View sample food and fluid intake research paper. Browse research paper examples for more inspiration. If you need a psychology research paper written according to all the academic standards, you can always turn to our experienced writers for help. This is how your paper can get an A! Feel free to contact our writing service for professional assistance. We offer high-quality assignments for reasonable rates.
Ingestive behaviors play primary roles in the maintenance of fluid homeostasis and energy balance. Feeding and drinking are intermittent behaviors that both renew and anticipate depletions. Their controls are complex and redundant. Early views of homeostasis focused on physiological mechanisms in the body for maintaining constant internal states. Claude Bernard (1859) and Walter Cannon (1932) put forth the concept of homeostasis as the maintenance of the internal milieu within fixed limits through the coordination of controlled physiological processes. Although Bernard and Cannon recognized a role for behavior in these processes, Curt Richter (1943) expanded the view of physiological defenses of the internal milieu to include behavior as a major regulating factor. For Richter, the role of behavioral regulators in homeostasis was broadly conceived and studied. A focus on the behavior itself has revealed that both food intake and water intake have multiple levels of control that interact to ensure that the body has adequate hydration and energy stores.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
In the following sections we focus on the major physiological systems involved in the controls of food and fluid intake, identifythesystemsthatmonitoravailablenutrientandhydrationalstores,discusssystemsthatrespondtotheconsequences of food and fluid intake, and identify how interactions among these systems produce behavioral outcomes that result in adequate and appropriate food and fluid intake.
Food Intake and Energy Balance
What and how much we eat depend on a wide variety of factors. These include factors related to palatability or taste, learning, social and cultural influences, environmental factors, and physiological controls. The relative contributions of these many factors to feeding control vary across species and testing situations. We concentrate on the roles of three interacting systems important in feeding control. These are systems that mediate (a) signals related to metabolic state, especially to the degree of adiposity; (b) affective signals related to taste and nutritional consequences that serve to reinforce aspects of ingestive behavior; and (c) signals that arise within an individual meal and produce satiety. We also identify the important interactions among these systems that permit the overall regulation of energy balance.
Metabolic Signals and Their Mediation
Arole for signals related to the availability of energy stores in the control of food intake has long been postulated. Depletionrepletion models tied to carbohydrate availability (Mayer, 1953) and fat stores (Kennedy, 1953) have been proposed. Although neither of these individual models is sufficient to explain the multiple variations in food intake that occur throughout the life cycle, evidence for food intake controls that depend upon monitoring fuel availability and utilization is strong. Administration of metabolic inhibitors that act on differing metabolic pathways stimulate food intake. For example, treatment with either 2-deoxy-D-methyl glucose (2-DG), which inhibits glucose utilization, or methyl palmoxirate, which suppresses fatty acid oxidation, stimulates food intake in satiated animals. Sites of action in both the liver and brain have been identified (Ji, Graczyk-Milbrandt, & Friedman, 2000; Ritter, Dinh, & Zhang, 2000).
Alterations in circulating glucose have been tied to meal initiation in both rats and humans. Campfield and colleagues have shown that transient declines and partial restorations in blood glucose levels reliably predict meal initiation (Campfield & Smith, 1986; Melanson, Westerterp-Plantenga, Saris, Smith, & Campfield, 1999). Demonstrations that experimentally induced declines in blood glucose can result in meal initiation suggest that the relationship may be more than correlational (Smith & Campfield, 1993).
Studies of genetic obesity models had long suggested the importance of circulating factors in overall body weight control. Having identified two different mutations in mice that led to obesity, Coleman (1973) conducted parabiotic experiments involving two strains of obese (obese, ob/ob, and diabetic, db/db) and normal mice in which the blood supply between the two mice in a parabiotic pair was shared. The results showed that when paired with db/db mice, ob/ob mice became hypoglycemic, lost weight, and eventually died—asimilar response to that seen in normal mice combined with db/db mice. In contrast, when combined with normal mice, ob/ob mice gained less weight than they otherwise would but were fully viable. The results led Coleman to conclude that the ob/ob mouse lacked a circulating satiety factor that, in its absence, results in hyperphagia and obesity whereas the db/db mouse produced the factor but lacked the ability to respond appropriately to it.
The positional cloning of leptin as the product of the ob gene (Zhang et al., 1994) and subsequent identification of the leptin receptor as the product of the db gene (Chua et al., 1996; Tartaglia et al., 1995) has provided the basis for Coleman’s observations. Leptin not only normalizes food intake and body weight in ob/ob mice but also reduces food intake in normal mice and rats (Campfield, Smith, Guisez, Devos, & Burn, 1995; Seeley et al., 1996). Leptin is produced in white adipose tissue, and circulating leptin levels correlate positively with adipose mass as animals and humans become obese (Maffei et al., 1995). Thus, leptin signals the availability of body energy stores.
Leptin is currently viewed as the major adiposity factor important for the long-term control of energy balance. Leptin receptors are members of the cytokine-receptor superfamily. Multiple leptin receptor isoforms that arise from differential splicing have been identified. The predominant form of the leptin receptor is the short form (Ob-Ra), which is widely expressed in multiple areas including the choroid plexus and brain microvasculature (Bjorbaek et al., 1998). These binding sites are likely to function as a part of a saturable transport system for circulating leptin to gain access into the brain.Thelong form of the leptin receptor (Ob-Rb) can activate Janus kinase (JAK) signal transduction andsignal transducers and activators of transcription (STAT) elements to mediate leptin’s cellular actions (Bjorbaek, Uotoni, da Silva, & Flier, 1997). Ob-Rb is highly expressed within hypothalamic nuclei with identified roles in energy balance. Highest concentrations of the long form of the leptin receptor are found within the arcuate, paraventricular, and dorsomedial hypothalamic nuclei as well as within the lateral hypothalamus (LH; Elmquist, Bjorbaek, Ahima,Flier,&Saper,1998).InteractionsofleptinwithOb-Rb receptors within these hypothalamic nuclei result in the activation or inactivation of hypothalamic pathways containing various orexigenic and anorexigenic peptides (M. W. Schwartz, Seeley, Campfield, Burn, & Baskin, 1996).
Hypothalamic Systems Involved in Food Intake
The role of the hypothalamus in food intake control was established through the classic experiments of Heatherington and Ranson (1940) and Anand and Brobesck (1951). Using stereotaxically placed lesions, they demonstrated that bilateral lesions of the medial hypothalamus resulted in hyperphagia and obesity whereas lesions of the LH produced profound anorexia and weight loss. Subsequent work demonstrated that stimulation of these hypothalamic regions had the opposite effects. Medial hypothalamic stimulation inhibited food intake whereas stimulation of the LH produced food intake. Results such as these led Stellar (1954) to propose the classic dual center hypothesis for the role of the hypothalamus in food intake. The ventromedial region (VMH) was viewed as a satiety center, and the LH was viewed as a feeding center.
The roles of various hypothalamic nuclei in food intake are now much better understood, and many of the peptide neurotransmitters through which these actions are mediated have been identified. Table 11.1 depicts the variety of the hypothalamic peptides that have effects on food intake. These may be broadly classified as falling into two categories: orexigenic, or those that stimulate or increase food intake, and anorexigenic, or those that decrease food intake.
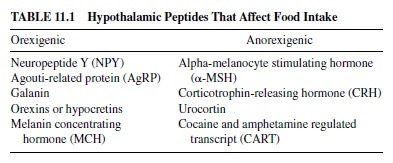
Among the orexigenic peptides, the one that has received the most attention is neuropeptide Y (NPY). Intracerebroventricular or direct hypothalamic injection of NPY potently stimulates feeding (Clark, Kalra, Crowley, & Kalra, 1984; Morley, Levine, Gosnell, Kneip, & Grace, 1987; Stanley, Krykouli, Lampert, & Leibowitz, 1986), and repeated or chronic NPY administration results in obesity (Stanley et al., 1986; Zarjevski, Cusin, Vetter, Rohner-Jeanrenaud, & Jeanrenaud, 1993). Hypothalamic NPY gene expression and secretion increase in response to food deprivation (Kalra, Dube, Sahu, Phelps, & Kalra, 1991; White & Kershaw, 1989) or exercise (Lewis et al., 1993) and decrease in response to overconsumption of a highly palatable high-energy diet (Widdowson et al., 1999). Cell bodies of neurons expressing NPY are found in multiple hypothalamic nuclei including the arcuate and dorsomedial hypothalamic nuclei (Chornwall et al., 1985). Important projection sites for these neurons in mediating the feeding stimulatory actions of NPY are the paraventricular nucleus andperifornicalregionoftheLH(Stanley&Leibowitz,1985; Stanley, Magdalin, Seirafi, Thomas, & Leibowitz, 1993). Whereas chronic treatment with NPY results in obesity, absence of NPYor its receptors does not result in the absence of food intake or wasting. Murine knockout models that do not express NPY or NPY receptors are viable (Erikson, Clegg, & Palmiter, 1996; Marsh, Hollopeter, Kafer, & Palmiter, 1998; Pedrazzini et al., 1998). Rather than suggesting that NPYdoes notplayaroleinfoodintakecontrolandenergybalance,these results should be interpreted as suggesting that there are multiple redundant systems available for stimulating food intake and that the absence of one is not sufficient to block this critical behavior significantly.
Other hypothalamic orexigenic peptides have been identified and their roles in food intake investigated. These include galanin, hypocretin 1 and 2 (also known as orexin A and B) and melanin concentrating hormone (MCH). Galanin stimulates food intake following either intraventricular or hypothalamic administration (Crawley et al., 1990; Kyrkouli, Stanley, & Leibowitz, 1986). Galanin levels and mRNA expression are elevated in rats consuming a high-fat diet but do not appear to be affected by food deprivation (Beck, Burlet, Nicolas, & Burlet, 1993; Mercer, Lawrence, & Atkinson, 1996). Whereas galanin antagonists block the actions of exogenous galanin on food intake, little effect of the antagonists alone have been demonstrated (Crawley, 1999).
Hypocretin 1 and 2 (i.e., orexin Aand B) are recently identified peptides that are coded from same prepro-mRNA (Sakurai et al., 1998). Both compounds increase food intake when centrally administered, but orexin A is much more potent (Sakurai et al., 1998; Sweet, Levine, Billington, & Kotz, 1999). Orexin-containing neurons are found in the perifornical area of the hypothalamus and project throughout the hypothalamus (Peyron et al., 1998). Prepro-orexin expression is increased in response to deprivation (Lopez et al., 2000), and administration of an orexin A antagonist has been demonstrated to inhibit food intake, suggesting a role for endogenous orexin A in food intake control (Haynes et al., 2000).
Intraventricular MCH administration increases food intake in a dose-related fashion in short-term tests but does not alter 24-hr food intake, and chronic administration does not result in significant weight gain (Rossi et al., 1997). MCH expression is increased in obesity, and levels are modulated by fasting (Qu et al., 1996). MCH neurons in the LH are a distinct population from those expressing hypocretin/orexin; like orexin neurons, however, they are innervated by arcuate nucleus NPY-containing fibers (Broberger, DeLecea, Sutcliffe, & Hokfelt, 1998).
Endogenous melanocortins have both feeding-stimulatory and feeding-inhibitory actions. Pro-opiomelanocortin (POMC) is the precursor for a variety of peptides. Among these is the anorexigenic peptide alpha-melanocyte stimulating hormone (-MSH). Central administration of -MSH or synthetic melanocortin agonists potently inhibits food intake (Benoit et al., 2000; Fan, Boston, Kesterson, Hruby, & Cone, 1997). The feeding inhibitory actions of central melanocortins are mediated primarily through interactions with the melanocortin-4 (MC-4) receptors. Within the hypothalamus, POMC expression is limited to the arcuate nucleus. Arcuate POMC expression decreases with food deprivation (Kim, Welch, Grace, Billington, & Levine, 1996) and increases with overfeeding (Hagan et al., 1999), suggesting a regulatory role for this peptide in feeding control. Important roles for melanocortin signaling in energy balance are demonstrated in experiments examining the effects of POMC (Yaswen, Diehl, Brennan, & Hochgeschwender, 1999) or MC-4 receptor (Huszar et al., 1997) knockouts. Unlike many other peptide-signaling systems that affect food intake, the melanocortin system has an endogenous receptor antagonist that is orexigenic. Agouti-related protein (AgRP) is localized to the arcuate nucleus, and its expression is up-regulated by fasting (Hahn, Breininger, Baskin, & Schwartz, 1998). AgRP or synthetic melanocortin antagonists increase food intake when administered centrally, and their effects are long lasting (Fan et al., 1997).
Other hypothalamic anorexigenic peptides have been identified. These include corticotrophin-releasing hormone (CRH), urocortin, and cocaine and amphetamine regulated transcript (CART). Central administration of each of these peptides decreases food intake. The expression of each is decreased in response to food deprivation and increased in states of positive energy balance.
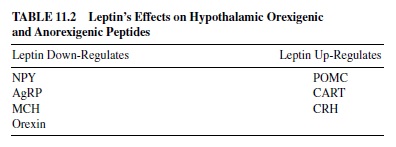
A number of these hypothalamic orexigenic and anorexigenic peptides have been implicated in the actions of leptin. Thus, a primary site of leptin action is within the arcuate nucleus. Ob-Rb receptors are localized to two distinct arcuate nucleus neuronal populations. Within the medial arcuate, Ob-Rb is expressed in cells that also express the orexigenic peptides NPY and AgRP. In more lateral aspects of the arcuate, Ob-Rb is expressed in cells containing the anorexigenic peptides CART and the anorexigenic peptide precursor POMC. Leptin up-regulates POMC- and CART-containing neurons and down-regulates NPY- and AgRP-containing neurons resulting in increased anorexigenic and decreased orexigenic activity (Kristensen et al., 1998; M. J. Schwartz et al., 1996, 1997). Leptin also affects the activity of MCH (Sahu, 1998), orexins (Beck & Richy, 1999) and CRH (van Dijk et al., 1999), down-regulating the expression of the orexigenic peptides and up-regulating the activity of CRH. Thus, as shown in Table 11.2, many of these hypothalamic signaling pathways are responsive to the overall level of adiposity as reflected by circulating leptin levels.
Although leptin is the adiposity signal that has received the most attention, insulin also acts in the hypothalamus as an adiposity signal. Insulin is secreted from pancreatic beta cells rather than adipose tissue. However, insulin levels increase with increased adiposity in response to growing insulin resistance. Insulin is transported from the circulation into the brain, and insulin receptors are localized to the hypothalamus with a high concentration in the arcuate nucleus (Corp et al., 1986). Central insulin inhibits food intake (Woods, Lotter, McKay, & Porte, 1979) and decreases NPY mRNA expression (M. W. Schwartz et al., 1992).
Whereas the hypothalamus has been the main focus of study for anorexigenic and orexigenic peptides, a number of these also have ingestive effects when delivered to the dorsal hindbrain. Thus, fourth-cerebroventricular administration of NPY (Corp, Melville, Greenberg, Gibbs, & Smith, 1990) or a melanocortin antagonist (Grill, Ginsburg, Seeley, & Kaplan, 1998) potently increases food intake, whereas a melanocortin agonist (Grill et al., 1998), CART (Aja, Sahandy, Ladenheim, Schwartz, & Moran, 2001), and urocortin (Grill, Markison, Ginsberg, & Kaplan, 2000) inhibit food intake when administered at this site. These hindbrain actions suggest that the central feeding regulatory system is a distributed one. How these hindbrain and hypothalamic systems interact with one another remains to be determined.
The Role of Reward in Food Intake Control
Taste and palatability play major roles in dietary choices and in the amount of a particular food that is consumed. The effects of taste on ingestion are best demonstrated under conditions in which the feedback effects of postingestional consequences are minimized. A number of paradigms that specifically assess the effects of palatability on ingestion have been commonly used. The first of these is the sham feeding paradigm in which animals have an esophageal or gastric fistula so that consumed liquid nutrients drain out of the fistula and do not accumulate in the stomach. Such a preparation was first employed by Pavlov (1910). Pavlov demonstrated that dogs with open esophageal fistulas did not develop satiety but continued to eat for hours. The sham feeding paradigm has clearly demonstrated the important role of orosensory stimuli in ingestion. Increasing the concentration of saccharide solutions or oil emulsions increases the amount consumed in a linear fashion over extensive concentration ranges (Grill & Kaplan, 1992; Mook, 1963; Weingarten & Watson, 1982).
A second method for assessing the effects of palatability on ingestion involves examining rates of ingestion when access is limited to a brief time period or examining ingestion rates at the very beginning of an ingestive bout. Both of these allow ingestion to be monitored at times during which the inhibitory effects of postoral feedback are minimized. In such tests, increasing concentrations of sugars or adding saccharin to sugar solutions can be shown to produce more rapid rates of licking in rats (Breslin, Davis, & Rosenak, 1996; Davis & Levine, 1977).
The effects of palatability on ingestion have both opioid and dopaminergic mediations. It has long been known that opiate agonists can increase feeding whereas antagonists decrease food intake. The effects of opioid ligands on ingestion appear to occur through alterations in palatability. Morphine enhances the intake of preferred over nonpreferred diets (Gosnell, Krahn, & Majchrzak, 1990) and enhances hedonic responses to sweet solutions as measured in taste reactivity tests (Doyle, Berridge, & Gosnell, 1993). In contrast, administration of the opiate antagonist naloxone specifically reduces the intake of a preferred diet while not affecting the intake of a nonpreferred diet in a choice paradigm in 24-hr deprived rats (Glass et al., 1996).
Although there has been significant interest in the hypothesis that opioids specifically affect the intake of fats deriving from studies demonstrating specific increases or decreases in fat intake with morphine or naloxone in nutrient selfselection paradigms (Marks-Kaufman & Kanarek, 1990), analyses of baseline nutrient preferences have indicated that morphine stimulates fat intake in fat-preferring rats and carbohydrate intake in carbohydrate-preferring rats (Gosnell et al., 1990). Such results have led to the conclusion that opioid effects on macronutrient selection and overall food intake are mediated through their actions in modulating food reward (Glass, Billington, & Levine, 2000).
Dopaminergic mediation of aspects of palatability has also been documented. Low doses of dopamine agonists increase food intake (Sills & Vaccarino, 1996), and animals with severe neurotoxin-induced dopamine depletions (Ungerstedt, 1971) or dopamine deficiency through gene knockout (Zhou & Palmiter, 1995) fail to consume food independently. Feeding increases extracellular dopamine within the nucleus accumbens, and the increase is greater with the consumption of a highly palatable food (Martel & Fantino, 1996), suggesting a specific role for mesolimbic dopamine in mediating food reward. A specific role for dopamine in signaling the incentive value of foods is also supported by work with dopamine antagonists. Dopamine antagonists potently reduce the sham intake of palatable diets. An ID50 dose of the dopamine 2 (D2) antagonist raclopride produces the same effect on both overall intake and the microstructure of licking as does halving the sucrose concentration (Schneider, Davis, Watson, & Smith, 1990). The consumption of 10% sucrose with raclopride resembles the consumption of 5% sucrose without antagonist pretreatment. Such data have been interpreted as suggesting that dopamine plays a critical role in the hedonic processing of orosensory stimuli. However, unlike opioids that can be shown to shift the hedonic response to ingestants in taste reactivity tests, dopamine antagonists suppress both hedonic and aversive responses (Pecina, Berridge, & Parker, 1997), suggesting alterations in intake through a change in sensorimotor responses rather than through a shift in taste palatability. Such data have been interpreted to suggest that dopaminergic antagonists reduce ingestion of palatable diets by affecting the incentive salience rather than by shifting the hedonic value of palatable diets.
The nutrient consequences of ingestion can also serve to reinforce dietary choice. This is best demonstrated in experiments that pair a novel taste with an intragastric nutrient infusion. Rats prefer the taste that has been associated with intragastric nutrient (Bolles, Hayward, & Crandall, 1981; Sclafani, 1991). Such nutrient conditioning has been demonstrated with simple and complex carbohydrates (Elizalde & Sclafani, 1990; Perez, Lucas, & Sclafani, 1998), proteins (Perez, Ackroff, & Sclafani, 1996), and fats (Lucas & Sclafani, 1989).Although the phenomena of flavor conditioning are well documented, the neural mediation is not well understood. There is some evidence that such preference conditioning can alter the taste responses to the paired flavor at the level of the nucleus of the solitary tract (Giza, Ackroff, McCaughey, Sclafani, & Scott, 1997). However, these effects are relatively weak. Potential opioid mediation of nutrient conditioning has also been investigated. The opioid antagonist naltrexone fails to block either the acquisition or the expression of a flavor preference conditioned by intragastric nutrients (Azzara, Bodnar, Delameter, & Sclafani, 2000), arguing for a nonopioid mediation of nutrient conditioning.
Satiety Signaling
In many species, including humans, food intake occurs in distinct bouts or meals. Meal initiation is determined by a variety of factors, especially food availability. During a meal, ingested nutrients contact a variety of receptors within the oral cavity and gastrointestinal tract, resulting in neural and hormonal signals that contribute to the determination of meal size. Meal size can be highly variable, and alterations in meal size appear to be a major determinant of overall food intake.
Taste plays an important role in determining meal size. Palatable or good-tasting substances are consumed more rapidly and in greater amounts than are unpalatable foods. Analyses of patterns of sham feeding not only have demonstrated effects of palatability on ingestion but also have revealed pregastric contributions to satiety. Sham feeding does eventually stop, and a number of processes have been proposed to contribute to the cessation of sham feeding, including oral metering (Mook, 1990), habituation (Swithers & Hall, 1994), and sensory-specific satiety (decreasing pleasantness of a specific food as more is ingested; B. J. Rolls, 1986). The amount that is sham fed depends also on the experience of the animal with the sham feeding paradigm. Although the rats’intakes double the first time that they sham feed, continued experience with sham feeding significantly increases intake over the next three or four tests. These data demonstrate the presence of a conditioned inhibition on food intake that is due to an association of the oral stimulation with postingestive negative feedback. Only with continued experience is this conditioned inhibition on intake overcome (Davis & Smith, 1990; Weingarten & Kulikovsky, 1989).
In normal ingestion, consumed nutrients contact mechanoand chemosensitive receptors that provide feedback information to the brain that is important to the control of meal size. The potential range of feedback mechanism that could be operating to lead to meal termination is dependent on the distribution of ingested nutrients during the meal. Kaplan, Spector, and Grill (1992) demonstrated in the rat that when the stomach is filled at rates mimicking normal ingestion rates, gastric emptying during the period of gastric fill is much more rapid than following fill, occurs at a constant rate for the duration of the fill period, and is not affected by nutrient concentration. Similar results were found whether the meal was infused or ingested by the rat (Kaplan, Seimers, & Grill, 1997). These data demonstrate that a significant portion of ingested nutrients (in the rat as much as 30%) enters the duodenum, contacts duodenal receptors, and is available for absorption. Similar dynamics of gastric emptying during fill have been demonstrated in rhesus monkeys; however, although volume is a main determinant, nutrient concentration also plays a significant role (Moran, Knipp, & Schwartz, 1999). Thus, the stomach and a significant proportion of the upper intestine are potential sites for within-meal generation of feedback signals.
The vagus nerve (Xth cranial nerve) is the major neuroanatomical link between the gastrointestinal tract and the brain. Vagal afferent fibers with cell bodies in the nodose ganglion arise from the digestive organs and project to the nucleus of the solitary tract (NTS) with a rough viscerotopic representation of the alimentary canal (Altschuler, Bao, Bieger, Hopkins, & Miselis, 1989). The response properties of vagal afferents depend in part on the target organ from which they arise. Although there are also significant spinal gut neural connections, the response properties of this system have not been well characterized.
Mechanosensitive gastric vagal afferents increase their firing in response to increasing gastric load volume. Slowly adapting mechanoreceptive fibers increase their response rate with increasing gastric volume (Andrews, Grundy, & Scratcherd, 1980). The fibers remain active while load volume is retained and show an off response in which activity briefly drops below baseline levels when the load volume is removed. Individual afferents are differentially tuned such that there are differences in their dynamic ranges (G. J. Schwartz, McHugh, & Moran, 1993). Some afferents reach their maximal activity at small intragastric volumes, whereas others do not begin to respond until a significant gastric load is present. Gastric mechanoreceptive vagal afferents do not respond directly to the chemical character of the gastric load. Response rate is similarly increased by nutrient and nonnutrient load volumes that are restricted to the stomach by a pyloric noose (Mathis, Moran, & Schwartz, 1998).
Duodenal vagal afferents are activated by both intraluminal load volume and nutrient character. Slowly adapting mechanoreceptive fibers in the duodenum have been identified. Similar to gastric mechanoreceptive fibers, activity increases with increases in load volume. Duodenal vagal afferents are also directly responsive to nutrient character. For example, both intestinal casein (Eastwood, Maubach, Kirkup, & Grundy, 1998) or lipid infusions (Randich et al., 2000) increase vagal afferent activity. Although gastric vagal activity is not directly responsive to intragastric nutrient character, gastric afferent responsivity can be altered by duodenal nutrient (G. J. Schwartz & Moran, 1998). Thus, gastric vagal afferent activity is modulated in the presence of duodenal nutrients.
These alterations in vagal afferent activity may reflect the actions of duodenal nutrient-induced release of gastrointestinal (GI) peptides. For example, the brain-gut peptide cholecystokinin (CCK) is released by the duodenal presence of nutrient digestion products. Local arterial CCK administration results in increases in vagal gastric mechanoreceptive afferent activity similar to those produced by intragastric load (G. J. Schwartz, McHugh, & Moran, 1991). Combinations of gastric load and CCK produce greater degrees of activity than either alone (G. J. Schwartz et al., 1991). CCK also modifies responses to subsequent intragastric load such that load volume results in greater degrees of activity following CCK administration than prior to it even at times when the initial response has disappeared (G. J. Schwartz et al., 1993). Duodenal vagal afferents also are activated by CCK; combinations of load and CCK combine to produce greater duodenal vagal afferent activity than either alone, and CCK affects the response to subsequent load volumes (G. J. Schwartz, Tougas, & Moran, 1995). CCK also plays a role in the response of duodenal afferents to nutrients. Administration of a CCK antagonist blocks the increase in vagal afferent activity produced by intraduodenal casein (Eastwood et al., 1998).
CCK-induced changes in gastric vagal afferent activity appear to result from a direct action of the peptide on the vagal afferent fibers. Vagal afferents contain CCK receptors (Moran, Norgren, Crosby, & McHugh, 1990), and CCK induces decreases in intragastric pressure that would not be expected to result in a secondary increase in vagal afferent activity (G. J. Schwartz, Moran, White, & Ladenheim, 1997). In contrast, gastrin-releasing peptide (GRP) induced increases in gastric vagal activity appear to be secondary to local peptide-induced changes in gastric motility. GRP increases gastric wall tension and intragastric pressure, and the increases in vagal afferent activity are correlated with these changes. In addition, GRP receptors are not found on vagal afferents (G. J. Schwartz et al., 1997).
Elimination of aspects of vagal afferent or peptideinduced feedback can result in significant alterations in the way that rats pattern their food intake. Surgical vagal deafferentation results in alterations in meal patterns in rats maintained on liquid diet in that such rats consume larger, less frequent meals than do sham-operated controls (G. J. Schwartz, Salorio, Skoglund, & Moran, 1999). Meal frequency is reduced in response to these increases in meal size such that overall food intake is unchanged. Similar alterations in meal size have been reported in response to capsaicin-induced chemical deafferentation. Following capsaicin treatment, rats consume larger meals on a novel diet (Chavez, Kelly, York, & Berthoud, 1997) or with calorically dilute sucrose access (Kelly, Morales, Smith, & Berthoud, 2000). These data demonstrate a role for vagal afferent feedback in the controls of meal size.
Peripheral Peptide Satiety Signaling
A number of peripherally acting peptides with roles in the controls of food intake have been identified. The best characterized of these is the brain-gut peptide CCK. Exogenously administered CCK was originally demonstrated to decrease food intake in rats (Gibbs, Young, & Smith, 1973). This feeding-inhibitory action of CCK and CCK agonists has been demonstrated in a variety of species including humans and nonhuman primates (Moran & McHugh, 1982; Pi-Sunyer et al., 1982). Exogenously administered CCK reduces meal size and results in an earlier appearance of a behavioral satiety sequence (Antin, Gibbs, Holt, Young, & Smith, 1975). A role for CCK in the control of the size of individual meals was confirmed by experiments examining the effects of repeated, meal-contingent CCK administration. CCK consistently reduced meal size without producing a significant change in overall daily food intake (West, Fey, & Woods, 1984).
The satiety actions of CCK depend on interactions with multiple receptor sites. CCK-A receptors, the receptor subtype through which the satiety actions of CCK are mediated, are found on vagal afferent fibers and on circular muscle cells within the pyloric sphincter. As discussed earlier, CCK activates vagal afferents. Surgical or chemical disruption of subdiaphragmatic vagal afferent innervation significantly affects the ability of CCK to inhibit food intake (Ritter & Ladenheim, 1985; Smith, Jerome, & Norgren, 1985; Moran, Baldessarini, Solorio, Lowerry, & Schwartz, 1997). The nature of this disruption is a reduction in CCK’s potency. Low doses of CCK that inhibit food intake in intact rats are ineffective following vagal afferent lesions. Higher doses inhibit intake but to a smaller degree. In contrast, surgical removal of the pyloric sphincter does not affect the ability of low doses of CCK to inhibit intake but truncates the dose-effect curve such that the additional suppression that normally accompanies higher CCK doses is eliminated (Moran, Shnayder, Hostetler, & McHugh, 1988). Results such as these have led to the proposal that the satiety actions of CCK are multifaceted and are, in part, secondary to its local gastrointestinal effects (Moran & McHugh, 1992).
A role for endogenous CCK in satiety is supported by data demonstrating that administration of CCK antagonists with specificity for the CCK-Areceptor results in increases in food intake (Moran, Ameglio, Peyton, Schwartz, & McHugh, 1993; Reidelberger & O’Rourke, 1989). In the primate, the effects have been demonstrated to be dose related with a maximum increase of around 40% in daily food intake in monkeys with 4-hr daily food access. This increase is almost completely accounted for by an increase in the size of their first meal (Moran et al., 1993). Alterations in meal patterns are also evident in rats lacking CCK-A receptors. Otsuka Long Evans Tokushima Fatty (OLETF) rats have been demonstrated to have approximately a 6-kb (kilobase) deletion in the CCK-A receptor gene spanning the promotor region and the first and second exons. This deletion prevents protein expression resulting in a CCK-A receptor knockout rat (Takiguchi et al., 1997). OLETF rats are obese and hyperphagic. Characterization of their spontaneous solid food intake has revealed a 35% increase in daily food intake resulting from a 78% increase in meal size combined with an insufficient decrease in meal frequency. Similar results are obtained when OLETF rats are maintained on liquid diet. Meal size, expressed as the number of licks, is increased by 93% (Moran, Katz, Plata-Salaman, & Schwartz, 1998).
Satiety actions have also been demonstrated for the mammalian bombesin-like peptides GRP and neuromedin-B (NMB). These peptides reduce food intake following peripheral exogenous administration (Gibbs, Fauser, Rowe, Rolls, & Maddison, 1979; Ladenheim, Taylor, Coy, & Moran, 1994; Stein & Woods, 1982). Bombesin is the most potent—an effect that can be best explained by its high affinity for both GRP and NMB receptors. Bombesin activates both mammalian pathways and produces an effect similar in magnitude to combined GRP and NMB administration (Ladenheim, Wirth, & Moran, 1996). Both vagal and spinal afferents contribute to the mediation of the satiety actions of abdominal bombesin-like peptides. Either combined vagotomy, dorsal rhizotomy, and cord section or neonatal capsaicin administration are necessary to abolish the effects of bombesin on food intake (Stuckey, Gibbs, & Smith, 1985; Michaud, Anisman, & Merali,1999). Bombesin-like peptides also inhibit food intake following central administration, and the site of action for this effect is within the caudal hindbrain (F. W. Flynn, 1989; Ladenheim & Ritter, 1988). There does appear to be a relationship between the central and peripheral actions of these peptides because central antagonist administration can block the effect of peripherally administered peptides (Ladenheim, Taylor, Coy, Moore, & Moran, 1996). Such results suggest the possibility that peripherally administered bombesin-like peptides may exert some of their actions through a central site.
Arole for endogenous mammalian bombesin-like peptides in satiety is supported by data demonstrating increases in food intake following antagonist administration. Central GRP (F. W. Flynn, 1992; Merali, Moody, & Coy, 1993) and NMB receptor antagonists (Ladenheim et al., 1997) have been demonstrated to increase food intake in a variety of feeding paradigms.These data provide further support for a central site of action as being important for the feeding effects of bombesin-like peptides and are consistent with a role for endogenous bombesin-like peptides in the controls of meal size.
Satiety actions for the pancreatic peptides glucagon and amylin have also been demonstrated. Rapidly eating elicits an increase in pancreatic glucagon secretion (Langhans, Pantel, Muller-Schell, Effengerger, & Scharrer, 1984). Because an increase in plasma glucagon is also stimulated by sham feeding, this appears to be a cephalic phase response (Nilsson & Uvnas-Wallenstien, 1977). Glucagon is rapidly cleared from the circulation by the liver (Langhans et al., 1984),which appears to be the site of glucagon’s satietyaction (Geary, 1998). Hepatic-portal infusion of glucagon at meal onset elicits a dose-related reduction in meal size (Geary & Smith, 1982a), and glucagon’s satiety actions have been demonstrated in human subjects (Geary, Kissileff, Pi-Sunyer, & Hinton, 1992). Glucagon’s satiety action requires the presence of other forms of ingestional consequences because glucagon does not affect sham feeding (Geary & Smith, 1982b).Arole for endogenous glucagon in the control of meal size is supported by data demonstrating the ability of hepatic portal infusions of glucagon antibody to increase meal size (LeSauter, Noh, & Geary, 1991).
Amylin inhibits feeding in a dose-dependent and behaviorally specific manner following either peripheral or central administration (Lutz, Geary, Szabady, Del Prete, & Scharrer, 1995; Lutz, Rossi, Althaus, Del Prete, & Scharrer, 1998). Although meal-related amylin release has not been specifically shown, amylin is obligatorily cosecreted with insulin by pancreatic beta cells (Cooper, 1994). Thus, amylin levels rise rapidly with meal onset and remain elevated for a significant period of time during and following meals. Amylin’s site of action is within the area postrema, a hindbrain structure lacking a blood-brain barrier. The area postrema contains amylin receptors, and lesions of the area postrema block the feedinginhibitory actions of peripherally administered amylin (Lutz, Senn, et al., 1998). A physiological role for endogenous amylin in feeding controls is supported by experiments demonstrating increases in food intake in response to administration of amylin antagonists (Rushing et al., 2001).
Unlike these peptides that play roles in limiting food intake, ghrelin, a brain-gut peptide that is primarily synthesized in the stomach, has recently been shown to stimulate food intake following peripheral or central administration (Tschop, Smiley, & Heiman, 2000; Wren et al., 2000). Ghrelin synthesis and plasma ghrelin levels are increased by food deprivation and reduced by refeeding (Tschop et al., 2000). Systemic and central ghrelin administration produce c-fos activation within the arcuate nucleus (Hewson & Dickson, 2000; Nakazato et al., 2001), and central ghrelin administration increases arcuate NPY expression (Shintani et al., 2001), suggesting a hypothalamic site of action. Aphysiological role for ghrelin in feeding initiation or maintenance is supported by data demonstrating that ghrelin antibodies suppress food intake (Nakazato et al., 2001). Together, these data suggest a novel action for a gastric peptide in stimulating food intake.
Interactions Among Control Systems
With food intake being influenced by these seemingly separate neural systems, the question of how they interact with one another is important. A number of the clearest demonstrations of interactions involve the adiposity signal leptin. As noted earlier, leptin circulates in direct relation to the degree of adiposity serving as a feedback signal for the overall regulation of energy balance. Both peripheral and central leptin administration reduce food intake, and a number of experiments have demonstrated that leptin’s effects on feeding are specific to reducing meal size without changing meal frequency (Eckel et al., 1998; M. C. Flynn, Scott, Pritchard, & Plata-Salaman, 1998; Kahler et al., 1998).
How does a signal that is critically involved in regulating hypothalamic pathways involved in energy balance result in reductions in the size of individual meals? Recent experiments have suggested multiple mechanisms through which leptin may affect food intake. Leptin’s actions may depend in part on its interactions with within-meal signals. For example, central administration of leptin at doses that are subthreshold for inhibiting feeding when administered alone enhance the satiating potential of peripheral CCK or an intragastric preload (Emond, Schwartz, Ladenheim, & Moran, 2001; Emond, Schwartz, & Moran, 1999). This action of leptin appears to depend on its ability to enhance the degree of NTS neural activation produced by these peripheral manipulations. That is, leptin enhances the dorsal hindbrain representation of ascending vagal afferent feedback signals arising from CCK or gastrointestinal stimulation induced by gastric preload.
Reducing leptin levels through food deprivation has the opposite result: The satiating potency of CCK is reduced (Billington, Levine, & Morley, 1983; McMinn, Sindelar, Havel, & Schwartz, 2000). This effect may be mediated through enhanced NPY signaling because NPY administration has the opposite effect to that of leptin on both the behavioral and neural activation potencies of CCK. NPY reduces the degree of NTS activation in response to CCK (McMinn et al., 2000).
Leptin also may result in reductions in meal size through its direct actions on taste sensitivity. Leptin specifically reduces chorda tympani and glossopharyngeal sensitivity to sweet stimuli without altering responses to other tastants (Kawai, Sugimoto, Nakashima, Mura, & Ninomiya, 2000). This appears to be a direct effect at the level of the taste bud because leptin hyperpolarizes the taste cell. Finally, leptin may decrease meal size by altering the reinforcing effects of ingestion. Leptin reduces the rewarding efficacy of electrical brain stimulation (Fulton, Woodside, & Shizgal, 2000). Thus, a signal derived from fat stores serving as a long-term regulator of energy balance has multiple actions. Many of these may contribute to its reductions in food intake in ways that enhance the negative feedback effects of ingestion while also reducing the positive feedback effects. Together these actions result in consistent reductions in meal sizes that over the long term serve to constrain energy intake and contribute to overall energy balance.
Satiety signals can also affect the efficacy of adiposity signals. For example, not only doesleptin enhance the potency of CCK within an individual meal situation, but also CCK enhances the leptin’s ability to reduce food intake and decrease body weight over the longer term (Matson, Reid, Cannon, & Ritter, 2000; Matson & Ritter, 1999). A dose of CCK that alone has no effect on 24-hr food intake or body weight significantly increases leptin’s effects on food intake and body weight. The site of action for this effect is yet to be determined,butitmaybehypothalamicbecauseinashort-termtest CCK significantly enhances the leptin-induced neural activation within the paraventricular nucleus (Emond, Schwartz, & Moran, 1998).
Other kinds of interactions have also been demonstrated. As ingestion continues, the perceived pleasantness or palatability of foods can change. That is, feedback signals arising from ingestion or ingestive consequences can alter aspects of taste processing. This may occur at multiple levels of the neural axis. For example, continued consumption of a single food results in that food’s being perceived as less pleasant in comparison to other nonconsumed foods. Such a phenomenon is referred to a sensory-specific satiety (B. J. Rolls, 1986). These changes are rapid and do not depend on the nutritional value of the consumed food, indicating that they likely arise from the sensory properties of the food, or on cognitive processes involved in assessing that enough of a particular type of food has been consumed. Sensory-specific satiety has been proposed to be an important mechanism for ensuring that a variety of foods are consumed, increasing the likelihood that an organism will maintain nutritional balance (B. J. Rolls, 1986). Sensory-specific satiety has a neurophysiological basis in that LH neurons that have ceased to respond to the taste of one food will respond to a different food (E. T. Rolls, Murzi, Yaxley, Thorpe, & Simpson, 1986).
Perceived pleasantness or palatability can also be reduced by gastrointestinal nutrient stimulation—a phenomena that has been termed alliesthesia (Cabanac, 1971). Thus, human subjects rate a sweet solution as less pleasant following a gastric glucose load (Cabanac & Fantino, 1977). Similar findings have been obtained in rats, using orofacial responses as a measure of the perceived pleasantness of taste stimuli (see Grill & Norgren, 1978). Gastric or intestinal nutrient infusions reduce the incidence of positive orofacial responses and increase the incidence of negative responses to an oral sucrose infusion (Cabanac & LaFrance, 1992). Similar results are produced by exogenous CCK, and the phenomenon is blocked by vagotomy (Cabanac & Zhao, 1994). Thus, one of the ways that within-meal negative feedback signaling affects ingestion is through a change in the perceived pleasantness of ingestive stimuli. In primates, the orbitofrontal cortex appears to be the likely neural site where such effects are mediated. Taste-evoked activity in the orbitofrontal cortex is suppressed by gastrointestinal nutrients (Scott, Yan, & Rolls, 1995).
A final example of interactions among signaling systems suggests a role for central reinforcing pathways in mediating the feeding actions of hypothalamic signaling systems. The opiate antagonist naloxone blocks the feeding stimulatory action of NPY (Kotz, Grace, Briggs, Levine, & Billington, 1995). The site of action for naloxone for this effect is within the medial subnucleus of the NTS (Kotz, Glass, Levine, & Billington, 2000). The site of action for the interaction appears to be within the amygdala. Naloxone does not affect NPY’s ability to induce c-fos within the hypothalamic paraventricular nucleus, but both NPY and naloxone induce c-fos within the central nucleus of the amygdala but do so in different cellular population (Pomonis, Levine, & Billington, 1997). Together, these data suggest that neural systems normally involved in palatability-induced feeding stimulation also play a modulatory role in the feeding induced by the hypothalamic signaling system’s response to adiposity stores.
Summary
The body contains multiple systems for regulating overall energy balance. These systems derive from and control different aspects of ingestive behavior and its consequences. Although adiposity, satiety, and reinforcement signaling have different primary sites of mediation within the brain, they are interacting systems that together ensure that the organism consumes an adequate amount and variety of nutrients. Although such interactions can now be demonstrated, little is known about the underlying cellular mechanisms through which they are mediated. Furthermore, how these interactions at the level of individual neurons are translated into behavioral outcomes remains to be determined. These are the two major issues currently facing investigators involved in research on the controls of food intake.
Over the past 10 years our knowledge of the brain sites and signaling systems involved in energy balance has grown exponentially. This has provided multiple targets for potential treatment development in obesity and eating disorders. A more complete understanding of how these systems respond under multiple metabolic states and interact with one another will be necessary to provide a rational base for such eventual treatment development.
Water Intake and Fluid Balance
The amount of water that we drink, like the amount of food that we eat, depends on a rich variety of factors that include homeostatic controls, learning and experience, and environmental social and cultural influences. Although there is ample evidence that the contribution of each of these factors is neurally mediated in the control of water intake, we concentrate here on the role of three relatively well-characterized systems that interact among themselves and that are important in the control of water balance. These three systems include, respectively, (a) neural and hormonal signals related to the detection of plasma osmolality and extracellular fluid volume that influence the initiation of bouts of ingestion, (b) neural and hormonal signals related to myriad factors that lead to satiety and thus terminate bouts of drinking, and (c) brain sites that receive and integrate these signals and that elicit appropriate physiological and behavioral responses. We also discuss the important interactions among these systems that permit overall regulation of body fluid balance.
Osmotic and Hypovolemic Signals That Stimulate Water Intake
All physiological processes occur in one or another internal sea consisting of mild salt solutions, and maintenance of the appropriate volume and concentration of the various fluid compartments in the body is essential for these processes to occur. Regulation occurs at the cellular level, enabling normal intracellular processes to occur, as well as at the level of the fluids that interconnect the cells, such that the formation and maintenance of extracellular fluid is a high priority. In this regard, maintenance of adequate blood volume is particularly essential for the delivery of nutrients to tissues and for the removal of metabolites for excretion. Thus, when body fluid balance is compromised, both physiological and behavioral responses are initiated to defend further aberrations in body fluid balance and to replenish lost body fluid stores. This could occur when fluid is shifted between compartments within the body (as in edema), when excess fluid is lost from the body (as occurs following hemorrhage or extreme vomiting), or when insufficient water and minerals are available for consumption. If water or sodium is lacking, the antidiuretic hormone arginine vasopressin (AVP) and the antinatriuretic hormone aldosterone work together to promote renal conservation of both water and sodium, thus preventing further body fluid depletion and maintaining the best possible level of osmolality. The behavioral responses of thirst and sodium appetite can also be engaged to restore lost water or salt because this is the only mechanism by which the lost fluids and electrolytes can be replaced. Both the physiological and the behavioral responses to perturbations of body fluid balance are under tight control by the brain. Although the careful balance of ingesting both water and salt is necessary for maintenance of extracellular fluid volume and concentration, this research paper focuses on the endocrine and neural controls of water intake.
Contemporary understanding of the physiology of water intake began with Andersson’s (1953; Andersson & Wyrwicka, 1957) report of the elicitation of drinking following the administration of hyperosmotic solutions to the brain of goats. Although the conscious goats had no apparent interest in water under basal conditions, they drank avidly when stimulated briefly within the anterior hypothalamus by small volumes of hypertonic saline. In later experiments drinking was elicited by weak electrical currents applied to the same anatomical sites. These reports demonstrated that water intake could be elicited by direct stimulation of the brain, and they thereby challenged the prevailing view that water intake was merely a sensation or a reflexive response to reduced salivary flow produced by dehydration (Cannon, 1918). In addition, these studies heralded the modern investigation of water intake by exploring its central neural basis and its instinctive (Lashley, 1938) and motivated (Stellar, 1954) origins. In the mid 1950s and early 1960s research focused on investigations of the water intake that accompanies cellular dehydration. This concept was initially proposed by Wettendorff (1901) and then established as a mechanism of
water intake by Gilman’s (1937) well-known experiments demonstrating that the administration of solutes that are excluded from cells (such as sodium) elicit cellular dehydration and are consequently highly effective dipsogens.
The more molar context of current research on the neural mechanisms of water intake was not achieved until Fitzsimons (1961) established hypovolemia (reduced blood volume) as an independent stimulus for thirst. He accomplished this by eliciting water intake in rats using several experimental manipulations that all resulted in reduced blood volume (e.g., hemorrhage, ligation of the inferior vena cava, hyperoncotic colloid dialysis). It is important that all of these paradigms resulted in reduced blood volume with no change of osmolarity of the remaining plasma, and hence with no change of cell volume. This essential point has been confirmed more clearly by the work of Tang (1976), who found (a) that these treatments reduce the plasma volume of rats without altering serum electrolytes or osmolarity and (b) that drinking is suppressed if the reduction in intravascular volume is prevented by intravenous infusion of an isotonic plasma substitute. Although earlier research had suggested that the causes of thirst are necessarily complex and that changes in extracellular volume, among others, must be considered (e.g., Adolph, Barker, & Hoy, 1954), the concept that hypovolemia is a second and potent cause of water intake— that hypovolemia operates under normal conditions of dehydration and has an independent sensory system utilizing detectors of reduced blood volume—was not considered. Rather, these concepts were elaborated by Fitzsimons (see Fitzsimons, 1979, for a full review) along with the subsequent proof of concept by Stricker (1968). Together, their work demonstrated that hypovolemia lowers the threshold for the initiation of drinking, that the water intake that is generated is a function of the magnitude of the reduction in blood volume, and that hypovolemia elicits drinking with the expected properties of motivation. In addition, the pioneering studies of hypovolemia-induced water intake also revealed the role of the renin angiotensin hormone system as an important systemic system that accesses the brain and stimulates water intake (Fitzsimons, 1969). Ultimately, the demonstration that cellular dehydration and extracellular volume loss can independently elicit water intake was suggested by the double depletion hypothesis of thirst (Epstein, Kissileff, & Stellar, 1973). Over a lengthy series of experiments, it was demonstrated that water intake in many naturalistic situations, and especially water deprivation, could be precisely predicted by this hypothesis. The bottom line is that cellular dehydration locally in the brain and systemic hypovolemia combine to produce the urge to drink, and the concurrent restoration of each deficit results in a summative suppression of drinking. The nature of the two depletions, the portions of the brain devoted to their regulation, and the manner of their joint function in the control of spontaneous drinking behavior directed much of the subsequent research on the physiology of water intake.
Cellular Dehydration and Brain Osmosensors
Cellular dehydration-induced water intake requires that the brain somehow detect water loss from osmosensitive or volume-sensitive cells and to generate a signal that leads to drinking. Studies in the early 1970s focused on cells within the brain that could be sensors that arouse drinking as a consequence of cellular water loss. Experiments by Peck and Novin (1971) and Blass and Epstein (1971) demonstrated that cells in the lateral preoptic area of the hypothalamus contained a large concentration of osmosensitive cells. When hyperosmotic solutions were applied locally in the vicinity of these cells, water intake was elicited. Conversely, when the cell group in the lateral preoptic area was selectively lesioned, the animals demonstrated impaired drinking stimulated by sudden increases in the osmolarity of the blood reaching the brain, whereas drinking elicited by hypovolemia remained intact.
Although more recent data have continued to support a role of the lateral preoptic area as a major osmosensitive area in the brain that elicits drinking, there remains considerable uncertainty about the location of the specific osmosensitive neurons that stimulate vasopressin secretion to promote water retention by the kidney. Candidate brain areas for these osmoreceptors are other subnuclei of the hypothalamus (including the lamina terminalis and the supraoptic nucleus) and the circumventricular organs (CVOs). The latter are implicated because they lack a blood-brain barrier and hence are sensitive to both plasma and brain interstitial osmotic influences. Further, they have axonal connections to areas that control drinking behavior.
Circumventricular Organs and Hypovolemic Water Intake
The demonstration that hypovolemia-induced intake is independent of cellular dehydration-induced intake arose from experiments in which rats drank water in response to an isotonic reduction of blood volume (Fitzsimons, 1961; Stricker, 1969; Tang, 1976). Because the osmolarity of the plasma is not increased as a function of reduced blood volume per se, the water intake cannot be attributed to dehydration of cells. The discovery of a hormonal control over this kind of drinking came from Fitzsimons’s (1964, 1969) demonstrations that the kidneys must be attached to the general circulation in order for hypovolemic treatments to have their full dipsogenic effects. This was demonstrated most clearly in following caval ligation, a procedure in which the inferior vena cava is occluded, preventing the return of the blood from the abdomen and lower limbs and thus reducing cardiac output by approximately 40%. The ensuing water intake that develops is dependent on access of the kidneys to the circulation. Because nephrectomy reduces caval ligation–induced intake, Fitzsimons reasoned not only that the kidney is necessary for eliciting hypovolemia-induced water intake but also that it does so as an endocrine rather than as an exocrine organ. The subsequent identification of renin, a peptide hormone produced by the kidney, and the demonstration that its levels are the rate-limiting step in the renin-angiotensin cascade that produces a powerful dipsogenic action, completed the story (Fitzsimons & Simons, 1969). It was subsequently found that renin acts as an enzyme that causes the formation of the peptide angiotensin II in the blood and that angiotensin II in turn gains access to the brain and stimulates drinking by acting on receptors in the CVOs.
The CVO that was initially observed to be particularly sensitive to the local application of angiotensin II in terms of eliciting a dipsogenic response was the subfornical organ (SFO; Simpson & Routtenberg, 1974). Using novel neuropharmacological application techniques, Simpson and his colleagues subsequently demonstrated that the SFO is exquisitely sensitive to the dipsogenic actions of angiotensin II as well as to other known dipsogenic agents such as the cholinomimetic carbachol. That group also found that lesions of the SFO rendered animals less responsive to hypovolemic stimuli as well as to intravenously administered angiotensin II, while still being responsive to cellular dehydration– induced stimuli (Simpson, Epstein, & Camardo, 1978). Subsequently, receptors that specifically bind angiotensin II have been localized in high concentrations in the SFO as well as in other brain areas. The distribution of angiotensin II receptors in the brain is of interest because many of the brain sites that contain high concentrations of these receptors receive direct projections from the SFO and are in other areas that lack a blood-brain barrier (Mendelsohn, Quirion, Saavedra, Aguiler, & Catt, 1984; Miselis, 1981).
The activation of these additional brain sites by angiotensin II is thought to occur by endogenous angiotensin II that is centrally generated because all of the components that are required to produce angiotensin II are present within the brain (Ganten, Hutchinson, Schelling, Ganten, & Fischer, 1975). Subsequent pharmacological studies have now revealed that there are at least two subtypes of angiotensin II receptors, designated angiotensin AT1 and AT2 receptors.
Although both receptor subtypes bind the native ligand angiotensin II with equal affinity, they differ in their amino acid sequences by over 70%. Based on this, the synthesis of nonpeptidergic ligands for each receptor subtype has become possible, and it is now recognized that the two receptors differ in binding affinity for these novel ligands and engage different second-messenger signaling systems once activated. Due in part to the widespread interest in these receptor subtypes in the control of various physiological functions, both AT1 and AT2 receptors have been cloned and sequenced. Subsequent research utilizing specific antisense oligodeoxynucleotide sequences has allowed both in vitro and in vivo receptor knockdown of each angiotensin receptor subtype. The bottom line from many experiments is that over 95% of the biological actions of angiotensin II appear to be mediated through its binding at the AT1 receptor. The physiological role of activation of the AT2 receptor subtype remains unclear. In sum, the SFO is a major site of action for peripherally generated angiotensin II in response to hypovolemia. The stimulation of the SFO, an area that contains high concentrations of angiotensin AT1 receptors, by systemic angiotensin II may also trigger the central angiotensin system to stimulate drinking as well as other physiological responses (such as the release of vasopressin) to maintain fluid homeostasis in response to hypovolemia.
Satiety Signals for Water Intake
The intake of water, like the intake of food, is under the control of diverse signals, some of which initiate the behavior and others of which stop it (i.e., satiety signals). Unlike the well-described satiety signals that terminate feeding, however, the satiety signals that terminate drinking are much less clear. A thirsty animal allowed the opportunity to drink water will rapidly consume sufficient water to restore the lost fluids. Although the animal may ingest a large quantity of fluid, satiation generally occurs several minutes prior to the time that substantial water is absorbed from the digestive system (Ramsay, Rolls, & Wood, 1977). Thus, the possibility that some sort of oral metering of ingested fluids provides a least one level of input to the satiation of thirst has been considered. Support for this concept derives from the data of Nicolaidis (1968), who demonstrated that infusions of water into the oral cavity of dehydrated rats produced rapid decreases in plasma vasopressin prior to any substantial absorption of the fluid by the digestive system. Although receptors in the mouth and throat can be demonstrated to influence the amount of water an animal ingests, receptors in the stomach, small intestine, and liver are also critically involved in the normal satiation of drinking. That is, preloads of water given by gastric gavage (thereby bypassing oral stimulation) also reduce drinking. Unlike the signals that lead to satiation of food intake, there is no clear evidence that receptors in the duodenum are involved in satiation of water intake.
The site of integration of the satiety signals for drinking is also unclear, although recent data have implicated the lateral parabrachial nucleus in the caudal brain stem as being important. This nucleus receives gustatory input from the tongue and appears to be an important site for the integration of signals that control fluid intake. Data from Menani and colleagues have demonstrated that this brain area may be producing a tonic serotonergic inhibitory tone on fluid intake (Menani, Colombari, Beltz, Thunhorst, & Johnson, 1998). During episodes of hypovolemia, parabrachial serotonergic tone is decreased, thus allowing the expression of drinking. Other neurotransmitters have also been found to inhibit fluid intake, including oxytocin, which is generated in forebrain areas and is projected to caudal brain sites to inhibit fluid ingestion. The identification of satiety signals for drinking awaits future research.
Interactions Among Other Control Systems
Besides being mediated by both osmotic and hypovolemic signals, the controls of water intake interact with other homeostatic control systems as well. Sodium homeostasis and its behavioral counterpart, sodium appetite, provide an important example of how the controls of water intake interact with other systems. Recall that for adequate reestablishment of extracellular fluid volume, electrolytes that act as osmotic agents are essential for maintaining water within the extracellular fluid compartment. There is ample evidence that the angiotensin II that is secreted in response to hypovolemic signals also stimulates a specific appetite for sodium as well as for water (Weisinger, Blair-West, Burns, Denton, & Tarjan, 1997). In addition, many of the same brain areas (SFO, other CVOs, several hypothalamic nuclei) at which the actions of angiotensin II regulate water intake also alter sodium appetite. For example, the expression of angiotensin II receptors can be differentially regulated by circulating levels of adrenal steroids such as aldosterone in sodiumdepleted rats, and sex steroids such as estrogen can modulate the dipsogenic potency of angiotensin II in the normally cycling female rat (Kisley, Sakai, & Fluharty, 1999).
Summary
In summary, we have reviewed the multiple mechanisms known to influence the elicitation and cessation of drinking. Because the maintenance of blood volume and osmotic pressure is so critical to the functioning of every organ system, and because even small deviations from the ideal can soon incapacitate an organism, the control system is exquisitely sensitive and fast to respond. In an ideal world, water and electrolytes would be consumed in the right volumes and concentrations to preclude having to monitor and adjust their levels constantly, and at one level of control this is what actually happens. Most individuals, when they are able, consume sufficient electrolytes and water with their food to ensure adequate regulation. In fact, estimates of the percentage of total daily water that is consumed when food is being eaten (i.e., at meal times) under conditions of ad libitum access range from 70% to 90% or more. Any excess water or electrolytes that are consumed during meals are rapidly and efficiently excreted from the body in the urine.
Unfortunately, few organisms live in such luxury and thus cannot rely on prandial consumption of sufficient water and electrolytes. As a result, they fall back on the control systems described in this research paper. In this process, the brain relies primarily on osmotic and volumetric signals arising in key sensory receptors in strategic locations in the body, as well as in the brain itself, to determine body fluid status. When deviations from the ideal are detected, the brain has a complex armamentarium of responses on which it can draw to reverse the problem and preclude its worsening. Hence, the brain can engage specific neurohormonal systems such as the reninangiotensin system to restore fluid balance.
As with food intake, there are signals that stimulate drinking, as well as signals that terminate drinking; the two interacting types of signals maximize the likelihood of consuming adequate amounts of water and electrolytes. The normal integration of these stimuli ensures that behavioral and physiological responses occur, in many cases, in anticipation of need states such that the individual is protected from large demands to defend homeostatic processes. That is, in a predictable environment, when an inadequate supply of water and electrolytes is inevitable, animals learn to activate the appropriate regulatory responses in anticipation of the situation and hence circumvent problems of fluid balance before they arise. These vital and complex regulatory processes are controlled, in many cases, utilizing redundant systems such that even in the case of disease or injury the individual is still able to function and respond normally.
One area in fluid balance that is not yet well understood is the nature of the controls involved in prandial drinking (drinking in association with meals). We do not know whether prandial drinking is elicited by the osmotic load of the meal or if the drinking occurs in anticipation of the osmotic load. We also do not yet appreciate whether the neurotransmitters and hormones that we normally associate with controlling water intake specific to fluid balance are involved in prandial drinking or whether this represents a unique situation. These issues remain to be investigated.
The investigation of water and sodium ingestion has provided insights into how the brain controls motivated behavior. A number of points are obvious. The first is that the controls over fluid balance in the body parallel in many ways those involved in energy regulation. Just as the body monitors key parameters such as blood glucose and body adiposity, it tracks osmolarity and blood volume. The second is that the central control over all homeostatically regulated systems, including fluid balance, is integrated such that water and electrolyte intake and excretion do not occur in a vacuum. Rather, the brain takes into account all of the key systems, compromises where necessary, and ensures the long-term survival of the organism. The study of water intake has also provided a model system to examine how peptide and steroid hormones interact with neural signals in the control of behavior. Specific brain areas that are critical in the control of these behaviors, as well as specific chemical signals that mediate this control (hormones and neurotransmitters), have been identified through the incorporation of modern biochemical and molecular biological tools. Because of the explosion of new techniques available in the last decade, great advances into how this complex behavior is governed have been forthcoming.As we look to the future, studies examining the interactions among the controls over caloric, thermal, and fluid needs, including the various neurochemical systems that mediate them, will be more clearly examined. Finally and most important, given the increasing knowledge of the controls of ingestive behavior, we hope to begin to use this information to develop rational and viable treatments for common human disorders such as obesity and hypertension.
Bibliography:
- Adolph, E. F., Barker, J. P., & Hoy, P. A. (1954). Multiple factors in thirst. American Journal of Physiology, 178, 538–562.
- Aja, S., Sahandy, S., Ladenheim, E. E., Schwartz, G. J., & Moran, T. H. (2001). Intracerebroventricular CART peptide reduces food intake and alters motor behavior at a hindbrain site. American Journal of Physiology, 281, R1862–R1867.
- Altschuler, S. M., Bao, X., Bieger, D., Hopkins, D. A., & Miselis, R. R. (1989). Viscerotopic representation of the upper gastrointestinal tract in the rat: Sensory ganglia and nuclei of the solitary and spinal trigeminal tracts. Journal of Comparative Neurology, 243, 248–268.
- Anand, B. K., & Brobesck, J. R. (1951). Localization of a feeding center in the hypothalamus of the rat. Proceedings of the Society for Experimental Biology and Medicine, 77, 323–324.
- Andersson, B. (1953). The effect of injections of hypertonic NaClsolutions in different parts of the hypothalamus of goats. Acta Physiologica Scandinavica, 28, 188–201.
- Andersson, B., & Wyrwicka, W. (1957). The elicitation of a drinking motor conditioned reaction by electrical stimulation of the hypothalamic “drinking area.” Acta Physiologica Scandinavica, 41, 194–198.
- Antin, J., Gibbs, J., Holt, J., Young, R. C., & Smith, G. P. (1975). Cholecystokinin elicits the complete behavioral satiety sequence in rats. Journal of Comparative and Physiological Psychology, 89, 784–790.
- Azzara, A. V., Bodnar, R. J., Delameter, A. R., & Sclafani, A. (2000). Naltrexone fails to block the acquisition or expression of a flavor preference conditioned by intragastric carbohydrate infusions. Pharmacology, Biochemistry, and Behavior, 67, 545– 557.
- Beck, B., Burlet, A., Nicolas, J. P., & Burlet, C. (1993). Galanin in the hypothalamus of fed and fasted lean and obese Zucker rats. Brain Research, 623, 124–130.
- Beck, B., & Richy, S. (1999). Hypothalamic hypocretin/orexin and neuropeptide Y: Divergent interaction with energy depletion and leptin. Biochemical Biophysical Research Communications, 258, 119–122.
- Benoit, S. C., Schwartz, M. W., Lachey, J. L., Hagan, M. M., Rushing, P. A., Blake, K. A., Yagaloff, K. A., Kurylko, G., Franco, L., Danhoo, W., & Seeley, R. J. (2000). Anovel selective melanocortin-4 receptor agonist reduces food intake in rats and mice without producing aversive consequences. Journal of Neuroscience, 20, 3442–3448.
- Bernard, C. (1859). Lecons sur les proprietes physiologiques et les alterations pathologiques de l’organisme. Paris: Baillers.
- Billington, C. J., Levine, A. S., & Morley, J. E. (1983). Are peptides truly satiety agents? A method for testing for neurohumoral satiety effects. American Journal of Physiology, 245, R920– R926.
- Bjorbaek, C., Elmquist, J. K., Michl, P., Ahima, R. S., van Buer, A., McCall, A. L., & Flier, J. S. (1998). Expression of leptin receptor isoforms in rat brain microvessels. Endocrinology, 139, 3485–3491.
- Bjorbaek, C., Uotoni, S., da Silva, B., & Flier, J. S. (1997). Divergent signaling capacities of the long and short isoforms of the leptin receptor. Journal of Biochemistry, 272, 32686–32695.
- Blass, E. M., & Epstein, A. N. (1971). A lateral preoptic osmosensitive zone for thirst in the rat. Journal of Comparative and Physiological Psychology, 76, 378–394.
- Bolles, R. C., Harward, L., & Crandall, C. (1981). Conditioned taste preferences based on caloric density. Journal of Experimental Psychology (Animal Behavior Processes), 7, 59–69.
- Breslin, P. A. S., Davis, J. D., & Rosenak, R. (1996). Saccharin increase the effectiveness of glucose in stimulating ingestion in rats but has little effect on negative feedback. Physiology and Behavior, 60, 411–416.
- Broberger, C., DeLecea, L., Sutcliffe, J. G., & Hokfelt, T. (1998). Hypocretin/orexin and melanin concentrating hormone expressing cells form distinct populations in the rodent lateral hypothalamus: Relationship to neuropeptide Y and agouti gene related protein systems. Journal of Comparative Neurology, 402, 460–474.
- Cabanac, M. (1971). Physiological role of pleasure. Science, 173, 1103–1107.
- Cabanac, M., & Fantino, M. (1977). Origin of olfacto-gustatory alliesthesia: Intestinal sensitivity to carbohydrate concentration? Physiology and Behavior, 18, 1039–1045.
- Cabanac, M., & LaFrance, L. (1992). Duodenal preabsorptive origin of gustatory alliesthesia in rats. American Journal of Physiology, 263, R1013–R1017.
- Cabanac, M., & Zhao, C. (1994). Postingestive alliesthesia produced by exogenous choloecystokinin and blocked by abdominal vagotomy. American Journal of Physiology, 266, R633–R637.
- Campfield, L.A., & Smith, F. J. (1986). Functional coupling between transient declines in blood glucose and feeding behavior; Temporal relationships. Brain Research Bulletin, 17, 427–433.
- Campfield, L. A., Smith, F. A., Guisez, Y., Devos, R., & Burn, P. (1996). Recombinant mouse ob protein: Evidence for a peripheral signal linking adiposity and central neural networks. Science, 271, 994–996.
- Cannon, W. B. (1918). The physiological basis of thirst. Proceedings of the Royal Society, London, 90B, 283–301.
- Cannon, W. B. (1932). The wisdom of the body. New York: Norton.
- Chavez, M., Kelly, L., York, D. A., & Berthoud, H. R. (1997). Chemical lesion of visceral afferents causes transient overconsumption of unfamiliar high-fat diets in rats. American Journal of Physiology, 272, R1657–R1673.
- Chornwall, B. M., Di Maggio, D. A., Massari, V. J., Pickel, S. M., Ruggiero, D. A., & O’Donohue, T. L. (1985). The anatomy of neuropeptide Y containing neurons in the rat brain. Neuroscience, 15, 1159–1181.
- Chua, S. C., Chung, W. K., Wu-Peng, X. S., Zhang, Y., Liu, S. M., Tartaglia, L., & Liebel, R. L. (1996). Phenotypes of mouse diabetes and rat fatty due to mutations in the OB (leptin) receptor. Science, 271, 994–996.
- Clark, J. T., Kalra, P. S., Crowley, W. R., & Kalra, S. P. (1984). Neuropeptide Y and human pancreatic polypeptide stimulate feeding behavior in rats. Endocrinology, 115, 427–429.
- Coleman, D. L. (1973). Effects of parabiosis of obese and diabetes and normal mice. Diabetologia, 9, 294–298.
- Cooper, G. J. (1994). Amylin compared with calcitonin gene-related peptide: Structure, biology and relevance to metabolic disease. Endocrine Review, 15, 163–201.
- Corp, E. S., Melville, L. D., Greenberg, D., Gibbs, J., & Smith, G. P. (1990). Effect of 4th ventricular neuropeptide Y and peptide YY on ingestive and other behaviors. American Journal of Physiology, 259, R317–R323.
- Corp, E. S., Woods, S. C., Porte, D., Jr., Dorsa, D. M., Figlewicz, D. P., & Baskin, D. G. (1986). Localization of 125I-insulin binding sites in the rat hypothalamus by quantitative autoradiography. Neuroscience Letters, 70, 17–22.
- Crawley, J. N. (1999). The role of galanin in feeding behavior. Neuropeptides, 33, 369–375.
- Crawley, J. N., Austin, M. C., Fiske, S. M., Martin, B., Consolo, S., Berthold, M., Langel, U., Fisone, G., & Bartfai, T. (1990). Activity of centrally administered galanin fragments on stimulation of feeding behavior and on galanin receptor binding in the rat hypothalamus. Journal of Neuroscience, 10, 3695–3700.
- Davis, J. D., & Levine, M. (1977). A model for the control of ingestion. Psychological Review, 84, 379–412.
- Davis, J. D., & Smith, G. P. (1990). Learning to sham feed: Behavioral adjustments to loss of physiological postingestive stimuli. American Journal of Physiology, 259, R1228–R1235.
- Doyle, T. G., Berridge, K. C., & Gosnell, B. A. (1993). Morphine enhances hedonic taste palatability in rats. Pharmacology, Biochemistry, and Behavior, 46, 745–749.
- Eastwood, C., Maubach, K., Kirkup, A. J., & Grundy, D. (1998). The role of endogenous cholecystokinin in the sensory transduction of luminal nutrient signaling in the rat jejunum. Neuroscience Letters, 254, 145–153.
- Eckel, L. A., Langhans, W., Kahler, A., Campfield, L. A., Smith, F. J., & Geary, N. (1998). Chronic administration of OB protein decreases food intake by selectively meal size in female rats. American Journal of Physiology, 275, R186–R189.
- Elizalde, G., & Sclafani, A. (1990). Flavor preferences conditioned by intragastric polycose; A detailed analysis using an electronic esophagus preparation. Physiology and Behavior, 47, 63–67.
- Elmquist, J. K., Bjorbaek, C., Ahima, R. S., Flier, J. S., & Saper, C. B. (1998). Distribution of leptin receptor mRNA isoforms in the rat brain. Journal of Comparative Anatomy, 395, 535–547.
- Epstein, A. N., Kissileff, H. R., & Stellar, E. (Eds.). (1973). The neuropsychology of thirst. Washington, DC: V. H. Winston & Sons.
- Erikson, J. C., Clegg, K. E., & Palmiter, R. D. (1996). Sensitivity to leptin and susceptibility to seizures in mice lacking neuropeptude Y. Nature, 381, 415–418.
- Fan, W., Boston, B. A., Kesterson, R. A., Hruby, V. J., & Cone, R. D. (1997). Role of melanocortinergic neurons in feeding and agouti obesity syndrome. Nature, 385, 165–168.
- Fitzsimons, J. T. (1961). Drinking by rats depleted of body fluid without increase in osmotic pressure. Journal of Physiology (London), 159, 297–309.
- Fitzsimons, J. T. (1964). Drinking caused by constriction of the inferior vena cava in the rat. Nature, 204, 479–480.
- Fitzsimons, J. T. (1969). The role of renal thirst factor in drinking induced by extracellular stimuli. Journal of Physiology (London), 201, 349–369.
- Fitzsimons, J. T. (1979). The physiology of thirst and sodium appetite. Cambridge, UK: Cambridge University Press.
- Fitzsimons, J. T., & Simons, B. J. (1969). The effect on drinking in the rat of intravenous infusion of angiotensin, given alone or in combination with other stimuli of thirst. Journal of Physiology (London), 203, 45–57.
- Flynn, F. W. (1989). Fourth ventricle bombesin injection suppresses ingestive behavior in rats. American Journal of Physiology, 256, R590–R596.
- Flynn, F. W. (1992). Fourth ventricular injection of selective bombesin receptor antagonists facilitates feeding in rats. American Journal of Physiology, 264, R218–R221.
- Flynn, M. C., Scott, T. R., Pritchard, T. C., & Plata-Salaman, C. R. (1998). Mode of action of OB protein (leptin) on feeding. American Journal of Physiology, 275, R174–R179.
- Fulton, S., Woodside, B., & Shizgal, P. (2000). Modulation of brain reward circuitry by leptin. Science, 287, 125–128.
- Ganten, D., Hutchinson, J. S., Schelling, P., Ganten, U., & Fischer, H. (1975). The isorenin angiotensin systems in extrarenal tissue. Clinical Experimental Pharmacology and Physiology, 2, 127–151.
- Geary, N. (1998). Glucagon and the control of meal size. In G. P. Smith (Ed.), Satiation: From gut to brain (pp. 164–197). New York: Oxford University Press.
- Geary, N., Kissileff, H. R., Pi-Sunyer, F. X., & Hinton, V. (1992). Individual, but not simultaneous, glucagon and cholecystokinin infusion inhibit feeding in men. American Journal of Physiology, 262, R975–R980.
- Geary, N., & Smith, G. P. (1982a). Pancreatic glucagon and postprandial satiety in the rat. Physiology and Behavior, 28, 313– 322.
- Geary, N., & Smith, G. P. (1982b). Pancreatic glucagon fails to inhibit sham feeding in the rat. Peptides, 3, 163–166.
- Gibbs, J., Fauser, D. J., Rowe, E. A., Rolls, E. T., & Maddison, S. P. (1979). Bombesin suppresses feeding in rats. Nature, 245, 323– 325.
- Gibbs, J., Young, R. C., & Smith, G. P. (1973). Cholecystokinin decreases food intake in rats. Journal of Comparative and Physiological Psychology, 84, 488–495.
- Gilman, A. (1937). The relation between blood osmotic pressure, fluid distribution and voluntary water intake. American Journal of Physiology, 120, 323–328.
- Giza, A. K., Ackroff, K., McCaughey, S. A., Sclafani, A., & Scott, T. R. (1997). Preference conditioning alters taste responses in the nucleus of the solitary tract. American Journal of Physiology, 273, R1230–R1240.
- Glass, M. J., Billington, C. J., & Levine, A. S. (2000). Opioids, food reward and macronutrient selection. In H.-R. Berthoud & R. J. Seeley (Eds.), Neural and metabolic control of macronutrient intake (pp. 407–423). Boca Raton, FL: CRC Press.
- Glass, M. J., Grace, M., Cleary, J. P., Billington, C. J., & Levine, A. S. (1996). Potency of naloxone’s anorectic effect in rats in dependent on diet preference. American Journal of Physiology, 271, R217–R221.
- Gosnell, B. A., Krahn, D. D., & Majchrzak, M. J. (1990). The effects of morphine on diet selection are dependent on baseline diet preferences. Pharmacology, Biochemistry, and Behavior, 37, 207–212.
- Grill, H. J., Ginsburg, A. B., Seeley, R. J., & Kaplan, J. M. (1998). Brainstem application of melanocortin receptor ligands produces long-lasting effects on feeding and body weight. Journal of Neuroscience, 18, 10128–10135.
- Grill, H. J., & Kaplan, J. M. (1992). Sham feeding in intact and chronic decerebrate rats. American Journal of Physiology, 262, R1070–R1074.
- Grill, H. J., Markison, S., Ginsberg, A., & Kaplan, J. M. (2000). Long term effects on feeding and body weight after stimulation of forebrain or hindbrain CRH receptors with urocortin. Brain Research, 867, 19–28.
- Grill, H. J., & Norgren, (1978). The taste reactivity test: I. Mimetic responses to gustatory stimuli in neurologically normal rats. Brain Research, 143, 263–279.
- Hagan, M. M., Rushing, P. A., Schwartz, M. W., Yagaloff, K. A., Burn, P., Woods, S. C., & Seeley, R. J. (1999). Role of CNS melanocortin system in the response to overfeeding. Journal of Neuroscience, 19, 2362–2367.
- Hahn, T., Breininger, J., Baskin, D., & Schwartz, M. (1998). Coexpression of AgRP and NPY in fasting activated hypothalamic neurons. Nature Neuroscience, 1, 271–272.
- Haynes, A. C., Jackson, B., Chapman, H., Tadyyon, M., Johns, A., Porter, R. A., & Arch, J. R. (2000). A selective orexin-1 receptor antagonist reduces food consumption in male and female rats. Regulatory Peptides, 96, 45–51.
- Heatherington, A. W., & Ranson, S. W. (1940). Hypothalamic lesions and adiposity in the rat. Anatomical Record, 78, 149–172.
- Hewson, A. K., & Dickson, S. L. (2000). Systemic administration of ghrelin induces Fos and Egr-1 proteins in the hypothalamus arcuate nucleus of fasted and fed rats. Journal of Endocrinology, 12, 1047–1049.
- Huszar, D., Lynch, C. A., Fairchild-Huntress, V., Dunmore, J. H., Fang, Q., Berlemeier, L. R., Gu, W., Kesterson, R. A., Boston, B. A., Cone, R. D., Smith, F. J., Campfield, L. A., Burn, P., & Lee, F. (1997). Targeted disruption of the melanocortin-4 receptor results in obesity. Cell, 88, 131–141.
- Ji, H., Graczyk-Milbrandt, G., & Friedman, M. I. (2000). Metabolic inhibitors synergistically decrease hepatic energy status and increase food intake. American Journal of Physiology, 278, R1579–R1582.
- Kahler, A., Geary, N., Eckel, L. A., Campfield, L. A., Smith, F. J., & Langhans, W. (1998). Chronic administration of OB protein decreases food intake by selectively meal size in male rats. American Journal of Physiology, 275, R180–R185.
- Kalra, S. P., Dube, M. G., Sahu,A., Phelps, C. P., & Kalra, P. (1991). Neuropeptide Y secretion increases in the paraventricular nucleus in association with increased appetite for food. Proceedings of the National Academy of Sciences, 88, 10931–10935.
- Kaplan, J. M., Siemers, W. H., & Grill, H. J. (1997). Effect of oral versus gastric delivery on gastric emptying of corn oil emulsions. American Journal of Physiology, 273, R1263–R1270.
- Kaplan, J. M., Spector, A. C., & Grill, H. J. (1992). Dynamics of liquid gastric emptying during and after stomach fill. American Journal of Physiology, 263, R813–R819.
- Kawai, K., Sugimoto, K., Nakashima, K., Mura, H., & Ninomiya, Y. (2000). Leptin as a modulator of sweet taste sensitivities in mice. Proceedings of the National Academy of Sciences, 97, 11044–11049.
- Kelly, L., Morales, S., Smith, B. K., & Berthoud, H. R. (2000). Capsaicin-treated rats permanently overingest low but not high concentration sucrose solutions. American Journal of Physiology, 279, R1805–R1812.
- Kennedy, G. C. (1953). The role of depot fat in the hypothalamic control of food intake in the rat. Proceedings of the Royal Society, London, 140, 579–592.
- Kim, E. M., Welch, C. C., Grace, M. K., Billington, C. J., & Levine, A. S. (1996). Chronic food restriction and acute food deprivation decrease mRNA levels of opioid peptides in the arcuate nucleus. American Journal of Physiology, 270, R1019–R1024.
- Kisley, L. R., Sakai, R. R., Fluharty, S. J. (1999). Estrogen decreases hypothalamic angiotensin II AT1 receptor binding and mRNA in the female rat. Brain Research, 844(1-2), 34–42.
- Kotz, C. M., Glass, M. J., Levine, A. S., & Billington, C. J. (2000). Regional effect of naltrexone in the nucleus of the solitary tract in blockade of NPY-induced feeding. American Journal of Physiology, 278, R499–R503.
- Kotz, C. M., Grace, M. K., Briggs, J. E., Levine, A. S., & Billington, C. J. (1995). Effects of opiate antagonists naloxone and naltrexone on neuropeptide Y induced feeding and brown fat thermoregulation in the rat: Neural site of action. Journal of Clinical Investigation, 96, 163–170.
- Kristensen, P., Judge, M. E., Thim, L., Ribel, U., Christjansan, K. N., Wulff, B. S., Clausen, J. T., Jensen, P. B., Madsen, O. D., Vrang, N., Larsen, P. J., & Hastrup, S. (1998). Hypothalamic CART is a new anorectic peptide regulated by leptin. Nature, 393, 72–76.
- Ladenheim, E. E., & Ritter, R. C. (1988). Low-dose 4th ventricular bombesin selectively suppresses food intake. American Journal of Physiology, 255, R988–R992.
- Ladenheim, E. E., Taylor, J. E., Coy, D. H., Carrigan, T. S., Wohn, A., & Moran, T. H. (1997). Caudal hindbrain neuromedin Bpreferring receptors participate in the control of food intake. American Journal of Physiology, 272, R433–R437.
- Ladenheim, E. E., Taylor, J. E., Coy, D. H., Moore, K. A., & Moran, T. H. (1996). Hindbrain GRP receptor blockade antagonizes feeding suppression by peripherally administered GRP. American Journal of Physiology, 271, R180–R184.
- Ladenheim, E. E., Taylor, J. E., Coy, D. H., & Moran, T. H. (1994). Blockade of feeding inhibition by neuromedin B using a selective receptor antagonist. European Journal of Pharmacology, 271, R7–R9.
- Ladenheim, E. E., Wirth, K., & Moran, T. H. (1996). Receptor subtype mediation of the feeding suppression by bombesin-like peptides. Pharmacology, Biochemistry, and Behavior, 54, 705–711.
- Langhans, W., Pantel, K., Muller-Schell, W., Effengerger, E., & Scharrer, E. (1984). Hepatic handling of pancreatic glucagon and glucose during meals in rats. American Journal of Physiology, 247, R827–R832.
- Lashley, K. S. (1938). The experimental analysis of instinctive behavior. Psychological Review, 45, 445–471.
- LeSauter, J., Noh, U., & Geary, N. (1991). Hepatic portal infusion of glucagon antibodies increases spontaneous meal size in rats. American Journal of Physiology, 261, R154–R161.
- Lewis, D. E., Shellard, L., Koeslag, D. C., Boer, D. E., McCarthy, H. D., McKibbin, P. E., Russell, J. C., & Williams, G. (1993). Intense exercise and food deprivation cause similar hypothalamic neuropeptide Y increases in rats. American Journal of Physiology, 264, E279–E284.
- Lopez, M., Seoane, L., del Carmen Garcia, M., Lago, F., Casanueva, F. F., Senaris, R., & Dieguez, C. (2000). Leptin regulation of prepro-orexin and orexin receptor mRNA levels in the hypothalamus. Biochemical and Biophysical Research Communications, 269, 41–45.
- Lucas, F., & Sclafani, A. (1989). Flavor preferences conditioned by intragastric fat infusions in the rat. Physiology and Behavior, 46, 403–412.
- Lutz, T. A., Geary, N., Szabady, M. M., Del Prete, E., & Scharrer, E. (1995). Amylin deceases meal size in rats. Physiology and Behavior, 58, 1197–1202.
- Lutz, T. A., Rossi, R., Althaus, J., Del Prete, E., & Sharrer, E. (1998). Amylin reduces food intake more potently than calcitonin gene-related peptide (CGRP) when injected into the lateral brain ventricle in rats. Peptides, 19, 1533–1540.
- Lutz, T. A., Senn, M., Althaus, J., Del Prete, E., Ehrensperger, E., & Scharrer, E. (1998). Lesion of the area postema/nucleus of the solitary tract (AP/NTS) attenuates the anorectic effects of amylin and calcitonin gene related peptide (CGRP) in rats. Peptides, 19, 309–317.
- Maffei, M., Halaas, E., Ravussin, E., Pratley, R. E., Lee, G. H., Zhang, Y., Fei, H., Kim, S., Lallone, R., Ranganathan, S., Kern, P.A., & Friedman, J. M. (1995). Leptin levels in human and rodent: Measurement of plasma leptin and ob RNA in obese and weight reduced subjects. Nature Medicine, 1, 1155–1161.
- Marks-Kaufman, R., & Kanarek, R. B. (1990). Diet selection following chronic morphine and naloxone regimen. Pharmacology, Biochemistry, and Behavior, 35, 665–669.
- Marsh, D. J., Hollopeter, G., Kafer, K. E., & Palmiter, R. D. (1998). Role of Y5 neuropeptide Y receptor in feeding and obesity. Nature Medicine, 4, 718–721.
- Martel, P., & Fantinio, M. (1996). Mesolimbic dopaminergic system activity as a function of food reward: A microdialysis study. Pharmacology, Biochemistry, and Behavior, 53, 221–226.
- Mathis, C., Moran, T. H., & Schwartz, G. J. (1998). Load sensitive rat gastric vagal afferents encode volume but not gastric nutrients. American Journal of Physiology, 274, R280–R286.
- Matson, C. A., Reid, D. F., Cannon, T. A., & Ritter, R. C. (2000). Cholecystokinin and leptin act synergistically to reduce body weight. American Journal of Physiology, 278, R882–R890.
- Matson, C. A., & Ritter, R. C. (1999). Long term CCK-leptin synergy suggests a role for CCK in the regulation of body weight. American Journal of Physiology, 276, R1038–R1045.
- Mayer, J. (1953). Glucostatic mechanisms of regulation of food intake. New England Journal of Medicine, 249, 13–16.
- McMinn, J. E., Sindelar, D. K., Havel, P. J., & Schwartz, M. W. (2000). Leptin deficiency induced by fasting impairs the satiety response to cholecystokinin. Endocrinology, 141, 4442–4448.
- Melanson, K. J., Westerterp-Plantenga, M. S., Saris, W. H., Smith, F. J., & Campfield, L. A. (1999). Blood glucose patterns and appetite in time blinded humans: Carbohydrate vs fat. American Journal of Physiology, 277, R337–R345.
- Menani, J. V., Colombari, D. S. A., Beltz, T. G., Thunhorst, R. L., & Johnson, A. K. (1998). Salt appetite: Interaction of forebrain angiotensinergic and hindbrain serotonergic mechanisms. Brain Research, 801(1-2), 29–35.
- Mendelsohn, F. A. O., Quirion, R., Saavedra, J. M., Aguiler, G., & Catt, K. J. (1984). Autoradiographic localization of angiotensin II receptors in rat brain. Proceeding of the National Academy of Sciences, USA, 81, 1575–1579.
- Merali, Z., Moody, T. W., & Coy, D. (1993). Blockade of brain bombesin/GRP receptors increases food intake in sated rats. American Journal of Physiology, 264, R1031–R1034.
- Mercer, J. G., Lawrence, C. B., & Atkinson, T. (1996). Regulation of galanin gene expression in the hypothalamic paraventricular nucleus of the obese Zucker rat by manipulation of dietary macronutrient. Molecular Brain Research, 43, 202–208.
- Michaud, D., Anisman, H., & Merali, Z. (1999). Capsaicin sensitive fibers are required for the anorexic action of systemic but not central bombesin. American Journal of Physiology, 276, R1617– R1622.
- Miselis, R. R. (1981). The efferent projections of the subfornical organ of the rat: A circumventricular organ within a neural network subserving water balance. Brain Research, 230, 1–23.
- Mook, D. G. (1963). Oral and postingestional determinants of the intake of various solutions in rats with esophagela fistulas. Journal of Comparative and Physiological Psychology, 56, 645– 659.
- Mook, D. G. (1990). Satiety, specifications and stop rules: Feeding as a voluntary act. In A. N. Epstein & A. R. Morrison (Eds.), Progress in psychobiology and physiological psychology: Vol. 14. (pp. 1–65). New York: Academic Press.
- Moran, T. H., Ameglio, P. J., Peyton, H. J., Schwartz, G. J., & McHugh, P. R. (1993). Blockade of type A, but not type B, CCK receptors postpones satiety in rhesus monkeys. American Journal of Physiology, 265, R620–R624.
- Moran, T. H., Baldessarini, A. R., Solorio, C. F., Lowerry, T., & Schwartz, G. J. (1997). Vagal afferent and efferent contributions to the inhibition of food intake by cholecystokinin. American Journal of Physiology, 272, R1245–R1251.
- Moran, T. H., Katz, L. F., Plata-Salaman, C. R., & Schwartz, G. J. (1998). Disordered food intake and obesity in rats lacking CCKA receptors. American Journal of Physiology, 274, R618–R625.
- Moran, T. H., Knipp, S., & Schwartz, G. J. (1999). Gastric and duodenal features of meals mediate controls of liquid gastric emptying during fill in rhesus monkeys. American Journal of Physiology, 277, R1282–R1290.
- Moran, T. H., & McHugh, P. R. (1982). Cholecystokinin decreases food intake by inhibiting gastric emptying. American Journal of Physiology, 242, R491–R497.
- Moran, T. H., & McHugh, P. R. (1992). Gastric mechanisms in CCK satiety. In C. T. Dourish, S. J. Cooper, S. D. Iversen, & L. L. Iversen (Eds.), Multiple cholecystokinin receptors in the CNS (pp. 183–205). Oxford: Oxford University Press.
- Moran, T. H., Norgren, R., Crosby, R. J., & McHugh, P. R. (1990). Central and peripheral vagal transport of CCK binding sites occurs in afferent fibers. Brain Research, 526, 95–102.
- Moran, T. H., Shnayder, L., Hostetler, A. M., & McHugh, P. R. (1988). Pylorectomy reduces the satiety actions of cholecystokinin. American Journal of Physiology, 255, R1059– R1063.
- Morley, J. E., Levine, A. S., Gosnell, B. A., Kneip, J., & Grace, M. (1987). Effect of neuropeptide Y on ingestive behaviors in the rat. American Journal of Physiology, 252, R599–R609.
- Nakazato, M., Murakami, N., Date, Y., Kojima, M., Matuso, H., Kanagawa, K., & Matsukara, S. (2001). A role for ghrelin in the central regulation of feeding. Nature, 409, 194–198.
- Nilsson, G., & Uvnas-Wallenstein, K. (1977). Effect of teasing and sham feeding on plasma glucagon concentration in dogs. Acta Physiologica Scandinavia, 100, 298–302.
- Pavlov, I. P. (1910). The work of the digestive glands (2nd ed.). London: Charles Griffin.
- Pecina, S., Berridge, K. C., & Parker, L. A. (1997). Pimozide does not shift palatability: Separation of anhedonia from sensorimotor suppression of taste reactivity. Pharmacology, Biochemistry, and Behavior, 58, 801–811.
- Peck, J. W., & Novin, D. (1971). Evidence that osmoreceptors mediating drinking in rabbits are in the lateral preoptic area. Journal of Comparative and Physiological Psychology, 74, 134–147.
- Pedrazzini, T., Seydoux, J., Kunster, P., Aubert, J.-F., Grouzmann, E., Beerman, F., & Brunner, H.-R. (1998). Cardiovascular response, feeding behavior and locomotor activity in mice lacking the NPY Y1 receptor. Nature Medicine, 4, 722–726.
- Perez, C., Ackroff, K., & Sclafani, A. (1996). Carbohydrate and protein conditioned flavor preferences: Effects of nutrient preloads. Physiology and Behavior, 59, 467–474.
- Perez, C., Lucas, F., & Sclafani, A. (1998). Increased flavor acceptance and preference conditioned by the postingestive actions of glucose. Physiology and Behavior, 64, 483–492.
- Peyron, C., Tighe, D. K., van den Pol, A. N., de Leces, L., Heller, H. C., Sutcliffe, J. G., & Kilduff, T. S. (1998). Neurons containing hypocretin (orexin) project to multiple neural systems. Journal of Neuroscience, 18, 9996–10015.
- Pomonis, J. D., Levine, A. S., & Billington, C. J. (1997). Interaction of hypothalamic paraventricular nucleus and central nucleus of the amygdala in naloxone blockade of neuropeptide Y induced feeding revealed by c-fos expression. Journal of Neuroscience, 17, 5175–5182.
- Qu, D., Ludwig, D. S., Gammeltolft, S., Piper, M., Pellymounter, M. A., Cullen, M. J., Mathes, W. F., Przypek, J., Kanarek, R., & Maratos-Flier, E. (1996). A role for melanin concentrating hormone in the central regulation of feeding behavior. Nature, 380, 243–247.
- Ramsay, D. J., Rolls, B. J., & Wood, R, J. (1977). Thirst following water deprivation in dogs. American Journal of Physiology, 232, R93–R100.
- Randich, A., Tyler, W. J., Cox, J. E., Meller, S. T., Kelm, G. R., & Bharaj, S. S. (2000). Responses of celiac and cervical vagal afferents to infusions of lipids in the jejunum or ileum of the rat. American Journal of Physiology, 278, R34–R43.
- Reidelberger, R. D., & O’Rourke, M. F. (1989). Potent cholecystokinin antagonist L-364,718 stimulates food intake in rats. American Journal of Physiology, 257, R1512–R1518.
- Richter, C. P. (1943). Total self regulatory functions in animals and human beings. Harvey Lectures, 38, 63–103.
- Ritter, R. C., & Ladenhiem, E. E. (1985). Capsaicin pretreatment attenuates suppression of food intake by cholecystokinin. American Journal of Physiology, 248, R501–R504.
- Ritter, S., Dinh, T. T., & Zhang, Y. (2000). Localization of hindbrain glucoreceptors sites controlling food intake and blood glucose. Brain Research, 856, 37–47.
- Rolls, B. J. (1986). Sensory-specific satiety. Nutrition Reviews, 44, 93–101.
- Rolls, E. T., Murzi, E., Yaxley, S., Thorpe, S. J., & Simpson, S. J. (1986). Sensory specific satiety: Food specific reduction in responsiveness of ventral forebrain neurons after feeding in the monkey. Brain Research, 368, 79–86.
- Rossi, M., Choi, S. J., O’Shea, D., Miyoshi, T., Ghatei, M. A., & Bloom, S. R. (1997). Melanin-concentrating hormone acutely stimulates feeding, but chronic administration has no effect on body weight. Endocrinology, 138, 351–355.
- Rushing, P. A., Haga, M. M., Seeley, R. J., Lutz, T. A., D’Alessio, D. A., Air, E. L., & Woods, S. C. (2001). Inhibition of central amylin signaling increases food intake and body adiposity in rats. Endocrinology, 142, 5035–5038.
- Sahu, A. (1999). Evidence suggesting that galanin, melanin concentrating hormone, neurotensin, proopiomelanocortin and neuropeptide Y are targets of leptin signaling in the hypothalamus. Endocrinology, 139, 795–798.
- Sakurai, T., Amemiya, A., Ishii, M., Matszaki, I., Chemelli, R. M., Tanaka, H., Williams, S. C., Richardson, J. A., Kozlowski, G.P.,Wilson,S.,Arch,J.R.S.,Buckingham,R.E.,Haynes,A.C., Carr, S.A.,Annan, R. S., McNulty, D. E., Liu, W.-S., Terett, J.A., Elshourbagy, N. A., Bergsma, D. J., & Yanagisawa, M. (1998). Orexins and orexin receptors: A family of hypothalamic neuropeptides and G protein coupled receptors that regulate feeding behavior. Cell, 92, 573–585.
- Schneider, L. H., Davis, J. D., Watson, C. W., & Smith, G. P. (1990). Similar effects of raclopride and reduced sucrose concentration on the microstructure of sucrose sham feeding. European Journal of Pharmacology, 186, 61–70.
- Schwartz, G. J., McHugh, P. R., & Moran, T. H. (1991). Integration of vagal afferent responses to gastric load and CCK in rats. American Journal of Physiology, 261, R64–R69.
- Schwartz, G. J., McHugh, P. R., & Moran, T. H. (1993). Gastric loads and CCK synergistically stimulate rat gastric vagal afferents. American Journal of Physiology, 265, R872–R876.
- Schwartz, G. J., & Moran, T. H. (1998). Duodenal nutrient exposure elicits nutrient specific gut motility and vagal afferent signals in rats. American Journal of Physiology, 274, R1236–R1242.
- Schwartz, G. J., Moran, T. H., White, W. O., & Ladenheim, E. E. (1997). Relationship between gastric motility and gastric vagal afferent responses to CCK and GRP in rats. American Journal of Physiology, 272, R1726–R1733.
- Schwartz, G. J., Solorio, C. F., Skoglund, C., & Moran, T. H. (1999). Gut vagal afferent lesions increase meal size but do not block gastric preload induced feeding suppression. American Journal of Physiology, 276, R1629–R1999.
- Schwartz, G. J., Tougas, G., & Moran, T. H. (1995). Integration of vagal afferent responses to duodenal loads and exogenous CCK. Peptides, 16, 707– 711.
- Schwartz, M. W., Seeley, R. J., Campfield, L.A., Burn, P., & Baskin, D. G. (1996). Identification of targets of leptin action in rat hypothalamus. Journal of Clinical Investigation, 98, 1101–1106.
- Schwartz, M. W., Seeley, R. J., Woods, S. C., Weigle, D. S., Campfield, L. A., Burn, P., & Baskin, D. G. (1997). Leptin increases hypothalamic proopiomelanocortin mRNA expression in the rostral arcuate nucleus. Diabetes, 46, 2119–2123.
- Schwartz, M. W., Sipols, A. J., Marks, J. L., Sanacora, G., White, J. D., Scheurink, A., Kahn, S. E., Baskin, D. G., Woods, S. C., Figlewicz, D. P., & Porte, D. J., Jr. (1992). Inhibition of hypothalamic neuropeptide Y gene expression by insulin. Endocrinology, 130, 3608–3616.
- Sclafani, A. (1991). Conditioned food preferences. Bulletin of the Psychonomic Society, 29, 256–260.
- Scott, T. R., Yan, J., & Rolls, E. T. (1995). Brain mechanisms of satiety and taste in macaques. Neurobiology, 3, 281–292.
- Seeley, R. J., van Dijk, G., Campfield, L. A., Smith, F. J., Burn, , Nelligan, J. A., Baskin, D. G., & Woods, S. C. (1996). Intraventricular leptin reduces food intake and body weight in lean rats but not obese Zucker rats. Hormone and Metabolism Research, 28, 664–668.
- Shintani,M.,Ogawa,Y.,Ebihara,K.,Aizawa-Abe,M.,Miyanaga,F., Takaya, K., Hayashi, T., Inoue, G., Hosada, K., Kojima, M., Kanagawa, K., & Nakao, K. (2001). Ghrelin, an endogenous growth hormone secretagogue, is a novel orexigenic peptide that antagonizes leptin action through the activation of hypothalamic neuropeptideY/Y1 receptor pathway. Diabetes, 50, 227–232.
- Sills, T. L., & Vaccarino, F. J. (1996). Individual differences in sugar consumption following systemic or intraccumbens administration of low doses of amphetamine in deprived rats. Pharmacology, Biochemistry and Behavior, 54, 665–670.
- Simpson, J. B., Epstein, A. N., & Camardo, J. S. (1978). The localization of receptors for the dipsogenic action of angiotensin II in the subfornical organ. Journal of Comparative and Physiological Psychology, 92, 581–608.
- Simpson, J. B., & Routtenberg, A. (1974). Subfornical organ: Acetylcholine application elicits drinking. Brain Research, 79, 157–164.
- Smith, F. J., & Campfield, L. A. (1993). Meal initiation occurs after experimental induction of transient declines in blood glucose. American Journal of Physiology, 265, R1423–R1429.
- Smith, G. P., Jerome, C., & Norgren, R. (1985). Afferent axons in abdominal vagus mediate the satiety effect of cholecystokinin. American Journal of Physiology, 249, R638–R641.
- Stanley, B. G., Kyrkouli, S. E., Lampert, S., & Leibowitz, S. F. (1986). Neuropeptide Y chronically injected into the hypothalamus: A powerful neurochemical inducer of hyperphagia and obesity. Peptides, 7, 1189–1192.
- Stanley, B. G., & Leibowitz, S. F. (1985). Neuropeptide Y injected into the paraventricular hypothalamus: A powerful stimulant of feeding behavior. Proceedings of the National Academy of Sciences, 82, 3940–3943.
- Stanley, B. G., Magdalin, W., Seirafi, A., Thomas, W. J., & Leibowitz, S. F. (1993). The perifornical area: The major focus of a patchily distributed hypothalamic neuropeptide Y sensitive feeding system(s). Brain Research, 604, 304–317.
- Stein, L. J., & Woods, S. C. (1982). Gastrin releasing peptide reduces meal size in rats. Peptides, 3, 833–835.
- Stellar, E. (1954). The physiology of motivation. Psychological Review, 61, 5–22.
- Stricker, E. M. (1968). Some physiological and motivational properties of the hypovolemic stimulus for thirst. Physiology and Behavior, 3, 379–385.
- Stricker, E. M. (1969). Osmoregulation and volume regulation in rats: Inhibition of hypovolemic thirst by water. American Journal of Physiology, 217, 98–105.
- Stuckey, J. A., Gibbs, J., & Smith, G. P. (1985). Neural disconnection of the gut from brain blocks bombesin-induced satiety. Peptides, 6, 1249–1252.
- Sweet, D. C., Levine, A. S., Billington, C. J., & Kotz, C. M. (1999). Feeding responses to central orexins. Brain Research, 821, 535–538.
- Swithers, S. E., & Hall, W. G. (1994). Does oral experience terminate ingestion? Appetite, 23, 113–138.
- Takiguchi, S., Takata, T., Funakoshi, K., Miyasaka, K., Kataoka, K., Fujimura, Y., Goto, T., & Kono, A. (1997). Disrupted cholecystokinin type-A receptor (CCK-AR) gene in OLETF rats. Gene, 197, 169–175.
- Tang, M. (1976). Dependence of polyethylene glycol-induced dipsogenesis of intravascular fluid volume depletion. Physiology and Behavior, 17, 811–816.
- Tartaglia, L. A., Demski, M., Weng, X., Deng, N., Culpepper, J., Devos, R., Richards, G. J., Campfield, L. A., Clarck, F. T., Deeds, J., Muir, C., Sanker, S., Moriarity, A., Moore, K. J., Smutko, J. S., Mays, G. G., Wolfe, E. A., Monroe, C. A., & Tepper, R. I. (1995). Identification and expression of a leptin receptor, OB-R. Cell, 83, 1–20.
- Tschop, M., Smiley, D. L., & Heiman, M. L. (2000). Ghrelin induces adiposity in rodents. Nature, 407, 908–913.
- van Dijk, G., Seeley, R. J., Theile, T. E., Freidman, M. I., Ji, H., Wikinson, C. W., Burn, P., Campfield, L. A., Tenenbaum, R., Baskin, D. G., Woods, S. C., & Schwartz, M. W. (1999). Metabolic, gastrointestinal and CNS neuropeptide effects of brain leptin administration in the rat. American Journal of Physiology, 276, R1425–R1433.
- Weingarten, H. P., & Kulikovsky, O. T. (1989). Taste-to-postingestive consequence conditioning: Is the rise in sham feeding with repeated experience a learning phenomenon? Physiology and Behavior, 45, 471–476.
- Weingarten, H. P., & Watson, S. D. (1982). Sham feeding as a procedure for assessing the influence of diet palatability on food intake. Physiology and Behavior, 28, 401–407.
- Weisinger, R. S., Blair-West, J. R., Burns, P., Denton, D. A., & Tarjan, E. (1997). Role of Brain angiotensin in thirst and sodium appetite of rats. Peptides, 18, 977–984.
- West, D. B., Fey, D., & Woods, S. C. (1984). Cholecystokinin persistently suppresses meal size but not food intake in free feeding rats. American Journal of Physiology, 246, R776–R787.
- Wettendorff, H. (1901). Modifications de sang sous l’influence de la privation d’eau: Contribution a l’etude de la soif. Travaux du Laboratoire de Physiologie, Institut de Physiologie, Instituts, Solvay, 4, 353–384.
- White, J. D., & Kershaw, M. (1989). Increased neuropeptide Y expression following food deprivation. Molecular and Cellular Neuroscience, 1, 41–48.
- Widdowson, P. S., Henderson, L., Pickavance, L., Buckingham, R., Tadayyon, M., Arch, J. R. S., & Williams, G. (1999). Hypothalamic NPY status during positive energy balance and the effects of the NPY antagonist, BW1229U91, on the consumption of highly palatable energy rich diet. Peptides, 20, 367–372.
- Woods, S. C., Lotter, E. C., McKay, L. D., & Porte, D., Jr. (1979). Chronic intracerebroventricular infusion of insulin reduces food intake and body weight in baboons. Nature, 282, 503–505.
- Wren, A. M., Small, C. J., Ward, H. L., Murphey, K. G., Dakin, C. L., Taheri, S., Kennedy, A. R., Roberts, G. H., Morgan, D. G., Ghatei, M. A., & Bloom, S. R. (2000). The novel hypothalamic peptide ghrelin stimulates food intake and growth hormone secretion. Endocrinology, 141, 4325–4328.
- Yaswen, J., Diehl, N., Brennan, M. B., & Hochgeschwender, U. (1999). Obesity in the mouse model of pro-opiomelanocortin deficiency responds to peripheral melanocortin. Nature Medicine, 5, 1066–1070.
- Zarjevski, N., Cusin, I., Vetter, R., Rohner-Jeanrenaud, F., & Jeanrenaud, B. (1993). Chronic intracerebroventricular NPY administration to normal rats mimics hormonal and metabolic changes of obesity. Endocrinology, 133, 1753–1758.
- Zhang, Y., Porcina, R., Maffei, M., Barone, M., Leopold, L., & Freidman, J. M. (1994). Positional cloning of the mouse obese gene and its human homologue. Nature, 372, 425–432.
- Zhou, Q. Y., & Palmiter, R. D. (1995). Dopamine-deficient mice are severely hypoactive, adipsic and aphagic. Cell, 83, 1197– 1209.




