25, 65–70.
- Demitrack, M. A., Putnam, F. W., Brewerton, T. D., Brandt, H. A., & Gold, P. W. (1990). Relation of clinical variables to dissociative phenomena in eating disorders. American Journal of Psychiatry, 147, 1184–1188.
- Enoch, M. A., Kaye, W. H., Rotondo, A., Greenberg, B. D., Murphy, D. L., & Goldman, D. (1998). 5-HT2A promoter polymorphism1438G/A, anorexia nervosa, and obsessive-compulsive disorder. Lancet, 351, 1785–1786.
- Everill, J., & Waller, G. (1995). Reported sexual abuse and eating psychopathology: A review of evidence for a causal link. International Journal of Eating Disorders, 18, 1–11.
- Everill, J., Waller, G., & Macdonald, W. (1995). Dissociation in bulimic and non-eating-disordered women. International Journal of Eating Disorders, 17, 127–134.
- Fairburn, C. G. (1995). Overcoming binge eating. New York: Guilford Press.
- Fairburn, C. G., Cooper, Z., Doll, H. A., & Welch, S. L. (1999). Risk factors for anorexia nervosa: Three integrated case-controlled comparisons. Archives of General Psychiatry, 56, 468–476.
- Fairburn, C. G., Doll, H. A., Welch, S. L., Hay, P. J., Davies, B. A., & O’Connor, M. E. (1998). Risk factors for binge eating disorders: A community-based study. Archives of General Psychiatry, 55, 425–432.
- Fava, M., Copeland, P. M., Schweiger, U., & Herzog, D. (1989). Neurochemical abnormalities of anorexia nervosa and bulimia nervosa. American Journal of Psychiatry, 146, 963–971.
- Field, A. E., Camargo, C. A., Taylor, C. B., Berkey, C. S., & Colditz, G. A. (1999). Relation of peer and media influences to the development of purging behaviors among preadolescent and adolescent girls. Archives of Pediatrics & Adolescent Medicine, 153, 1184–1189.
- Fitzgibbon, M. L., & Blackman, L. R. (2000). Binge eating disorder and bulimia nervosa: Differences in the quality and quantity of binge eating episodes. International Journal of Eating Disorders, 27, 238–243.
- Furnham, A., & Husain, K. (1999). The role of conflict with parents in disordered eating among British Asian females. Social Psychiatry & Psychiatric Epidemiology, 34, 498–505.
- Gard, M. C. E., & Freeman, C. P. (1996). The dismantling of a myth: A review of eating disorders and socioeconomic status. International Journal of Eating Disorders, 20, 1–12.
- Garfinkel, P., & Garner, D. (1982). Anorexia nervosa: A multidimensional perspective. New York: Brunner/Mazel.
- Garfinkel, P. E., Lin, E., Goering, P., Spegg, C., Goldbloom, D. S., Kennedy, S., Kaplan, A. S., & Woodside, D. B. (1995). Bulimia nervosa in a Canadian community sample: Prevalence and comparison of subgroups. American Journal of Psychiatry, 152, 1052–1058.
- Garner, D., Olmsted, M., Polivy, J., & Garfinkel, P. (1984). Comparison between weight preoccupied women and anorexia nervosa. Psychosomatic Medicine, 46, 255–266.
- Ghadirian, A. M., Marini, N., Jabalpurlawa, S., & Steiger, H. (1999). Seasonal mood patterns in eating disorders. General Hospital Psychiatry, 21, 354–359.
- Gleaves, D. H., & Eberenz, K. P. (1995). Correlates of dissociative symptoms among women with eating disorders. Journal of Psychiatric Research, 29, 417–426.
- Gleaves, D. H., Eberenz, K. P., & May, M. C. (1998). Scope and significance of posttraumatic symptomatology among women hospitalized for an eating disorder. International Journal of Eating Disorders, 24, 147–156.
- Gleaves, D. H., Lowe, M. R., Snow, A. C., Green, B. A., & MurphyEberenz, K. P. (2000). Continuity and discontinuity models of bulimia nervosa: A taxometric investigation. Journal of Abnormal Psychology, 109, 56–68.
- Godart, N. T., Flament, M. F., Lecrubier, Y., & Jeammet, P. (2000). Anxiety disorders in anorexia nervosa and bulimia nervosa: Comorbidity and chronology of appearance. European Psychiatry, 15, 38–45.
- Goldstein, H. J. (1981). Family factors associated with schizophrenia and anorexia nervosa. Journal of Youth and Adolescence, 10, 385–405.
- Grave,R.D.,Oliosi,M.,Todisco,P.,&Vanderlinden,J.(1997).Selfreported traumatic experiences and dissociative symptoms in obesewomenwithandwithoutbinge-eatingdisorder.EatingDisorders: The Journal of Treatment and Prevention, 5, 105–109.
- Grinspoon, S., Gulick, T., Askari, H., Landt, M., Vignati, L., Bowsher, R., Herzog, D., & Klibanski, A. (1996). Serum leptin levels in women with anorexia nervosa. Journal of Clinical Endocrinology and Metabolism, 81, 3861–3863.
- Gupta, M. A., & Johnson, A. M. (2000). Nonweight-related body image concerns among female eating-disordered patients and nonclinical controls: Some preliminary observations. International Journal of Eating Disorders, 27, 304–309.
- Hall, A., & Brown, L. B. (1983). A comparison of the attitudes of young anorexia nervosa patients and non-patients with those of their mothers. British Journal of Medical Psychology, 56, 39–48.
- Hall, A., Leibrich, J., Walkley, F., & Welch, G. (1986). Investigation of “weight pathology” of 58 mothers of anorexia nervosa patients and 204 mothers of schoolgirls. Psychological Medicine, 16, 71–76.
- Halmi, K. A., Sunday, S. R., Strober, M., Kaplan, A., Woodside, D. B., Fichter, M., Treasure, J., Berrettini, W. H., & Kaye, W. H. (2000). Perfectionism in anorexia nervosa: Variation by clinical subtype, obssessionality, and pathological behavior. American Journal of Psychiatry, 157, 1799–1805.
- Hebebrand, J., Blum, W. F., Barth, N., Coners, H., Englaro, P., Juul, A., Ziegler, A., Rascher, W., & Remschmidt, H. (1997). Leptin levels in patients with anorexia nervosa are reduced in the acute stage and elevated upon short-term weight restoration. Molecular Psychiatry, 2, 330–334.
- Herzog, D. B., Keller, M. B., Sacks, N. R., Yeh, C. J., & Lavori, P. W. (1992). Psychiatric comorbidity in treatment-seeking anorexics and bulimics. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 810–818.
- Hinney, A., Lentes, K. U., Rosenkrantz, K., Barth, N., Roth, H., Ziegler, A., Henninghausen, K., Coners, H., Wurmser, H., Romer, J. K., Winnikes, G., Mayer, H., Herzog, W., Lehmkuhl, , Poustka, F., Schmidt, M. H., Blum, W. F., Pirke, K. M., Schafer, H., Greschik, K. H., Remschmidt, H., & Hebebrand, J. (1997). Beta 3-adrenergic receptor allele distributions in children, adolescents and young adults with obesity, underweight or anorexia nervosa. International Journal of Obesity Related Metabolic Disorders, 21, 224–230.
- Hodes, M., & leGrange, D. (1993). Expressed emotion in the investigation of eating disorders: A review. International Journal of Eating Disorders, 13, 279–288.
- Hodges, E. L., Cochrane, C. E., & Brewerton, T. D. (1998). Family characteristics of binge-eating disorder patients. International Journal of Eating Disorders, 23, 145–151.
- Hoffman, G. W., Ellinwood, E. H., Rockwell, W. J., Herfkens, R. J., Nishita, J. K., & Guthrie, L. F. (1989). Cerebral atrophy in bulimia. Biological Psychiatry, 25, 894–902.
- Holderness, C., Brooks-Gunn, J., & Warren, M. (1994). Comorbidity of eating disorders and substance abuse: Review of the litertaure. International Journal of Eating Disorders, 16, 1–34.
- Hsu, L. K. G., & Sobkiewicz, T. A. (1991). Body image disturbance: Time to abandon the concept for eating disorders. International Journal of Eating Disorders, 10, 15–30.
- Humphrey, L. L. (1991). Object relations and the family system: An integrative approach to understanding and treating eating disorders. In C. Johnson (Ed.), Psychodynamic treatment of anorexia nervosa and bulimia (pp. 321–353). New York: Guilford Press.
- Jacobsin, R., & Robins, C. J. (1989). Social dependency and social support in bulimic and nonbulimic women. International Journal of Eating Disorders, 8, 665–670.
- Jimerson, D. C., Lesem, M. D., Kaye, W. H., & Brewerton, T. D. (1992). Low serotonin and dopamine metabolite concentrations in cerebrospinal fluid from bulimic patients with frequent binge episodes. Archives of General Psychiatry, 49, 132–138.
- Johnson, C. (1991). Treatment of eating-disordered patients with borderline and false-self/narcissistic disorders. In C. Johnson (Ed.), Psychodynamic treatment of anorexia nervosa and bulimia (pp. 165–193). New York: Guilford Press.
- Johnston, J. L., Leiter, L. A., Burrow, G. N., Garfinkel, P. E., & Anderson, G. H. (1984). Excretion of urinary catecholamine metabolites in anorexia nervosa: Effect on body composition and energy intake. American Journal of Clinical Nutrition, 40, 1001–1006.
- Katz, B. E., & Gleaves, D. H. (1996). Dissociative symptoms with eating disorders: Associated feature or artifact of a comorbid dissociative disorder. Dissociation, 9, 28–36.
- Kaye, W. H., Ebert, M. H., Raleigh, M. H., & Lake, R. (1984). Abnormalities in CNS monoamine metabolism in anorexia nervosa. Archives of General Psychiatry, 41, 350–355.
- Kaye, W. H., Frank, G. K. W., & McConaha, C. (1999). Altered dopamine activity after recovery from restricting-type anorexia nervosa. Neuropsychopharmacology, 21, 503–506.
- Kaye, W. H., Gendall, K. A., Fernstrom, M. H., Fernstrom, J. D., McConaha, C. W., & Weltzin, T. E. (2000). Effects of acute tryptophan depletion on mood in bulimia nervosa. Biological Psychiatry, 47, 151–157.
- Kaye, W. H., Greeno, C. G., Moss, H., Fernstrom, J. D., Fernstrom, M. H., Lilenfeld, L. R, Weltzin, T. E., & Mann, J. (1998). Alterations in serotonin activity and psychiatric symptoms after recovery from bulimia nervosa. Archives of General Psychiatry, 55, 927–935.
- Kaye, W. H., Gwirtsman, H. E., George, D. T., & Ebert, M. H. (1991). Altered serotonin activity in anorexia nervosa after longterm weight restoration. Does elevated cerebrospinal fluid 5hydroxyindoleacetic acid level correlate with rigid and obsessive behavior? Archives of General Psychiatry, 48, 556–562.
- Kaye, W. H., Gwirtsman, H. E., George, D. T., Jimenson, D. C., Ebert, M. H., & Lake, R. (1990). Disturbances of noradrenergic systems in normal weight bulimia: Relationship to diet and menses. Biological Psychiatry, 27, 4–21.
- Kendler, K. S., Maclean, C., Neale, M. C., Kessler, R. C., Heath, A. C., & Eaves, L. J. (1991). The genetic epidemiology of bulimia nervosa. American Journal of Psychiatry, 148, 1627–1637.
- Keys, A., Brozek, J., Henschel, A., Mickelson, O., & Taylor, H. (1950). The biology of human starvation. Minneapolis: University of Minnesota Press.
- Kog, E., Vertommen, H., & Vandereycken, W. (1987). Minuchin’s psychosomatic family model revised: Aconcept validation study using a multitrait-multimethod apporach. Family Process, 26, 235–253.
- Lake, A. J., Staiger, P. K., & Glowinski, H. (2000). Effect of western culture on women’s attitudes to eating and perceptions of body shape. International Journal of Eating Disorders, 27, 83–89.
- Lambe, E. K., Katzman, D. K., Mikulis, D. J., Kennedy, S. H., & Zipursky, R. B. (1997). Cerebral gray matter volume deficits after weight recovery from anorexia nervosa. Archives of General Psychiatry, 54, 537–542.
- Lauer, C. J., Gorzewski, B., Gerlinghoff, M., Backmund, H., & Zihl, J. (1999). Neuropsychological assessments before and after treatment in patients with anorexia nervosa and bulimia nervosa. Journal of Psychiatry Research, 33, 129–138.
- Lee, S., Ho, P., & Hsu, L. K. G. (1993). Fat phobic and non-fat phobic anorexia nervosa: A comparative study of 70 Chinese patients in Hong Kong. Psychological Medicine, 23, 999–1017.
- Lehoux, P., Steiger, H., & Jabalpurlawa, S. (2000). State/trait distinctions in bulimic syndromes. International Journal of Eating Disorders, 27, 36–42.
- Levitan, R. D., Kaplan, A. S., Brown, G. M., Joffe, R. T., Levitt, A. J., Vaccarino, F. J., & Kennedy, S. (1997). Low plasma cortisol in bulimia nervosa patients with reversed neurovegetative symptoms of depression. Biological Psychiatry, 41, 366– 368.
- Levitan, R. D., Kaplan,A. S., Levitt,A. J., & Joffe, R.T. (1994). Seasonal fluctuations in mood and eating behavior in bulimia nervosa. International Journal of Eating Disorders, 16, 295–299.
- Levitan, R., Maselis, M., Kaplan, A., Basile, V., Kennedy, S., Lam, R., Vaccarino, F., Macciardi, F., & Kennedy, J. (2000, May). Serotonin genetic polymorphism in bulimia nervosa and seasonal affective disorder. Paper presented at the Ninth International Conference on Eating Disorders, New York.
- Lilenfeld, L. R., Kaye, W. H., Greeno, C. G., Merikangas, K. R., Plotnicov, K., Pollice, C., Rao, R., Strober, M., Bulik, C. M., & Nagy, L. (1997). Psychiatric disorders in women with bulimia nervosa and their first-degree relatives: Effects of comorbid substance dependence. International Journal of Eating Disorders, 22, 253–264.
- Lilenfeld, L. R., Kaye, W. H., Greeno, C. G., Merikangas, K. R., Plotnicov, K., Pollice, C., Rao, R., Strober, M., Bulik, C. M., & Nagy, L. (1998). A controlled family study of anorexia nervosa and bulimia nervosa: Psychiatric disorders in first-degree relatives and effects of proband comorbidity. Archives of General Psychiatry, 55, 603–610.
- Lilenfeld, L. R., Stein, D., Bulik, C. M., Strober, M., Plotnicov, K., Pollice, C., Rao, R., Merikangas, K. R., Nagy, L., & Kaye, W. H. (2000). Personality traits among currently eating disordered, recovered and never ill first-degree female relatives of bulimic and control women. Psychology Medicine, 30, 1399–1410.
- Lippincott, J. A., & Hwang, H. S. (1999). On cultural similarities in attitudes toward eating of women students in Pennsylvania and South Korea. Psychological Reports, 85, 701–702.
- Logue, C. M., Crowe, R. R., & Bean, J.A. (1989).Afamily study of anorexia nervosa. British Journal of Psychiatry, 30, 179–188.
- Lucas, A. R., Crowson, C. S., O’Fallon, W. M., & Melton, L. J. (1999). The ups and downs of anorexia nervosa. International Journal of Eating Disorders, 26, 397–405.
- Marcus,M.D.,Wing,R.R.,&Hopkins,J.(1988).Obesebingeeaters: Affect, cognitions and response to behavioral weight control. Journal of Consulting and Clinical Psychology, 13, 433–439.
- Matsunaga, H., Kaye, W. H., McConaha, C., Plotnicov, K., Pollice, C., & Rao, R. (2000). Personality disorders among subjects recovered from eating disorders. International Journal of Eating Disorders, 27, 353–357.
- Matsunaga, H., Kaye, W. H., McConaha, C., Plotnicov, K., Pollice, C., Rao, R., & Stein, D. (1999). Psychopathological characteristics of recovered bulimics who have a history of physical or sexual abuse. Journal of Nervous and Mental Disease, 187, 472–477.
- Matsunaga, H., Kiriike, N., Iwasaki, Y., Miyata, A., Matsui, T., Nagata, T., Yamagami, S., & Kaye, W. H. (2000). Multiimpulsivity among bulimic patients in Japan. International Journal of Eating Disorders, 27, 348–352.
- Matsunaga, H., Kiriike, N., Miyata, A., Iwasaki, Y., Matsui, T., Fulimtot, K., Kasai, S., & Kaye, W. H. (1999). Prevalence and symptomatology of comorbid obsessive-compulsive disorder among bulimic patients. Psychiatry and Clinical Neurosciences, 54, 661–666.
- Mehler, P. S., Eckel, R. H., & Donahoo, W. T. (1999). Leptin levels in restricting and purging anorectics. International Journal of Eating Disorders, 26, 189–194.
- Miller, D. A., McCluskey-Fawcett, K., & Irving, L. M. (1993). Correlates of bulimia nervosa: Early mealtime experiences. Adolescence, 28, 621–635.
- Mitchell, J. E., & Eckert, E. D. (1987). Scope and significance of eating disorders. Journal of Consulting and Clinical Psychology, 55, 628–634.
- Mitchell, J. E., Mussell, M. P., Peterson, C. B., Crow, S., Wonderlich, S. A., Crosby, R. D., Davis, T., & Weller, C. (1999). Hedonics of binge eating in women with bulimia nervosa and binge eating disorder. International Journal of Eating Disorders, 26, 165–170.
- Monteleone, P., Brambilla, F., Bortolototti, F., LaRocca, A., & Maj, M. (1998). Prolactin response to d-fenfluramine is blunted in people with anorexia nervosa. British Journal of Psychiatry, 172, 438–442.
- Monteleone, P., Di Lieto, A., Tortorella, A., Longobardi, N., & Maj, M. (2000). Circulating leptin in patients with anorexia nervosa, bulimia nervosa or binge-eating disorder: Relationship to body weight, eating patterns, psychopathology and endocrine changes. Psychiatry Research, 94, 121–129.
- Moreno, J. K., Selby, M. J., & Neal, S. (1998). Psychopathology in sexually abused and non-sexually abused eating-disordered women. Psychotherapy in Private Practice, 17, 1–9.
- Murnen, S. K., & Smolak, L. (1997). Femininity, masculinity, and disordered eating: A meta-analytic review. International Journal of Eating Disorders, 22, 231–242.
- Newton, J. R., Freeman, C. P., & Munro, J. (1993). Impulsivity and dyscontrol in bulimia nervosa: Is impulsivity an independent phenomenon or a marker of severity? Acta Psychiatrica Scandinavia, 87, 389–394.
- Nielsen, D., Virkkunen, M., Lappalainen, J., Eggert, M., Brown, G., Long, J., Goldman, D., & Linnoila, M. (1998). A tryptophan hydroxylase gene marker for suicidality and alcoholism. Archives of General Psychiatry, 55, 593–602.
- Nilsson, E. W., Gillberg, C., Gillberg, I. C., & Rastam, M. (1999). Ten-year follow-up of adolescent onset anorexia nervosa: Personality disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 1389–1395.
- Norman, D. K., Blais, D., & Herzog, D. (1993). Personality characteristics of eating-disordered patients as identified by the Millon Clinical Multiaxial inventory. Journal of Personality Disorders, 7, 1–9.
- Olivardia, R., Pope, H. G., Jr., & Hudson, J. I. (2000). Muscle dysmorphia in male weightlifters: A case-control study. American Journal of Psychiatry, 157, 1291–1296.
- Pate, J. E., Pumariega, A. J., Hester, C., & Garner, D. M. (1992). Cross-cultural patterns in eating disorders: A review. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 802–809.
- Pirke, K. M., Kellner, M. B., Frie, E., Krieg, J.-C., & Fichter, M. M. (1994). Satiety and cholecystokinin. International Journal of Eating Disorders, 15, 63–69.
- Polivy, J., & Herman, C. P. (1985). Dieting and binging: A causal analysis. American Psychologist, 40, 193–201.
- Polivy, J., & Herman, C. P. (1993). Etiology of binge eating: Psychological mechanisms. In C. G. Fairbairn & G. T. Wilson (Eds.), Binge eating: Nature, assessment, and treatment (pp. 173–205). NewYork: Guilford Press.
- Pruitt,J.A.,Kappins,R.E.,&Gorman,P.W.(1992).Bulimiaandfear of intimacy. Journal of Clinical Psychology, 48, 472–476.
- Råstam, M. (1992). Anorexia nervosa in 51 Swedish adolescents: Premorbid problems and comorbidity. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 819–829.
- Rhea, D. J. (1999). Eating disorder behaviors of ethnically diverse urban female adolescent athletes and non-athletes. Journal of Adolescence, 22, 379–388.
- Rhodes, B., & Kroger, J. (1992). Parental bonding and separationindividuationdifficultiesamonglateadolescenteatingdisordered women. Child Psychiatry & Human Development, 22, 249–263.
- Rosenvinge, J. H., Martinussen, M., & Ostensen, E. (2000). The comorbidity of eating disorders and personality disorders: A metaanalytic review of studies published between 1983 and 1998. Eating and Weight Disorders, 5, 52–61.
- Ross, H. E., & Ivis, F. (1999). Binge eating and substance use among male and female adolescents. International Journal of Eating Disorders, 26, 245–260.
- Schmidt, U., Humfress, H., & Treasure, J. (1997). The role of general family environment and sexual and physical abuse in the origins of eating disorders. European Eating Disorders Review, 5, 184–207.
- Schukit, M. A., Tipp, J. E., Anthenelli, R. M., Bucholz, K. K., Hesselbrock, V. M., & Nurnberger, J. I., Jr. (1996). Anorexia nervosa and bulimia nervosa in alcohol-dependent men and women and their relatives. American Journal of Psychiatry, 153, 74–82.
- Sights, J. R., & Richards, H. C. (1984). Parents of bulimic women. International Journal of Eating Disorders, 3, 3–13.
- Sitnick,T.,&Katz,J.(1984).Astudyofsexroleidentityandanorexia nervosa. International Journal of Eating Disorders, 3, 81–87.
- Smith, K. A., Fairburn, C. G., & Cowen, P. J. (1999). Symptomatic relapse in bulimia nervosa following acute tryptophan depletion. Archives of General Psychiatry, 56, 171–176.
- Sohlberg, S., & Strober, M. (1994). Personality in anorexia nervosa: An update and a theoretical integration. Acta Psychiatrica Scandinavica, 89(Suppl. 378), 1–15.
- Spitzer, R. L., Devlin, M., Walsh, B. T., Hasin, D., Wing, R., Marcus, M., Stunkard, A., Wadden, T., Yanovski, S., Agras, S., Mitchell, J., & Nonas, C. (1992). Binge eating disorder: Amultisite field trial of diagnostic criteria. International Journal of Eating Disorders, 11, 191–203.
- Srinivasagam, N. M., Kaye, W. H., Plotnicov, K. H., Greeno, C., Weltzin, T. E., & Rao, R. (1995). Persistent perfectionism, symmetry, and exactness after long-term recovery from anorexia nervosa. American Journal of Psychiatry, 152, 1630–1634.
- Steiger, H., Gauvin, L., Israel, M., Koerner, Ng Ying Kin, N. M. K., Paris, J., & Young, S. N. (2001). Association of serotonin and cortisol indices with childhood abuse in bulimia nervosa. Archives of General Psychiatry, 58, 837–843.
- Steiger, H., Gauvin, L., Jabalpurlawa, S., Séguin, J. R., & Stotland, S. (1999). Hypersensitivity to social interactions in bulimic eating syndromes: Relationship to binge-eating. Journal of Consulting and Clinical Psychology, 67, 765–775.
- Steiger, H., Koerner, N. M., Engleberg, M., Israel, M., Ng Ying Kin, N. M. K., & Young, S. N. (2001). Self-destructiveness and serotonin function in bulimia nervosa. Psychiatry Research, 103, 15–26.
- Steiger, H., Leonard, S., Ng Ying Kin, N. M. K., Ladouceur, C., Ramdoyal, D., & Young, S. N. (2000). Childhood abuse and tritiated paroxetine binding in bulimia nervosa. Journal of Clinical Psychiatry, 61, 428–435.
- Steiger, H., Van der Feen, J., Goldstein, C., & Leichner, P. (1989). Defense styles and parental bonding in eating-disordered women. International Journal of Eating Disorders, 8, 131–140.
- Stickney, M. I., Miltenberger, R. G., & Wolff, G. (1999). A descriptive analysis of factors contributing to binge eating. Journal of Behavior Therapy and Experimental Psychiatry, 30, 177–189.
- Striegel-Moore, R. H., Silberstein, L. R., & Rodin, J. (1986). Toward an understanding of risk factors for bulimia. Amercan Psychologist, 41, 246–248.
- Striegel-Moore, R. H., Wilfley, D. E., Pike, K. M., Dohm, F. A., & Fairburn, C. G. (2000). Recurrent binge eating in blackAmerican women. Archives of Family Medicine, 9, 83–87.
- Striegel-Moore, R. H., Wilson, G. T., Wilfley, D. E., Elder, K. A., & Brownell, K. D. (1998). Binge eating in an obese community sample. International Journal of Eating Disorders, 23, 27–37.
- Strober, M. (1991). Disorders of the self in anorexia nervosa: An organismic-developmental paradigm. In C. Johnson (Ed.), Psychodynamic treatment of anorexia nervosa and bulimia (pp. 354–372). New York: Guilford Press.
- Strober, M., Freeman, R., Lampert, C., Diamond, J., & Kaye, W. (2000). Controlled family study of anorexia nervosa and bulimia nervosa: Evidence of shared liability and transmission of partial syndromes. American Journal of Psychiatry, 157, 393–401.
- Strober, M., Lampert, C., Morrell, W., Burroughs, J., & Jacobs, C. (1990).Acontrolledfamilystudyofanorexianervosa:Evidenceof familialaggregationandlackofsharedtransmissionwithaffective disorders. International Journal of Eating Disorders, 9, 239–253.
- Szmukler,G.I.,Andrewes,D.,Kingston,K.,Chen,L.,Stargatt,R.,& Stanley, R. (1992). Neuropsychological impairment in anorexia nervosa: Before and after refeeding. Journal of Clinical and Experimental Neuropsychology, 14, 347–352.
- Thornton, C., & Russell, J. (1997). Obsessive-compulsive comorbidity in the dieting disorders. International Journal of Eating Disorders, 21, 83–87.
- Tobin, D. L., Griffing, A., & Griffing, S. (1997). An examination of subtype criteria for bulimia nervosa. International Journal of Eating Disorders, 22, 179–186.
- Toner, B. B., Garfinkel, P. E., & Garner, D. M. (1987). Cognitive style of patients with bulimic and diet-restricting anorexia nervosa. American Journal of Psychiatry, 144, 510–512.
- Treasure, J. L., & Holland, A. J. (1989). Genetic vulnerability to eating disorders: Evidence from twin and family studies. In H. Remschmidt & M. H. Schmidt (Eds.), Anorexia nervosa (pp. 59–68). Toronto, Ontario, Canada: Hogrefe & Huber.
- Tuschen-Caffier, B., & Vogele, C. (1999). Psychological and physiological reactivity to stress: An experimental study on bulimic patients, restrained eaters and controls. Psychotherapy and Psychosomatics, 68, 333–340.
- Vanderlinden, J., Vandereycken, W., van Dyk, R., & Vertommen, H. (1993). Dissociative experiences and trauma in eating disorders. International Journal of Eating Disorders, 13, 187–194.
- Vitousek, K., & Manke, F. (1994). Personality variables and disorders in anorexia nervosa and bulimia nervosa. Journal of Abnormal Psychology, 103, 137–147.
- von Ranson, K. M., Kaye, W. H., Weltzin, T. E., Rao, R., & Matsunaga, H. (1999). Obsessive-compulsive disorder symptoms before and after recovery form bulimia nervosa. American Journal of Psychiatry, 156, 1703–1708.
- Wade, T. D., Bulik, C. M., Neale, M., & Kendler, K. S. (2000). Anorexia nervosa and major depression: Shared genetic and environmental risk factors. American Journal of Psychiatry, 157, 469–471.
- Wakeling, A. (1996). Epidemiology of anorexia nervosa. Psychiatry Research, 62, 3–9.
- Waller, J. V., Kaufman, M. R., & Deutsch, F. (1940). Anorexia nervosa: Apsychosomatic entity. Psychosomatic Medicine, 2, 3–16.
- Walters, E. E., & Kendler, K. S. (1995). Anorexia nervosa and anorexic-like syndromes in a population-based female twin sample. American Journal of Psychiatry, 152, 64–71.
- Ward, A., Brown, N., Lightman, S., Campbell, I. C., & Treasure, J. (1998). Neuroendocrine, appetitive and behavioral responses to d-fenfluramine in women recovered from anorexia nervosa. British Journal of Psychiatry, 172, 351–358.
- Ward, A., Ramsay, R., & Treasure, J. (2000). Attachment research in eating disorders. British Journal of Medical Psychology, 73, 35–51.
- Ward, A., Ramsay, R., Turnbull, S., Benedettini, M., & Treasure, J. (2000). Attachment patterns in eating disorders past in the present. International Journal of Eating Disorders, 28, 370–376.
- Webster, J. J., & Palmer, R. L. (2000). The childhood and family background of women with clinical eating disorders: A comparison with women with major depression and women without psychiatric disorder. Psychological Medicine, 30, 53–60.
- Weizman, R., Carmi, M., Tyano, S., Apter, A., & Rehavi, M. (1986). High affinity [3H]imipramine binding and serotonin uptake to platelets of adolescent females suffering from anorexia nervosa. Life Sciences, 38, 1235–1242.
- Wertheim, E. H. (1999). Relationships among adolescent girls’ eating behvaiors and their parents’ weight-related attitudes and behaviors. Sex Roles, 41, 169–187.
- Whelan, E., & Cooper, P. J. (2000). The association between childhood feeding problems and maternal eating disorder: A community study. Psychological Medicine, 30, 69–77.
- Widiger, T. A., & Sankis, L. M. (2000). Adult psychopathology: Issues and controversies. Annual Review of Psychology, 51, 377–404.
- Wiederman, M. W., & Pryor, T. (1996). Multi-impulsivity among women with bulimia nervosa. International Journal of Eating Disorders, 20(4), 359–365.
- Windauer, U., Lennerts, W., Talbot, P., Touyz, S., & Beumont, P. (1993). How well are “cured” anorexia nervosa patients? An investigation of 16 weight-recovered anorexic patients. British Journal of Psychiatry, 163, 195–200.
- Wolfe, B. E., Jimerson, D. C., & Levine, J. M. (1994). Impulsivity ratings in bulimia nervosa: Relationship to binge eating behaviors. International Journal of Eating Disorders, 15, 289–292.
- Wonderlich, S. A., Brewerton, T. D., Jocic, Z., Dansky, B., & Abbott, D. W. (1997). Relationship of childhood sexual abuse and eating disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 1107–1115.
- Zaider, T. I., Johnson, J. G., & Cockell, S. J. (2000). Psychiatric comorbidity associated with eating disorder symptomatology among adolescents in the community. International Journal of Eating Disorders, 28, 58–67.




